Limb Amputation in Indigenous Australians on Renal Dialysis
advertisement

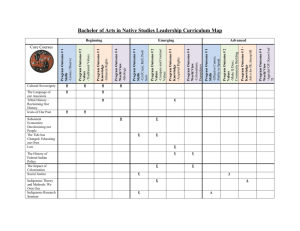
Limb Amputation in Indigenous Australians on Renal Dialysis Dr Rajit Gilhotra RMO, The Royal Brisbane Hospital Diabetes • Diabetes Mellitus (DM) – 7.4% of the adult Australian population – Leading cause of End Stage Renal Failure (ESRF), blindness, Lower Limb Amputations (LLA) and cardiovascular disease (CVD) ) (1 Mellitus Diabetic Foot Syndrome (DFS)(2,3) Diabetic neuropathy Peripheral vascular disease (PVD) Amputation Ischemia prevails End-Stage Renal Failure (ESRF) DM PVD (6-10) Non-healing ulcers LLAs (4,5) Dialysis therapy and foot complications(10-12) – Increased risk of foot ulcers – Amputation is a frequent event – Inconsistent data regarding role of ethnic background Risk further increased with concurrent DM ESRF and LLAs worldwide Study Country Total cases Prevalence DM pts amputated Non-DM pts amputated Speckman et al, 2004 USA 3272 HD 4% 6% 1% LockingCustolito et al, 2005 Canada 232 HD 13.4% 26.53% 3.73% Reddy et al, 2007 USA 271 HD 13% - - Combe et al, Multinationa 29838 HD 2009 l 6% 14.2% 1.6% Ishii et al, 2012 Japan 1513 HD 1.72% 2.8% 0.6% Plantinga et al, 2009 USA 1041 (767 13% HD, 274 PD) - - Australian data • CVD: Indigenous population > non-Indigenous (13) • Major diabetic amputations: Indigenous population 38x > non-Indigenous (14) • Limited data in patients with ESRF (10,15) Impact of amputations • 1 amputation every 3 hours!(16) • $16, 700 per person per year.(1) • Individual: poor QOL, unemployment, comorbidities, chronic pain, prosthesis, death (17,18) Aim 1. To determine prevalence of non-traumatic Amputations in patients on dialysis and document differences between Indigenous and non-Indigenous patients. 2. To determine the association of comorbidities linked with Amputations. 3. To determine the biochemical risk factors associated with Amputations. Study details Population • All patients attending TTH or Northward Dialysis Centre • 219 patient Size Inclusion Exclusion Age>18 Traumatic Amputations HD or PD Neoplastic Amputations Dialysis for at least 1 month DM or nonDM Ethics • Townsville HREC, SSA, PHA • JCU external ethics One off dialysis Data Collection Demographics Clinical History Biochemical Auslab Patient Charts Excel sheet Data analysis Descriptive analysis IBM SPSS Statistics 22 software Univariate analysis - Pearson’s chi squared p<0.05 (Statistically - Student’s t test significant) - Mann-Whitney U test Multivariate analysis - Binary logistic regression Results – patient characteristics Characteristics N (%) Characteristics N (%) n 219 Retinopathy 64 (29.2%) Age (yr) 60.73 (14.48) Neuropathy 61 (27.9%) Male 109 (49.8%) Foot deformity 11 (5%) Indigenous 114 (52.1%) IHD 109 (49.8%) HD 160 (73.1%) CVA 35 (16%) DM Type I 143 (65.3%) 5 (2.3%) HPTN 204 (93.2%) Ulceration 54 (24.7%) Dyslipidaemia 168 (76.7%) PVD 68 (31.1%) Amputation 30 (13.7%) Aim 1: Prevalence of Amputations 30/219 = 13.7% Characteristics N=30 N (%) Characteristics N (%) Male 17 (56.7%) IHD 18 (60%) Indigenous 23 (76.7%) Diabetic nephropathy as cause of ESRF 24 (80%) CVA 6 (20%) DM Type 1 30 (100%) 1 (3.3%) PVD 27 (90%) HD 24 (80%) Retinopathy 19 (63.3%) Major amputation (AKA, BKA, TKA) Previous multiple minor amputations 9 (30%) Neuropathy 24 (80%) 3 (33.33%) Foot deformity 8 (26.7%) HPTN 28 (93.3%) Ulceration Neuro-ischaemic ulcers 27 (90%) 12 (40%) Dyslipidemia 27 (90%) Indigenous vs non-Indigenous Indigenous 20% Non-Indigenous 7% Amputated nonAmputated 80% 93% Amputees Indigenous vs non-Indigenous 120 100 80 % 60 40 20 0 non-Indigenous Indigenous Aim 2: Demographics and comorbidities Association OR [95% CI] Pearson’s Chi Squared with continuity correction Ulceration 81 [18.201 - 360.478] <0.001 PVD 31.285 [9.016 - 108.556] <0.001 Neuropathy 19.719 [7.052 - 55.141] <0.001 Dyslipidemia 4.596 [1.053 – 20.052] 0.049 Indigenous Indigenous background OR 3.39 [1.380.01 – 8.33] p=0.01 3.39 [1.38 – 8.33] Male 1.298 [.592 – 2.846] 0.651 DM present 1.673 [1.488-1.88] <0.001 HD 1.494 [.576-3.874] 0.545 IHD 1.526 [.691-3.369] 0.395 CVA 1.439 [0.539-3.841] 0.647 Retinopathy 6.080 [2.636 – 14.023] <0.001 Foot deformity 23.619 [5.816 – 95.925] <0.001 HPTN 0.997 [0.213 – 4.665] 1 Logistic regression for risk of LLAs B S.E. Wald df Sig. 95% C.I.for EXP(B) Exp(B) Lower Upper Ulceration 2.518 .876 8.271 1 .004 12.408 2.230 69.036 PVD 2.005 .865 5.380 1 .020 7.429 1.364 40.449 Retinopathy .616 .642 .921 1 .337 1.852 .526 Neuropathy .971 .727 1.783 1 .182 2.641 .635 10.991 Foot deformity 2.016 1.005 4.019 1 .045 7.507 1.046 53.863 Dyslipidemia 1.570 1.156 1.844 1 .175 4.808 .498 46.387 Indigenous 1.606 .685 5.490 1 .019 4.98 -1.615 1.030 2.457 1 .117 .199 Constant 1.3 6.515 19.23 Aim 3: Biochemical risk factors Mean five year Vitamin D levels Mean five year Albumin levels Student’s t test* Student’s t test** *p<0.05, **p<0.01, ***p<0.0001 Mean five year Haemoglobin levels Median five year C-reactive protein levels Student’s t test* Mann-Whitney U test** *p<0.05, **p<0.01, ***p<0.0001 Median five year HbA1c levels Mann-Whitney U test** *p<0.05, **p<0.01, ***p<0.0001 Logistic regression for risk of LLAs 95% C.I.for EXP(B) B S.E. Wald df Sig. Exp(B) Lower Upper Vitamin D -.024 .027 .794 1 .373 .976 .926 1.029 Albumin -.405 .186 4.735 1 .030 .667 .463 .961 C-reactive protein -.003 .015 .034 1 .853 .997 .969 1.026 Haemoglobin -.090 .067 1.775 1 .183 .914 .801 1.043 HbA1c 1.078 .397 7.365 1 .007 2.940 1.349 6.406 13.926 8.552 2.652 1 .103 1117069.315 Constant Conclusion 1. Prevalence of Amputations 13.7% 2. Comorbidities and biochemical factors that play major role in development of Amputations: a. Indigenous background b. Ulceration c. Foot deformity d. PVD a. Low serum Albumin (inflammation/poo r nutrition) b. High HbA1c (poor diabetic control) Over-representation of the Indigenous population Townsville population Townsville Dialysis Centre TTH amputations 6% 23% 48% 52% 94% Indigenous 77% non-Indigenous Interesting findings • Low Vitamin D amongst patients with LLAs • Wound healing, T cell function, DFS, PVD, LLAs(19,20,21) • Low Haemoglobin amongst patient with LLAs • Anaemia found to be independent risk factor for limb loss in PVD patients.(22) Impact and relevance • Ability to easily identify at risk population early – – – – – Improved quality of clinical care Foot checks Optimizing biochemistry Reduce hospital and government costs Improve QOL • Further research: – Prospective studies into optimising biochemistry to prevent limb loss. – Effects of Vitamin D supplementation in PVD patients. Acknowledgement • A/Prof Usman Malabu, Department of Diabetes, TTH • Dr Venkat Vangaveti, James Cook University • Data collection: • • • Dr George Kan, Department of Nephrology, TTH Elizabeth Messer, Department of Diabetes, TTH A/Prof David Porter, Department of Pathology, TTH • Guidance: – – – – – – – – Dr Kunwarjit S Sangla Dr Joseph Moxon Beverly Rodrigues Dr Ross Smith Dr Divyajeet Rai Dr Seth Delpachitra Dylan Morris Cedric Hensman Thankyou! Questions? References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. Lazzarini PA, Gurr JM, Rogers JR, Schox A, Bergin SM. Diabetes foot disease: the Cinderella of Australian diabetes management? Journal of foot and ankle research. 2012;5:24. Stiegler H. [Diabetic foot syndrome]. Herz. 2004;29:104-15. Bruhn-Olszewska B, Korzon-Burakowska A, Gabig-Ciminska M, Olszewski P, Wegrzyn A, Jakobkiewicz-Banecka J. Molecular factors involved in the development of diabetic foot syndrome. Acta biochimica Polonica. 2012;59:507-13. Luke RG. Chronic renal failure--a vasculopathic state. The New England journal of medicine. 1998;339:841-3. Port FK. Morbidity and mortality in dialysis patients. Kidney international. 1994;46:1728-37. O'Hare AM, Glidden DV, Fox CS, Hsu CY. High prevalence of peripheral arterial disease in persons with renal insufficiency: results from the National Health and Nutrition Examination Survey 1999-2000. Circulation. 2004;109:320-3. O'Hare AM, Bacchetti P, Segal M, Hsu CY, Johansen KL, Dialysis M, et al. Factors associated with future amputation among patients undergoing hemodialysis: results from the Dialysis Morbidity and Mortality Study Waves 3 and 4. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2003;41:162-70. 11 Jaar BG, Astor BC, Berns JS, Powe NR. Predictors of amputation and survival following lower extremity revascularization in hemodialysis patients. Kidney international. 2004;65:613-20. Margolis DJ, Hofstad O, Feldman HI. Association between renal failure and foot ulcer or lower-extremity amputation in patients with diabetes. Diabetes care. 2008;31:1331-6. Ndip A, Rutter MK, Vileikyte L, Vardhan A, Asari A, Jameel M, et al. Dialysis treatment is an independent risk factor for foot ulceration in patients with diabetes and stage 4 or 5 chronic kidney disease. Diabetes care. 2010;33:1811-6. Combe C, Albert JM, Bragg-Gresham JL, Andreucci VE, Disney A, Fukuhara S, et al. The burden of amputation among hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study (DOPPS). American journal of kidney diseases : the official journal of the National Kidney Foundation. 2009;54:680-92. Nelson RG, et al. Diabetes Care. 1988 Davis TM, et al. Diabetes Care. 2012 Norman PE, et al. Med J Aust. 2010 Goodman WG, Goldin J, Kuizon BD, Yoon C, Gales B, Sider D, et al. Coronary-artery calcification in young adults with end-stage renal disease who are undergoing dialysis. The New England journal of medicine. 2000;342:1478-83. Bergin SM, et al. Med J Aust. 2012 Sinha R, et al. Prosthet Orthot Int. 2011 Tentolouris N, et al. Diabetes Care. 2004 Zubair M, Malik A, Meerza D, Ahmad J. 25-Hydroxyvitamin D [25(OH)D] levels and diabetic foot ulcer: is there any relationship? Diabetes & metabolic syndrome. 2013 Jul-Sep;7(3):148-53. PubMed PMID: 23953180. Chua GT, Chan YC, Cheng SW. Vitamin D status and peripheral arterial disease: evidence so far. Vascular health and risk management. 2011;7:6715. PubMed PMID: 22140318. Pubmed Central PMCID: 3225350. Gaddipati VC, Bailey BA, Kuriacose R, Copeland RJ, Manning T, Peiris AN. The relationship of vitamin D status to cardiovascular risk factors and amputation risk in veterans with peripheral arterial disease. Journal of the American Medical Directors Association. 2011 Jan;12(1):58-61. PubMed PMID: 21194661. Desormais I, Aboyans V, Bura A, Constans J, Cambou JP, Messas E, et al. Anemia, an independent predictive factor for amputation and mortality in patients hospitalized for peripheral artery disease. European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery. 2014 Aug;48(2):202-7. PubMed PMID: 24935912.