Pharmacological Therapy of Heart Failure: Case presentations
advertisement

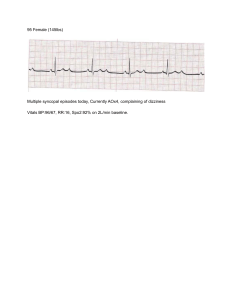
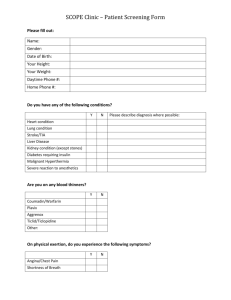
Pharmacological Therapy of Heart Failure: Case presentations Steven W. Harris MHS, PA-C Heart Failure Complex diagnosis that results from structural or functional disorder(s) which impair the ability of the ventricle to fill with or eject blood. – ACC 2005 Epidemiology Prevalence Affects 5+ million Americans currently, >600,000 new cases diagnosed each year. 23 million people worldwide. Estimates are based only on symptomatic HF. Cost Annual direct cost is >10 billion dollars Frequency It is the most common inpatient diagnosis in the US for patients over 65 years of age In 2004, there were over one million hospitalizations in the US with a first listed discharge diagnosis of HF Major Determinants of Cardiac Function Ventricular systolic function Ventricular diastolic function Ventricular preload Ventricular afterload Cardiac rate and conduction Myocardial blood flow Ventricular Systolic Function Systolic dysfunction accounts for 6070% of all cases of HF Ejection fraction decreased 55-65% normal 40-50% mild 30-40% moderate <30% severe systolic dysfunction NYHA Classification Class I - symptoms only at activity levels that would limit normal individuals Class II – symptoms with ordinary exertion (moderate exertion) Class III - symptoms with less than ordinary exertion (minimal exertion) Class IV - symptoms at rest Heart Failure Stages Stage A — High risk for HF, without structural heart disease or symptoms Stage B — Heart disease with asymptomatic left ventricular dysfunction Stage C — Prior or current symptoms of HF Stage D — Advanced heart disease and severely symptomatic or refractory HF Classification of HF severity ACC/AHA HF Stage1 NYHA Functional Class2 A At high risk for heart failure but without structural heart disease or symptoms of heart failure (eg, patients with hypertension or coronary artery disease) B Structural heart disease but without symptoms of heart failure C Structural heart disease with prior or current symptoms of heart failure D Refractory heart failure requiring specialized interventions None I Asymptomatic II Symptomatic with moderate exertion IIISymptomatic with minimal exertion IV Symptomatic at rest SA et al. J Am Coll Cardiol. 2001;38:2101–2113. York Heart Association/Little Brown and Company, 1964. Adapted from: Farrell MH et al. JAMA. 2002;287:890–897. 1Hunt 2New Treatment Objectives Decrease Symptoms Improve tissue perfusion Increase exercise tolerance Quality of/Prolong Life /Survival Correct aggravating/precipitating factors: Endocarditis Arrhythmias Obesity Pregnancy Hypertension Infections Physical activity Hyperthyroidism Dietary excess Thromboembolism Medications Preload Afterload Ionotropy Optimize chonotropy Neurohormonal activity Vicious Cycle Chronic HF Home SOB, Wt gain IV Lasix +/-admit Providers office ER PO Lasix Case 1 76 y/o moderately obese male with a history of CAD with associated CABG x 4, presents to your clinic c/o dyspnea on exertion, 2 pillow orthopnea, bilateral lower extremity edema. Case 1 Meds: Simvastatin 80mg po qhs Synthroid 125 mcg po qd Lisinopril 5 mg po qd Metoprolol 50 mg po qd ASA 81 mg 2 tabs po qd PMH Physical exam: Vitals ?? BP: 146/78 HR: 78 regular RR: 12 bpm T: 98.6 F SPO2: 95% on RA JVD at 5 cm above sternal angle Bilateral rales to mid lung fields 1+ bilat pedal edema Case 1 Plan: Diagnostics: Treatment: Patient Education: Follow-up/ Referrals: Echocardiogram BMP BNP Lasix 20 mg po qd KCL 10 meq po qd f/u in 1 wk Case 2 65 y/o female who is 6 months s/p AWMI c/o 10 lb weight gain over 72 hours. Associtated sx include orthopnea, pnd, dyspnea at rest and abdominal “fullness”. At the time of discharge 6 months prior she had an ischemic cardiomyopathy with an EF of 50% Case 2 Meds: Quit meds ASA 81 mg 1 tab po qd Physical exam: DM HTN Dyslipidemia BP: 130/78 HR: 100 regular RR: 18 bpm T: 98.7 F SPO2: 90% on RA JVD at 10 cm above sternal angle Hepato-Jugular reflux to angle of mandible Bilateral rales 2/3 up 1+ bilat pedal edema PMH Vitals Case 2 Plan: Diagnostics: Treatment: Patient Education: Follow-up/ Referrals: Admit to hospital Echocardiogram CMP, BNP, CBC… Lasix 40 mg IV x 1 Then 40 mg po BID Enalapril 2.5 mg BID Simvastatin 20 mg qhs Morning labs Case 2 Morning Results: Diuresed 3 liters Feeling much better EF 45% BNP 550 Vitals: BP 122/76 HR 78 RR 12 T 98.6 SPO2 98 % on 2 L Plan Plan: Wean O2 Carvedilol 3.125 mg BID Continue Furosemide dose Morning labs Beta blockers Case 3 65 y/o male with known history of prior MI and CABG, ischemic cardiomyopathy with an EF of 30% presents to the ER with dyspnea at rest. He states that over the last week he has gained “at least 10 lbs” and has been sleeping in his armchair. Case 3 Meds: Carveidolol 12.5 mg BID Lisinopril 5 mg qd Atorvastatin 40 mg qhs Furosemide 80 mg qAM ASA 81 mg 1 tab po qd PMH HTN, Dyslipidemia ?? Physical exam: Vitals BP: 110/78 HR: 110 regular RR: 22 bpm T: 98.7 F SPO2: 88% on RA Sitting upright JVD above angle of the mandible Hepato-Jugular reflux to angle of mandible Diffuse bilateral rales 2+ bilat pedal edema Case 3 Plan: Diagnostics: Treatment: Patient Education: Follow-up/ Referrals: Admit to hospital Echocardiogram CMP, BNP, CBC… Bumetanide 1 mg IV then 0.5 gtt KCL repletion 2 gm sodium diet Case 3 Results Diuresed 4 liters Weaned from IV to PO Furosemide 80 mg po qd Cr 1.5 Slowly gaining H2O weight What can you do? Sequential nephron blockade. Addition of aldosterone antagonist Sequential nephron blockade with: Metolazone 2.5 mg po qd Aldosterone antagonist Spironolactone 25 mg daily f/u labs K+ in 3 days and one week. Increased Risk of hyperkalemia if Cr >1.6 Case 3 Consideration of positive inotropes Dobutamine 2-20 mcg/kg/min IV Indications: insufficient cardiac output Effect: Increase Cardiac output and stroke volume Comment: Tachycardia, hypertension, hypotension Dopamine. 2-20 mcg/kg/min IV Indications: Insufficient cardiac output, hypotension, reduced renal perfusion Effect: Increase cardiac output, stroke volume, and renal blood flow Digoxin Digoxin Mildly positive inotropic effects Associated with symptomatic improvement, increase exercise tolerance, and clinical stability Pts taking digoxin are less likely to be hospitalized (25% reduction) due to CHF. Additive benefits to Diuretic, ACE, Beta blocker therapy Case 4 60 y/o male with known history of CAD and prior MI presents to your clinic to establish care. He states that over the last month he has had to double his water pill to keep his legs thin and breathe well at night. His most recent EF was 50% one year ago. Currently he is feeling fine, but has SOB with riding his road bike. Case 4 Meds: Enalapril 20 mg qd Cardizem CD 180 mg qd Atorvastatin 40 mg qhs HCTZ 25 mg 2 tabs po qd ASA 81 mg 1 tab po qd Naproxen 220 mg qd PMH HTN, Dyslipidemia ?? Physical exam: Vitals BP: 118/78 HR: 64 regular RR: 12 bpm T: 98.7 F SPO2: 97% on RA JVD 3 cm above sternal angle Clear lung fields Trace bilateral pedal edema Case 4 Plan: Diagnostics: Treatment: Patient Education: Follow-up/ Referrals: DC Cardizem Start: Carvedilol 6.25 mg BID and uptitrate to 12.5 mg BID in two weeks DC Naproxen Consider acetaminophen BMP to eval K+ Echocardiogram F/u 2 weeks Case 5 80 y/o female c/o of 1 week h/o palpitations and 3 days of SOB and orthopnea Considerations African Americans CRF ACE intolerant