Parasitic Pathogens
advertisement

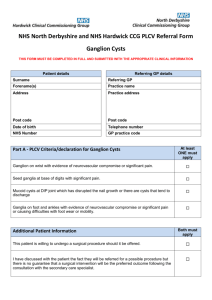
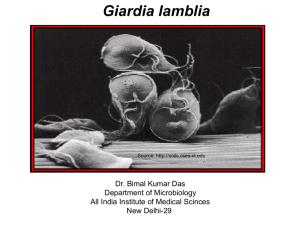
Enteric Parasites Mostly Protozoans ENVR 421 Mark D. Sobsey Enteric Parasites: Taxonomy Protozoans: • Sarcodina: Amoebas: ex.: Entamoeba histolytica • Mastigophora: Flagellates: ex.: Giardia lamblia • Sporozoa: Coccidians: Cryptosporidium parvum • Ciliophora: Ciliates: ex.: Balantidium coli • Microsporidia: ex.: Enterocytozoon beinusi Helminths: • Platyhelminthes: Flatworms: – Cestods (tapeworms) and Trematodes (flukes) • Nemathelminthes (roundworms) Giardia: Description • Human pathogen: G. lamblia or G. intestinalis or G. duodenalis • Many other species: e.g., G. muris (mice) • A flagellated protozoan enteric parasite. • Two life stages: trophozoite and cyst. Giardia lamblia cyst Giardia lamblia cyst G. lamblia trophozoite Life Cycle of Giardia lamblia Giardia Cysts and Trophozoites • Trophozoite is heart (pear) shaped, symmetric and 10-18 um long by 6-8 um wide, 4 pairs of flagella with bilateral symmetry; 2 nuclei with central karyosomes and 2 axistyles. • Large concave sucking disk on anterior ventral surface. • Trophozoites found in upper 1/3rd of small intestine. • When swept into the colon they encyst. • Cysts are 8-14 um long, ellipsoid, contain 2-4 nuclei and have a thick (0.3 um) wall. • Trophs. and cysts are shed in feces; trophs degrade quickly. • Cysts are the persistent environmental form. • Fecal shedding by humans ranges from • 103-108 cysts/gram and by calves 107-108/gram. Clinical Illness and Pathogenesis • Ingested cysts excyst in response to stomach acidity. • Trops. attach (via their sucking disk) to microvilli of epithelium in small intestine, causing epithelial damage and interfering with gut transport processes. • Epithelial mucus is thinned, lymphocytes and other inflammatory cells infiltrate, physical blocking of absorption may occur, and enterobacteria may proliferate, causing more epithelial damage. • Symptoms include profuse and watery to semisolid, greasy, bulky and foul- smelling diarrhea; abdominal cramps; nausea; vomiting; anorexia; low-grade fever and flu-like headache. General malaise, weakness, weight loss, • distention and flatulence can occur. Giardia Illness and Treatment • Symptoms more likely in children and immunosuppressed adults than in healthy adults. • Infectous dose is low (about 10 cysts; possibly less). • Incubation period from 7-11 days. • Duration of illness varies: few days to months. • May resolve spontaneously. Often, subchronic stage develops with mild to moderate symptoms occurring periodically. • Treatment is recommended for symptomatic infections with one of several drugs: Quinacrine HCl (Atabrine), Metronidazole (Flagyl) and Furazolidone (Furoxone). • Oral Quinicrine HCl cures about 90% of infections. Giardia Epidemiology • Fecal-oral route. • One of the most prevalent human parasites in the U.S.A. • Many animals are major reservoirs: dogs, beaver, muskrat, elk, deer, voles, mice, horses and sheep. • Transmission by contaminated water and food is common • Transmission in day-care centers, refugee camps, jails and other crowded facilities with poor hygiene and sanitation. • Levels in sewage are estimated in the range of 3,000 • to 30,000 per liter. • Animal-to-human transmission occurs, but pathogenicity and virulence of non-human sources for humans is still • uncertain. – Strain differences documented both antigenically and genetically. Giardia Detection, Analysis and Environmental Control Detection: • Microscopic detection based on finding distinctive trophs. or cysts in stools, with our without dye staining or immunofluorescent (fluorescent antibody) staining. • Newer clinical diagnostic detection by enzyme immunoassay (EIA; ELISA). • Microscopic detection of cysts in environmental samples. – After prior concentration, purification, staining (immunofluorescent). • Molecular detection by PCR is now being used for detection and characterization. Environmental Control of Giardia Water: physical and chemical treatment (coagulationflocculation, sedimentation, filtration and disinfection) will reduce Giardia by 3+ log10 – 2 to 2.5 log10 by typical physical-chemical treatment – ~0.5 log10 by chemical disinfection (chlorine, ozone or chlorine dioxide) – Extensive >4 log10 reductions by membrane filtration • Sewage: ~99% reductions by conventional 1o+2o sewage treatment – Infectivity of cysts in treated effluent is uncertain • Relatively resistant to chemical disinfection but relatively sensitive to physical disinfection by UV radiation or heat – Pasteurization and thermal treatments effective for foods Cryptosporidium parvum, and Other Cryptosporidium species: Description of the Agents • C. parvum: coccidian protozoan parasite infecting the enteric tract of humans and other animals. • At least two major C. parvum genotypes: “human” and “cattle” • Several other other species: C. muris (mice), C. baileyi and C. melagridis (birds), felis (cats), wrarii, etc. • Complex life cycle; 6 major stages: excystation, merogony (asexual reproduction), gametogony (gamete formation), fertilization, oocyst wall formation and sporogony (sporozoite formation). • Complete cycle in a single host; auro infection occurs. • Oocysts are spherical or oval, 3-7 um in diameter. • A "suture line” sometimes seen spanning the circumference. • Most (80%) oocysts have thick walls; some (20%) have thin walls. • Oocysts contain four sporozoites; infective when excreted. Life Cycle of Cryptosporidium Cryptosporidium Life Cycle • Infection begins from ingested oocysts. • Oocyst wall breaks down in the gut; release sporozoites that go on to form trophozoites. • Trophs. Released in gut attach to the microvilli of the epithelial cells lining the GI tract. • They make intimate association with cell membranes. • Attached trophs. divide their nuclear material 3X to produce the first generation schizont. • Schizonts contain 8 first generation merozoites; schizonts rupture to release their merozoites, which attach to other epithelial cells. • These then round up and form second generation schizonts, each containing four second generation merozoites. • Some second generation merozoites develop into micro- and macro- gametocytes, which combine (sexual reproduction) to form the zygote. • Infective oocysts develop from these zygotes. Cryptosporidiosis in Immunocompetent Hosts • Infection is often subclinical. • Symptoms like giardiasis: watery diarrhea, abdominal cramps, nausea, vomiting, anorexia, fever, malaise and constipation. • In children an additional clinical manifestation is failure to thrive; children are more likely to develop illness than adults. • Incubation period ~7 days • Typical duration of illness is 10 days, with a range of 1-4 weeks. • Pathology occurs most often in the proximal small intestine. Damage to intestinal epithelium is minimal; there is no invasion. • Diarrhea probably results from hypersecretion of fluid and electrolytes and decreased absorption. • Occasionally there is acute inflammation and cellular infiltration. Microvilli may be be blunted or lost at the site of attachment and neighboring microvilli may become elongated. Cryptosporidiosis in Immunocompromized Hosts • Cryptosporidiosis can be life-threatening. • For example, fluid loss in AIDS patients is often 2-6 L per day, reaching 17 L/day. • In some cases extra-intestinal infection occurs; – for example respiratory cryptosporidiosis (interstitial pneumonia) in AIDS patients. • Opportunistic infections can occur, such as Pneumocystis carinii lung invasion in AIDS patients. • Chronic illness can occur in these patients and is complicated by the lack of effective drug therapy. C. parvum Transmission • Infective dose of C. parvum is probably quite low; • As little as 1 cyst is infective for nonhuman primates. • As few as 10 cysts of some strains infect humans – Infectivity varies by strain – 100X difference • Fecal-oral route. • Animal reservoirs; >20 species common in North America: calves, lambs, goats, horses, pigs, deer, squirrel, chipmunk, beaver, muskrat, woodchuck, rabbit, dogs, fox, cat, skunk, • raccon and bear. • Animal to human transmission is thought to be common. C. parvum Epidemiology • Prevalent in children, rate of up to 7% in developed countries and twice that in developing countries. • Overall U.S prevalence ~ 0.3%, but in day care center children it is 6-54%. • Estimated concentration in raw sewage is about 104/L. • Concentrations of 10s to 1000s/L in 2o treated sewage • Oocyst concentrations in fecally contaminated water vary but concentrations of up to 240/L have been reported. • High risk groups are day care center children and their adult • contacts, travellers, health care workers, animal workers and AIDS patients. • Waterborne and foodborne transmission is documented. Cryptosporidium Detection • Similar to that of Giardia. • In feces: by staining and microscopic examination of fecal smears with or without flotations for partial purification. • For water, recover by filtration, extract from filters, centrifuge and float in density solutions (or use immunomagnetic separation) . • Stain with fluorescent antibody and examine microscopically. – IMS and fluorescent antibody staining have greatly improved detection because oocysts are very similar in size and shape to algae, yeasts and fungi spores. • As for Giardia, a major limitation of detection methods is determination of viability. • How do you know a cyst or oocyst is viable/infectious by looking at it? • New infectivity detection in cell culture • New molecular methods for detection and characterization Prevention and Control of Cryptosporidiosis • No effective chemotherapy; no effective vaccine • Control in water treatment by conventional processes – about 2 log10 reduction by coagulation-flocculation and filtration – >4 log10 reduction by membrane filtration – not inactivated by free chlorine or chloramine at practical doses – inactivated by moderate doses of ozone and chlorine dioxide – inactivated by low doses of UV radiation – treatment process reliability is essential to prevent breakthrough • Milwaukee outbreak of 1993 (>400, cases) partly due to unreliable treatment • About 2 log10 reduction by conventional sewage treatment • Control in foods by thermal treatment and in beverage by UV • Hygiene and sanitation are important controls measures in high-risk settings, such as day-care facilities, prisons, etc. Entamoeba histolytica and Amoebic Dysentery • A typical ameba; moves by pseudopod extension • two life stages: – actively motile, feeding trophozoite (12-50 um) and – quiescent, resistant, infective cyst (10-20 um); • formed from trophs. when environmental conditions are unfavorable. • Reproduce by binary fission of trophozoite or development of several (up to 4) trophs. within the mature, miltinucleated cyst. Life Cycle of Entamoeba histolytica Life Cycle and Process of Infection of E. histolytica • • • • • • • • • ingestion of mature cysts(1) in fecally contaminated food, water, etc. Excystation (2) occurs in the small intestine Trophozoites (3) are released, which migrate to the large intestine. Trophozoites multiply by binary fission and produce cysts (4) , which are passed in the feces. Often, trophozoites remain in intestinal lumen (A: non-invasive infection) – individuals are asymptomatic carriers and cysts passers. In some hosts trophs. invade the intestinal mucosa (B:intestinal disease). Via bloodstream they can invade extraintestinal sites such as the liver, brain, and lungs (C: extra-intestinal disease), with resultant pathology. Invasive and noninvasive forms represent separate species, respectively E. histolytica and E. dispar, which are morphologically indistinguishable. Transmission also occurs via fecal exposure during sexual contact (in which case not only cysts, but also trophozoites could be infective). E. histolytica trophozoites and cysts (Ingested red blood cells) Right: E. histolytica trophozoites (trichrome stain) Right: E. histolytica cysts iodine (L); trichrome (R) E. histolytica: appearance of trophozoites and cysts • Stained trophozoites display a granular nucleus containing a small dense mass of chromatin (called a karyosome) in the center. • Trops. can ingest red blood cells; often visible in the endoplasm. • Diagnosis of infection is by detection of characteristic cysts (or trophs.) in feces or infected tissue. • Cysts are formed from trophs. as they move down the colon • Mature cysts contain 4 nuclei (from two successive nuclear divisions) and perhaps several chromatoidal bars, which are aggregates of ribosomes in the cytoplasm E. histolytica illnesses • When trops. divide and invade the intestinal epithelium, they produce areas necrosis in the large intestine • Cause mild GI symptoms (abdominal pain, cramps, • colitis and diarrhea) are produced; a cytotoxin is made. • If necrosis becomes worse, areas of invasion ulcerate, coalesce and hemmorrhage and secondary bacterial invasion occurs. • Diarrhea with blood and mucus in the numerous stools produced indicates severe amoebic dysentery. • If trophs. invade peritoneum, they can spread to liver and even lungs to produce painful hepatic and bronchial abcesses. • Treatment is by administration of one of several drugs: dehydroemetine,diiodohydroxyquin, chloroquine or metronidazole. Epidemiology and Control • Transmission by fecal-oral route; humans the only hosts. • Most infections are inapparent (asymptomatic; subclinical) • Adequate sanitation and excreta disposal and provision of nonfecally contaminated water and food will control. • In developed countries like the U.S., most cases occur in settings where sanitation is poor – or among male homosexuals (via oral-anal sex) • Some outbreaks due to fecally contaminated water and food. • 1-2% prevalence. • High risk settings: institutions with poor sanitation: mental facilities, military and refugee camps, prisons, day-care centers. • In developing countries, esp. in tropics and subtropics, prevalence is 10-15% and sometimes up to 50-80%. – Many inapparent infections in which hosts shed large numbers of cysts.