University of Washington
advertisement

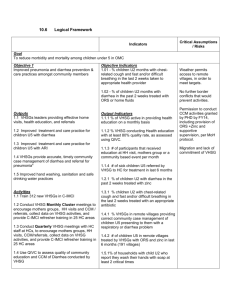
e-IMCI: Improving Pediatric Health Care in Low-Income Countries Brian DeRenzi Quals Talk November 19, 2007 University of Washington e-IMCI Project PDA-based decision support for clinicians at the point of care Increase quality of care delivered Result Significantly increased adherence to medical protocol without substantially increasing patient visit time Contribution Adapted code base to implement the protocol for pediatric health care Ran two-month field study in rural Tanzania to pilot the Outline Motivation Introduction Background on Project Integrated Management of Childhood Illness (IMCI) e-IMCI Field Study Results Future work Acknowledgements Motivation This year almost 10 million children will die before reaching the age of 5 Most live in low-income countries 10% of infants die during their first year, compared to 0.5% in wealthy countries Almost 2/3 could be saved by the correct application of affordable interventions Motivation Every 6 seconds a child dies unnecessarily Introduction UNICEF, WHO and others develop medical protocols e.g. Integrated Management of Childhood Illness (IMCI) Clinical guidelines for busy facilities Easy to use for lowly-trained health workers Introduction - IMCI Originally developed in 1992 Adopted by over 80 countries worldwide Children 0-5 years old Common illness Cough Diarrhea Fever Ear Pain Malnutrition IMCI IMCI Barriers Expense of training ($1150 -$1450) Not sufficient supervision Chart booklet Takes a long time to use Natural tendency to be less rigorous Social pressure Result - not often followed in health clinics Related Work Automating procedural tasks Harvard University Program on AIDs (HUPA) Project Designing medical protocol in South Africa Decision support in India TRACNet, OpenMRS, IHRDC study Gary Marsden Computable protocols Using mobile devices can help under high workloads GLIF Artificial Intelligence e-IMCI Put IMCI protocol on PDA Guide health workers step-by-step Potential benefits Better adherence to protocol Easier and faster than book Data collection is a by-product of care Can handle more complex protocols Interface with other devices and EMR Reduce training time and cost Strong supervision Background How the project started and how I got involved. D-Tree International Medical algorithms on mobile devices Help over-burdened health workers Gather data from the field Work with governments to implement sustainable programs HUPA project HUPA Project Started in Cape Town HIV screening algorithm Counselors can quickly determine if patient needs to see doctor Huge shortage of doctors 29.1% national HIV prevalence1 Less than 1% in US 1 http://www.avert.org/safricastats.htm South Africa Worked with Right To Care Non-profit at Helen Joseph Hospital Second site for HUPA project Gained experience with the HUPA code Delivered PDAs, established workflow Introduced to health facilities and field work South Africa Tanzania Worked with IHRDC Met with the Tanzanian government and other NGOs IMCI Integrated Management of Childhood Illness. IMCI Example IMCI Example IMCI Example IMCI Example IMCI Example e-IMCI Electronic delivery of IMCI. e-IMCI Interface e-IMCI Implemented subset of IMCI protocol for pilot study Contains cough, diarrhea, fever and ear pain questions and treatment First visit, ages 2 weeks to 5 years Field Study Real clinicians. Real patients. Real world. Mtwara, Tanzania Worked with IHRDC in Mtwara, Tanzania Southern Tanzania Rural Subsistence farming Fishing Piloted e-IMCI at a dispensary Study Design Started with five clinicians Four clinicians completed study Goals: Discover usability issues Discover if e-IMCI increases adherence Determine how e-IMCI affects patient visit IMCI Protocol Use Ideal case “Current practice” Follow paper chart booklet for every patient between 0-5 years of age Treat patients from memory, occasionally referencing the chart booklet e-IMCI trials Treat patients using the e-IMCI software system Study Design Started with some pretrials to fix major bugs Semi-structured interview of all clinicians Observed 24 “current practice” IMCI sessions 27 e-IMCI sessions Exit interview for each clinician Study Design Real Patients, not actors Used same data collection forms for current practice and eIMCI Pairwise design Basic pilot, no randomization Trials per Clinician Clinician 1 2 3 4 5 Number of “current practice” trials 5 5 5 5 4 Number of e-IMCI trials - 6 4 4 13 Results Numbers, reactions and lessons. Adherence Measured adherence using 23 items IMCI asks the practitioner to perform e-IMCI significantly improved adherence to the IMCI protocol p < 0.01 p < 0.01 Adherence: The Numbers Investigation Current Practice Adherence e-IMCI Adherence p-value Vomiting 66.7% (n=24) 85.7% (n=28) - Chest Indrawing 75% (n=20) 94.4% (n=18) - Blood in Stool 71.4% (n=7) 100% (n=3) - Measles in Last 55.6% (n=9) 3 Months 95.2% (n=21) <0.05 Tender Ear 0% (n=1) 100% (n=5) - All 61% (n=299) 84.7% (n=359) < 0.01 Adherence: Advice Numbers Clinical Officer Current Practice e-IMCI Advice Adherence Adherence p-value 1 20% (n=15) 76.9% (n=39) < 0.01 3 26.7% (n=15) 66.7% (n=18) < 0.05 4 80% (n=15) 100% (n=12) - 5 100% (n=12) 73.3% (n=21) - All 56.9% (n=72) 77.4% (n=84) < 0.01 Timing No substantial increase in patient visit time Clinical Officer Average Length of Current Practice Patient Visit (minutes) Average Length of eIMCI Patient Visit (minutes) 95% Confidence Interval of e-IMCI Minus Current Practice 1 16 (n=5) 13 (n=13) -2.1 to 7.9 † 3 6 (n=5) 8 (n=6) -5.5 to 1.0 † 4 7 (n=5) 9 (n=4) -5.7 to 4.7 † 5 19 (n=4) 14 (n=4) -2.1 to 13.1 † Total 10 (n=24) 11 (n=27) -2.4 to 2.4 ‡ † unpaired t-test, ‡ paired t-test of 18 trials Clinician Reaction Unanimously cited e-IMCI as easier to use and faster than following the chart booklet Clinician Reaction Wanted to use the system for Care Treatment Clinic Liked being able to review answers to questions Asked to be in future studies “Sometimes since I have experience [with IMCI] I will skip things, but with the PDA I can’t skip.” Would “use a combination” of current practice and the e-IMCI software and would never need to refer to the book Lessons Learned Limitations Question Grouping Threshold Problem Requirements Incorrect IMCI Flexibility otitis externa Local Preference Antibiotic Lab use Conclusion e-IMCI significantly improves adherence to IMCI protocol Does not substantially lengthen the patient visit time Positive reaction from clinicians, but room for improvement Large number of interesting enhancements for the future Future Work Where we’re going. e-IMCI for Training Current training lasts 11-16 days Costs $1150 - $1450 per person Using e-IMCI to train, could reduce time and cost No need to train the protocol as in-depth Tutored mode User-Driven Model “Expert” mode Allow users to decide what investigations to perform Flexibility will encourage long-term use Merge with current system-driven approach to ensure correct care Deploying Protocols Interfaces for tutor, guided and expert modes Automatically generate interfaces for different platforms Maintain consistent look and feel Community Outreach Take e-IMCI outside of the health facility Travel village-to-village to collect health census information and deliver care Acknowledgments Neal Lesh, Marc Mitchell, Gaetano Borriello, Tapan Parikh, Clayton Sims, Werner Maokola, Mwajuma Chemba, Yuna Hamisi, David Schellenberg, Kate Wolf, Victoria DeMenil, D-Tree International, Dimagi Inc., the Ifakara Health Research & Development Centre, the Ministry of Health in Tanzania and the clinicians in Mtwara for their support and contribution to this work. Questions Extra Slides Just in case. Introduction The vision. Related Work What others have done. IMCI in Tanzania Adapted and adopted by Tanzania in 1996 National policy Main component is a medical protocol followed by health workers at the point of care Pre-Grad School Volunteered with American Red Cross after Hurricane Katrina Volunteered with International Service Learning to deliver medical supplies in rural Tanzania Introduction Digitize protocol to make it easier to use