Vital Bleaching
advertisement

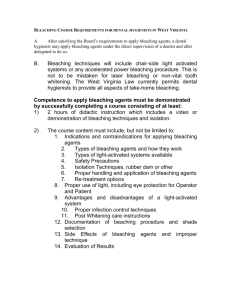
Vital Bleaching Dr. Ignatius Lee Potential Results Vital Bleaching Modern era of vital bleaching began with Haywood and Heymann’s 1989 article on nightguard vital bleaching - using a custom fitted plastic mouthguard to apply a 10% carbamide peroxide gel. Today there are 3 major methods for vital bleaching » In office or power bleaching » At home or tray bleaching » Over the counter In-office/Power Bleaching 25% to 38% hydrogen peroxide Involve chair time; thus most expensive Results most predictable Good for non-compliant or unwilling patients, also for patients demanding instant result At Home or Tray Bleaching 10% to 22% carbamide peroxide (10%=3.6% hydrogen peroxide); 6% to 10% hydrogen peroxide Typically will attain optimal results in 2-6 weeks Results are dose/time dependent Over the Counter Bleaching 6% to 14% hydrogen peroxide Strips, wraps, paint on products Least expensive Results least predictable Vital Bleaching Advantages Low cost High success rate No tooth alternation Vital Bleaching Disadvantages Unpredictable results Need Re-treatment Possible side effects Contraindications When the extrinsic stain can be removed by a thorough prophylaxis Dental caries Discolored restoration Restoration showing through Vital Bleaching Mechanism The active ingredient is hydrogen peroxide, an oxidizing agent It diffuses through the organic matrix of enamel and dentin Produces free radicals, which are responsible for the bleaching process (oxidation) These free radicals open the highly pigmented carbon rings and converting them into chains, which are lighter in color Etiology of Tooth Discoloration Extrinsic Stain » superficial changes » secondary to colored food, drinks (tea, coffee, cola), tobacco products, smokeless tobacco » more of a problem if there are microcracks Aged Related Color Change » thinned enamel » darkened dentin due to deposition of secondary dentin, more yellowish Etiology of Tooth Discoloration Intrinsic Stain » medication given systemically, e.g. tetracyclin, minocyclin » fluorosis » systemic conditions, e.g. jaundice, erythroblastosis fetalis, porphyria » dental caries » old restorations showing through, e.g. amalgam » trauma » heredity Prognosis Discoloration due to aging, inherited discoloration, smoking, chromogenic materials, trauma (evenly distributed discoloration) EXCELLENT PROGNOSIS Works better in removing yellow, orange and light musky brown color Dark blue-gray stain do not response as well Prognosis Brown fluorosis discoloration » good prognosis, may need micro-abrasion and at home bleaching White spot » not removed, only get lighter during treatment Tetracyclin stain » do not typically response well » may need multiple in-office application, extended take home application (2 to 6 months) or combination Prognosis Uneven pulp size » uneven results; smaller pulp slower to lighten or do not lighten as much Initial color relapse » due to oxygen trapped in tooth diffuses out of tooth Longevity of color change » one to three years, individual variations Non-responsive teeth » extend treatment time or use in-office bleaching as a booster Effects on Restorative Materials Composite » minimal changes in color, surface roughness and physical properties » may increase microleakage at CEJ with earilier generation of dentin bonding system » effect unknown on the current generation of bonding system Amalgam » in one invitro study, the amount of mercury released into the peroxide solution was significantly higher than released into saline solution (4-30x) Effects on Restorative Materials Ceramic » no effects on the color or physical properties Luting cements » an intro study showed that glass ionomer, and particularly zinc phoshpate dissolved readily in 10% carbamide peroxide » clinical significance not known Effects on Restorative Materials Temporary restorations » causes microscropic surface change in IRM (Intermediate Restorative Material, a eugenol based temporary material) in both hydrogen peroxide and carbamide peroxide » macroscropically, IRM appears cracked and swollen when exposed to hydrogen peroxide but not carbamide peroxide » metharcylate discolored when exposed to carbamide peroxide » causes no color change in polycarbonate crown and composite-type temporary Effects on Restorations Defective restoration » should consider repairing defects before bleaching to prevent unwanted penetration of the bleaching agent through open margin » should consider temporary repair instead of replacing the restoration because of color match concern Composite / Bonding » delay any bonding or composite procedure for at least one week following bleaching » rationale: lower bond strength and allow for better color match due to regression of bleaching result Effects on Pulp Application of peroxide gel resulted in rapid penetration of peroxide to the pulp chamber. Minor irritation of the pulp tissue did occur, but that it was resolved within 2 weeks after cessation of treatment. No differences between whitened and unwhitened teeth on their responses to electric or cold pulp tests (up to 12 years following bleaching). No evidence of irreversible pulpitis even in extended treatment regimen (more than 6 months). Effects on Enamel Lower enamel microhardness (3% to 7%) immediately after treatment Slight increase in surface porosity as observed under SEM. More surface dissolution by phosphoric acid Safety Issues Sensitivity to Temperature Change » Primary side effect associated with vital bleaching. » Typically begins early in the bleaching process (1st or 2nd day); increased during the course of the treatment. » Usually mild and transient in nature. » Adding potassium nitrate and sodium fluoride to the formulation results in significant reduction in sensitivity as reported by the patients. Safety Issues Sensitivity to Temperature Change » Reported incidence of sensitivity from 7% to as high as 75% » Of those who experienced sensitivity; over 70% are labeled as mild and less than 10% are labeled as severe. » Up to 20% of placebo group experienced sensitivity (due to tray or glycerin) » Predictors of sensitivity: history of tooth sensitivity and treatment frequency (more 1x/day) and dose (concentration and time) » Non-predictors: age, gender, exposed dentin/cementum, cracks, pulp size, caries Safety Issues Sensitivity to Temperature Change Remedy » Reduce wear time or frequency of application » Utilize a lower concentration of peroxide » Immediate removal (in-office) or refrain from using for a couple days » Utilize a product that contain fluoride and or sodium nitrate Safety Issues Irritation of gingiva » due to improper isolation (leaking rubber dam) or excess bleaching agent (patient sensitive to bleaching agent or poor fitting nightguard) » poor fitting or improperly trimmed nightguard » immediate removal (in-office) or for 2-3 days » reduction of wearing time, remake nightguard Not recommended for pregnant or lactating woman Safety Issues Carcinogenic effect » potentiate the effect of a known carcinogen associate with tobacco products (DMBA) » special warning for smokers; refrain Ingestion » not a major problem » taste and laxative effect from the glycerine base Allergy » peroxide, nightguard material Safety Issues Excessive free radicals Low level: may contribute to aging. Moderate level: oxidation damage to DNA occurs, thus possibly leading to mutations and possible carcinogenic. High level: death JADA 135:319 6.6% HCl + silicon carbide microparticles (Opalustre) JADA 134:1066 18% HCl (PREMA) Clinical Case 16 y.o. male Discoloration due to fluorosis Opalustra (6.6% HCl + silicon carbide microparticles) - 4 x 60 sec Followed by Opalesence Xtra Boost (38% hydrogen peroxide) - 2 x 20 min First session Before After Second Session Before After In-office Bleaching (Clinical Protocol) Clean teeth with pumics Record pre-op shade Isolate teeth as close to the gingival margin as possible with rubber dam (no tears, leakage, fully inverted) In-office Bleaching (Clinical Protocol) Mix the thickening agent (Cab-o-Sil) with 35% hydrogen peroxide to a non-slumping consistency. Place the gel material on the teeth for 30 min In-office Bleaching (Clinical Protocol) May need to “refresh” with hydrogen peroxide liquid if the gel appear too dry Rinse and clean; remove rubber dam and record post-op shade Nightguard Bleaching (Laboratory Procedure for Tray) Trim cast to ideal thickness for use in vacuum former » base of cast parallel to occulsal plane, and 45mm from gingival margin (result in good adaptation of tray material) Nightguard Bleaching (Laboratory Procedure for Tray) Make tray using vacuum former Nightguard Bleaching (Laboratory Procedure for Tray) Trim tray using #25 Bard-Parker blade » trim to gingival margin; scallop around interdental papilla Smooth edges using alcohol torch Nightguard Bleaching Clinical Protocol Nightguard Bleaching Clinical Protocol Nightguard Bleaching Opalescence - sustained release How to deal with patient’s expectation Bleaching is an inexact science Results depends on dentist’s skill, individual variation in the teeth, and the patient’s continuing habits , diet and hygiene care Difficult to guarantee results Keys to avoid problem » ensure that patient understand the limitations and what is involved in keeping the enhanced look for as long as possible » document patient’s appearance before treatment (intraoral camera, photo, shade guide, reference pt)