CRE Education Template
advertisement

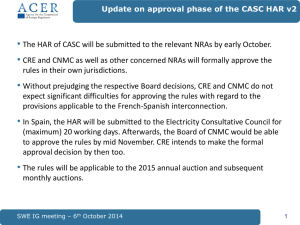
Carbapenem-resistant Enterobacteriacea (ent-ə-rō-ˌbak-ˌtir-ē-ˈā-sē-ˌā) July 2013 http://www.forvo.com/word/enterobacteriaceae/ Outline • Background • Epidemiology • Control 2 What are Enterobacteriaceae? • Family of Gram negative bacteria – Normal part of the human gut bacteria – Common causes of community and healthcare-associated infections (HAIs) – Most common are E. coli and Klebsiella species • E. coli is the most common cause of outpatient urinary tract infections. • E. coli and Klebsiella species (especially K. pneumoniae) are important causes of HAIs. – Together, they accounted for 15% of all HAIs reported to the CDC’s National Healthcare Safety Network (NHSN) in 2007. 4 Why have Enterobacteriacae become an issue? • Some of these kinds of bacteria have become resistant to most antibiotics. They are called Carbapenem-resistant Enterobacteriaceae or “CRE” • Infections with CRE germs are very difficult to treat and can be deadly—one report cites they can contribute to death in up to 50% of patients who become infected. (CDC) • Beta-lactam class carbapenem antibiotics (antibiotics that have been developed from penicillin) have been mainstay of treatment for years • However, resistance to carbapenem antibiotics emerged several years ago and has continued to increase steeply. – Extended spectrum β-lactamase producing Enterobacteriaceae (ESBLs) – Plasmid-mediated AmpC-type enzymes 5 The Last Line of Defense • Fortunately, our most potent β-lactam class carbapenems remained effective against almost all Enterobacteriaceae...until recently… Doripenem, Ertapenem, Imipenem, Meropenem • Unfortunately, “Antimicrobial resistance follows antimicrobial use as surely as night follows day” ~John Jernigan 6 How bad is it? Map showing states where CRE has been identified by the CDC. First case in U.S. showed up in NC in 2001 ! How bad is it? • About 4% of U.S. hospitals had at least one patient with a CRE infection during the first-half of 2012. • About 18% of long-term acute care hospitals had one during this same timeframe. • CRE germs kill up to half of patients who get bloodstream infections from them. • Untreatable and hard-to-treat infections from CRE germs are on the rise among patients in medical facilities. • CRE germs have become resistant to all or nearly all the antibiotics we have today. Carbapenem resistance in K. pneumoniae HAIs -NHSN Time CLABSI CAUTI VAP 2007-2008 11% 9% 4% 2009-2010 12.5% 12.8% 11.2% SSI 7.9 A Klebsiella spp. was identified as the pathogen associated with 8% of CLABSIs, 11% of CAUTIs, 10% of VAPs and 4% of SSIs in 2009-2010 Sievert et al. Infect Control Hosp Epidemiol 2013;34(1):1-14 Hidron, A et al Infect Control Hospital Epidemiol. 2008;29:996 8 CRE are epidemiologically important: • CRE are associated with high mortality rates (up to 50% in some studies). • In addition to β-lactam/carbapenem resistance, CRE often carry genes that have high levels of resistance to many other antimicrobial drugs, often leaving very limited treatment options. • CRE have spread throughout many parts of the U.S. and have the potential to spread more widely. • The emergence and spread of carbapenem resistance among Enterobacteriaceae in the United States represent a serious threat to public health. How are CRE spread? • To get a CRE infection, a person must be exposed to CRE germs. • CRE germs are usually spread person-to-person through contact with infected or colonized people, particularly contact with wounds or stool. • CRE can cause infections when they enter the body, often through medical devices like ventilators, intravenous catheters, urinary catheters, or wounds caused by injury or surgery. Who is most likely to get a CRE infection? • Patients who have been in a healthcare facility for a long time (longer length-of-stay) • Patients with long-term care facility (LTCF) exposure • Patients who have been in ICU • Patients who have received antibiotics – – – – Carbapenems Cephalosporins Fluoroquinolones Vancomycin • Organ or stem cell transplant patients • Patients with invasive medical devices such as Foley catheters, central lines, G-tubes, ventilators, etc. • Healthy people usually don’t get CRE infections. Patel et al. ICHE 2008; 29:1099-106 Schwaber et al. Antimicrob Agents Cehmother 2008; 52:1028-33 Hussein et al. ICHE 2009; 30:666-71 11 Risk Factors for Getting CRE Infections • Comorbidities: – Diabetes – Heart disease – HIV – Renal disease – Liver disease – Transplant • Healthcare-associated factors: – Presence of medical devices (Foleys, central lines, ventilators, G-tube, tracheostomy, etc.) – Being in ICU – Prior and/or current antibiotics – History of MDRO – Decubitus ulcer – Lower Braden Scale score Prabaker et al. Infect Control Hosp Epidemiol 2012;33(12):1193-1199 Prior Antibiotics Increase Risk of CRE CRKP (n=99) CSKP (n=99) p-value Cephalosporins 63 31 p<0.001 Fluoroquinolones 36 23 p=0.05 B-lactam/inhibitor 54 33 p=0.005 Aminoglycosides 14 3 p=0.01 Carbapenems 54* 6 p<0.001 • *26 (48%) on carbapenems at time of isolation of CRKP • *37 (69%) either on carbapenems or completed a course of carbapenems within 2 weeks prior to CRKP isolation Patel et al. Infect Control Hosp Epidemiol 2008;29:1099-1106 13 Can CRE be treated? • Many people with CRE will have the germ in or on their body without it producing an infection. These people are said to be colonized with CRE, and they do not need antibiotics for the CRE. • If the CRE are causing an infection, the antibiotics that will work against it are limited but some options are often available. • Some infections might be able to be treated with other therapies, like draining the infection. • Strains that have been resistant to all antibiotics are very rare but have been reported. Control of CRE • CRE can be spread from patients that are infected or colonized. • To prevent CRE spread, there are several important things to do, called “prevention strategies”. • These prevention strategies apply to all patients with CRE, whether they are infected or colonized. 16 CDC Toolkit – An Important Resource • http://www.cdc.gov/hai/organisms/cre/cretoolkit/ 17 CRE Control: No Magic Bullet but some Core Prevention Strategies from the CDC 1. 2. 3. 4. 5. 6. 7. 8. Lab identification/surveillance Education Hand hygiene Contact Precautions with strict PPE compliance Patient and staff cohorting Limiting use of invasive devices Surveillance screening Antimicrobial stewardship http://www.cdc.gov/HAI/organisms/cre/index.html 18 Laboratory Notification • <Provide your facility’s process for how and when lab notifies IP, unit, and/or physician about CRE.> • <List steps to be taken by each group when lab notifies them (e.g. place patient on Contact Precautions, etc.)> Surveillance • <Insert facility CRE surveillance plan/protocol(s)> Education Staff in all settings who care for patients with MDROs, including CRE, should be educated about preventing transmission of these organisms. At a minimum this should include: – Proper use of Contact Precautions – Hand hygiene Don’t forget physicians, PAs, NPs, phlebotomists, OT/PT, RT, transport personnel, EMT, housekeeping staff, etc. AND – don’t forget the patient and visitors! Hand Hygiene • Strict hand hygiene by everyone is critical! • Hand washing and use of alcohol hand rubs are both effective with CRE. • MONITOR hand hygiene compliance to make sure it’s being done and report back to staff on a regular basis. • Immediate feedback should be provided to anyone who misses opportunities for hand hygiene. • Ensure access to adequate hand hygiene stations (e.g., clean sinks and/or alcohol-based hand rubs) and ensure they are well stocked with supplies (e.g. towels, soap, etc.) and clear of clutter. • Don’t forget to teach the patient and visitors about the importance of hand hygiene and make sure they can get to a sink/hand rub dispenser. 22 Contact Precautions <Place your CP sign here> 23 • <When to implement CP on CRE patients – include patients that are colonized as well as infected> • <Length of time patient should be on CP per your facility policy on CRE> • <How patients may be removed from CP> Contact Precautions – Minimum Requirements for <Your Facility> • Perform hand hygiene <when and how per facility policy> • Don gown and gloves <when> • Remove the gown and gloves and perform hand hygiene prior to exiting the affected patient’s room • <Include short tutorial on proper donning and removal of PPE> <Tip to presenter: Consider fun ways to teach PPE application, such as having a volunteer don PPE properly, dip hands in chocolate pudding, and remove w/o getting pudding where it should not be. (Pudding is a visual surrogate for germs.)> ?Preemptive Contact Precautions? • <If you preemptively place patients at high risk for CRE on CP, populate this slide. If not, delete it.> Patient and Staff Cohorting • Patient cohorting in dedicated wards or areas – Dedicated Staff – Dedicated Equipment • Healthcare provider and patient education key!!! • <Facility-specific instructions for cohorting here> 26 Removal of Invasive Devices • 1/3 of all HAIs are device related • Urinary Catheters – 25% of patients with Foley > 7days develop CAUTI – CAUTI risk increases 5% every day of catheter use • Central Lines – Central venous catheter – Pulmonary artery (Swan-Ganz) catheter – PICCs • Routine review of device necessity should be carried out and device should be removed promptly once no longer clinically indicated <Describe facility-specific device review protocol(s) here> 27 CRE Screening • Used to: – Evaluate prevalence – Determine if transmission has occurred between patients – Identify unrecognized CRE colonization in patients epidemiologically linked to patients w/known CRE • Stool, rectal or peri-rectal swabbing is done or cultures of wounds or urine if they are indicated Antimicrobial Stewardship <Phrase as appropriate to your facility> An antibiotic stewardship program is in place to oversee best antimicrobial practices such as: • Antimicrobials are used for appropriate indications and duration • The most narrow-spectrum antimicrobial that is appropriate for the clinical situation is used http://www.cdc.gov/getsmart/healthcare/ Additional Consideration: Role of Environment Hygiene, hands, patient, and environment are closely interrelated because contamination of any one of these may easily and quickly result in contamination of the others. Role of the Environment "There is no doubt in my mind that contamination of the environment (surfaces in patient care areas and medical equipment) play a major role in the transmission of potential pathogens. There are well-designed studies which show patients who occupy the bed of a patient previously infected with a resistant pathogen are at greater risk of acquiring that pathogen.” ~ Michael Phillips, MD, hospital epidemiologist at New York University, Langone Medical Center Pyrek K. Communicating the importance of environmental hygiene to healthcare workers. Inf Cntrl Today. July 14, 2011. http://www.infectioncontroltoday.com/articles/2011/07/communicating-theimportance-of-environmental-hygiene-to-healthcare-workers.aspx 31 CRE Environmental Contamination Study • 34 known CRE carriers’ environment sampled by contact plate, environmental swab and environmental swab w/ enrichment. CRE was found on surfaces as follows – – – – – Pillow: 68/204 (33%) Patient’s crotch: 63/202 (31%) Patient’s legs 46/198 (23%) Infusion pump 19/120 (16%) Personal bedside table 28/204 (14%) • Overall CRE detected in surroundings of 88% of patients – Detection rate decreased with increased distance from pt • Sampling done before and 4h after clothing/sheet replacement – 27% pre – 21% post Lerner et al. J Clin Microbiol. 2013, 51:177-181 32 Survival of Pathogens on Inanimate Surfaces Pathogen Survival MRSA 7 days – 7 months VRE 5 days – 4 months Acinetobacter 3 days -5 months C. difficile (spores) 5 months Norovirus 12 – 28 days E. coli 2 hours – 16 months Klebsiella spp. 2 hours to > 30months Kramer A, et al (2006). BMC Infect Dis; 6:130 Environment-to-Hand-to-Patient Stiefel U, et al. ICHE 2011;32:185-187 40% 45% Germs can be transferred from surfaces to healthcare worker hands without direct patient contact! Environmental Cleaning • <Fill in facility protocol for environmental cleaning when patient has a MDRO> • Monitoring and Feedback 35 Supplemental Measures Supplemental Measures useful when core measures do not achieve desired results: • Active surveillance testing: culturing of patients w/o an epidemiological link but meet pre-specified criteria. • Chlorhexidine bathing Example CRE “Bundle” -LTAC Bundled Interventions • • • • • Daily CHG 2% baths for patients Enhanced environmental cleaning Surveillance cultures at admission Serial point prevalence surveys Training/education of personnel Munoz-Price et al. Infect Control Hosp Epidemiol 2010; 31:341-347 37 Summary • CRE rates are increasing • CRE infections carry high morbidity and mortality • Treatment options are limited and will remain so for at least the next 5-10 years • Control within institutions requires multiple prevention strategies AND multidisciplinary efforts – EVERYONE must be informed and active to prevent CRE! • GOWNS, GLOVES and HAND HYGIENE EVERY TIME!!! • Antibiotic Stewardship!!!!!!!!!!!! • More research needed!!! 38 Additional Resources • CDC’s site on CRE: http://www.cdc.gov/HAI/organisms/cre/index.html • http://abcnews.go.com/Health/cre-tops-list-scarysuperbugs/story?id=18666434#.UeW4_xZB7N8 • http://www.cbsnews.com/video/watch/?id=50150 323n superbug cases found in at least 43 states CBS News Video • Oregon state CRE toolkit: http://public.health.oregon.gov/DiseasesCondition s/DiseasesAZ/CRE/Documents/cre_toolkit.pdf