Flowers - Lebanese Society of Medical Oncology (LSMO)
advertisement

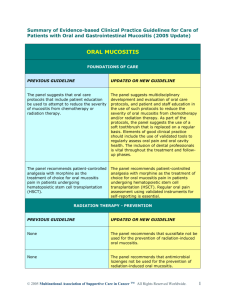
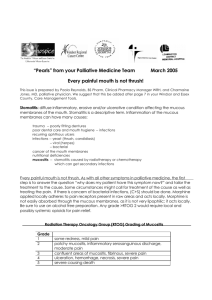
Oral Mucositis At AUBMC Nada Nassar, RN, BSN, MSN, Nursing Quality Improvement Program Zeina Kassem, BSN, RN November 2008 Outline I. II. III. IV. V. VI. VII. VIII. IX. Oral mucositis: definition and description Incidence, prevalence Risk factors Management Patient education Implications Oral Mucositis Project at AUBMC Evaluation Future projects Objectives By the end of the session the audience will be able to: Acknowledge what is oral mucositis and its impact on patient’s condition and quality of life Identify risk factors for oral mucositis Identify different stages of oral mucositis Acknowledge the new AUBMC Oral Mucositis Assessment Tool Perform complete physical assessment Identify strategies to prevent oral mucositis and to manage oral mucositis if present Definition of Oral Mucositis Mucositis is an inflammatory and potentially ulcerative process that affects the mucous membranes of the oral cavity and gastrointestinal tract of individuals receiving chemotherapy and radiation therapy as treatments for cancer. Definition Oral Mucositis Oral Mucositis can lead to serious clinical complications including hemorrhage, pain, taste changes, erythema, swelling, infection and impaired nutritional status. It significantly affects the patient’s quality of life, jeopardizes treatment outcomes, prolongs patient’s length of stay, increases morbidity and increases the financial burden on patients. Definition Oral Mucositis Historically, literature used the terms mucositis and stomatitis in combination (i.e., mucositis/ stomatitis) are almost interchangeably. Definition Oral Mucositis Individuals with mucositis use the terms pain, bleeding, taste changes, and dry mouth to report the symptoms that they experience and have reported mucositis to be the most distressing symptom of high-dose therapy Definition Oral Mucositis Mucositis remains a major dose-limiting side effect of cancer therapy. This dose-limiting effect is related to the risk of life-threatening infections secondary to breakdown in the mucosal lining that normally provides the first line of defence against microbial invasion by the organisms in the oral cavity. Incidence and Prevalence Oral mucositis occurs in 40% of cancer patients receiving cytotoxic chemotherapy. Studies report that 70 to 80% of patients undergoing bone marrow transplantation suffer from oral mucositis during treatment. One million episodes of oral mucositis occur annually in America. Risk Factors Age ( young children and elderly) Gender ( women are at greater risk for severe mucositis) Oral health and oral hygiene Reduced salivary function High expression of cytokines Altered drug metabolisms Risk Factors Smoking Alcohol Specific chemotherapeutic agents( ex: Bleomycin, Cytarabine, Doxorubicin, 5 FU) Bone marrow transplantation Radiotherapy Management Assessment—use of standardized assessment tool Collaborative management Oral care protocol, including patient education Pre treatment dental evaluation, repair, and prevention Nutrition and fluid management Prevention of mucositis with 5-fluorouracil—use of 30 minutes of cryotherapy Treatment—symptom-focused interventions Management Assessment The oral cavity should be assessed regularly using valid and reliable instruments to document “normal pattern” of changes seen with cancer treatment regimens. Management Implement an oral care protocol using a. Non-irritating agents i. Normal saline with or without baking soda ii. Sterile water iii. Avoid mouth washes with alcohol. b. Soft-bristle toothbrush i. Continue as long as tolerated if no uncontrolled bleeding present ii. Changed frequently especially when patient is neutropenic (at least every week during aplasia) Management c. Floss If a regular part of patient’s oral care, continue as long as tolerated if no uncontrolled bleeding present. d. Use foam toothettes for cleansing of soft tissues and for teeth when tooth brush is not tolerated. Management Use a multidisciplinary team approach to oral care to include the integration of dental health professionals as indicated by the status of a patient’s oral cavity. a. Clean and repair teeth prior to initiation of immunosuppressive therapy. b. Treat potential problems prior to initiation of immunosuppressive therapy Patient Education Patients and family care providers should learn about a. The importance of oral care during cancer treatment to decrease morbidity and mortality b. Systematic care of oral cavity—promote health and avoid trauma Patient Education c. Assessment of the oral cavity (i.e., at least daily during therapy) d. Signs and symptoms to report (i.e., changes in sensation or taste, presence of ulcerations and/or bleeding) Implications The first crucial step in treating oral mucositis is performing a thorough assessment of patient’s oral cavity. Implications The nursing daily physical assessment form at AUB MC includes a part related to integumentary system which does not clearly specify proper assessment of oral cavity; thus nurses are not properly assessing oral mucositis based on an evidence based assessment tool. Oral Mucositis Project at AUBMC The purpose of the project done at AUBMC is to adopt or create a tool for assessing oral mucositis that is well defined, evidence based, reliable, and culturally sensitive. Oral Mucositis Project at AUBMC Organizing the Team: A team was formed from nurses working on oncology units: Seven registered nurses 1 clinical educator 1 advanced practice nurse Oral Mucositis Project at AUBMC Assessment of oncology patient’s medical records was done at the American University of Beirut Medical Center (AUBMC) that revealed 39.74% of patients receiving chemotherapy developed oral mucositis. This result is similar to those results reported by the literature and thus oral mucositis is an important issue that needs to be surveyed by oncology nurses at AUB MC. Oral Mucositis Project at AUBMC This raises an alarm to the magnitude of the problem and the importance of exploring it profoundly in an attempt to promote patient outcomes. Oral Mucositis Project at AUBMC Briefing: A prospective and retrospective review of patient medical records for the presence of mucositis was conducted at AUB MC on the oncology units (3 units) during the period from November 2007 to January 2008 (3 months). Oral Mucositis Project at AUBMC Method: A form for data collection was developed to assess the evidence of mucositis, age, gender, admitting diagnosis, and initiation of mucositis treatment. Retrospective review: patient medical records were assessed for the documentation of the evidence of oral mucositis in the progress notes (doctors and nurses) and medical orders (for initiation of therapy). Oral Mucositis Project at AUBMC Method: Prospective review: patient’s charts on the units were surveyed for the presence of assessment and documentation of oral mucositis. Oral Mucositis Project at AUBMC Results: The retrospective study (N=50) revealed a prevalence of 18% of oral mucositis while in the prospective study (N=28) revealed 78.57% prevalence. This may be explained as a result of the awareness about oral mucositis the importance of its assessment that was discussed by the team members collecting data with the nurses. Oral Mucositis Project at AUBMC Results The combined data showed a prevalence of 39.74% of oral mucositis where 40% only received treatment. Despite its large magnitude, this result is similar to what is reported by the literature (Debra & Knobf, 2004). Oral Mucositis Project at AUBMC Variables Retrospective Data N. ( Sample = 50) Percentage Variables Age Evidence of Mucositis Gender Treatment for Mucositis 20-50 > 50 Male Female Yes No Yes No 14 36 21 29 9 41 9 41 28% 72% 42% 58% 18% 82% 18% 82% Age Evidence of Mucositis Gender Treatment for Mucositis Prospective Data 20-50 > 50 Male Female Yes No Yes No N. ( Sample = 28) 12 16 13 15 22 6 22 6 42.80% 57.14% 46.42% 53.57% 78.57% 21.42% 78.57% 21.42% Percentage Oral Mucositis Project at AUBMC Variables Combined Data N. ( Sample = 78) Percentage Age Evidence of Mucositis Gender Treatment for Mucositis 20-50 > 50 Male Female Yes No Yes No 26 52 34 44 31 47 31 47 33.33% 66.67% 43.58% 56.41% 39.74% 60.25% 40.00% 60.00% Oral Mucositis Project at AUBMC Results: Despite the small sample of this assessment exercise, the need to properly assess oral mucositis in oncology patients is identified as a need for AUB MC nurses. As a result of this needs assessment, a proposal of an oral mucositis assessment tool was initiated by the team members. Oral Mucositis Project at AUBMC Literature review Literature review exploring the published assessment tools is conducted utilizing CINAHL, PubMed, Cochrane… The tools were assessed for reliability, validity, clinical usefulness, level of evidence, and other reviews available. Oral Mucositis Project at AUBMC Oral Mucositis Assessment tools There are several assessment tools available in the literature for performing assessment of oral mucositis (Elier, 2005). Oral Assessment Guide. Oral Mucosa Rating Scale. Oral Mucositis Index (uses subset of Mucosa Rating Scale). Oral Mucositis Assessment Scale. Spijkervet Radiation Mucositis Scale. Oral Mucositis Project at AUBMC Oral Mucositis Assessment tools Western Consortium for Cancer Nursing Research Scale. World Health Organization (WHO). National Cancer Institute Common Toxicity Criteria (NCICTC) scale. Several studies conducted favor the utilization of WHO, Oral Assessment Guide and National Cancer Institute Common Toxicity Criteria (NCICTC) assessment tools due to their practicality (Raber et al, 2000). Oral Mucositis Project at AUBMC Oral Mucositis Assessment tools The WHO tool assesses the oral mucositis for erythema, ulceration, and diet tolerance without clearly identifying the severity of pain. The Oral Assessment Guide assesses erythema and functioning of the oral cavity without identifying the other aspects such as diet tolerance and pain. National Cancer Institute Common Toxicity Criteria (NCICTC) assesses ulceration erythema and pain but is not very clear and comprehensive. Oral Mucositis Project at AUBMC Creating Our Own Tool After studying the above mentioned tools, the team members opted to create an assessment tool to include all the needed criteria included in the 3 tools. Oral Mucositis Project at AUBMC Approvals Approval from the administration was secured. Two oncologists were consulted and they validated the usage of this tool to enhance multidiscplinary involvement. Oral Mucositis Project at AUBMC Pilot Phase The Piloting process: Unit Process Timeline 9North Training of RNs 2 weeks Implementation 2 months (Nov, Dec 2008) Evaluation Ongoing with the implementation Training of RNs 1 week Implementation 2 months (Nov, Dec 2008) Evaluation Ongoing with the implementation Overall Evaluation All through BMT Team members Oral Mucositis Project at AUBMC Training Phase The training of RNs included: Stages of oral mucositis Timing and duration of assessment Assessment sequence Equipment needed Sites to be evaluated How to perform the physical examination Oral Mucositis Project at AUBMC Training Phase How to document findings How to link the findings from the Oral Mucositis Assessment Tool to the Nursing Care Plan, Multidisciplinary Notes and the intershift report. Pocket guide oral mucositis assessment tool was developed for all oncology nurses Oral Mucositis Project at AUBMC Implementation Phase The Oral Mucositis Assessment Tool will be launched on all oncology units after the completion of the pilot and evaluation by the team members. Evaluation The continuous evaluation that is being conducted till now (15 days) is very promising and showing high rates of compliance on behalf of nurses. Expected Patient Outcomes Optimized practice patterns, use of the best evidence based nursing interventions for oral mucositis that will improve the quality of life of cancer patients receiving chemotherapy and radiotherapy. Future Projects The project is considered to be a research study and is presented to the nursing research council in AUBMC. References Auritcher et al (2004). Scope and Epidemiology of Cancer Therapy –Induced Oral and Gastrointestinal Mucositis. Seminars in Oncology Nursing, 20, 3-10. Debra, J. and Knobf, M. (2004).Assessing and Managing Chemotherapy-Induced Mucositis Pain. Clinical Journal of Oncology Nursing, 8,662-628. Duncan, M. and Grant, G.(2003). Review Article: Oral and Intestinal Mucositis –Causes and Possible Treatments. Aliment Pharmacotherapy, 18,853-874. Elier, J. (2005). Measuring Oncology Sensitive Patient Outcomes: Evidenced Based Summary. References Oncology Nursing Society (2007). Mucositis. What Interventions are Effective for Managing Oral Mucositis in People Receiving Treatment for Cancer? Raber, J. et al. (2000).Oral Mucositis in Patients Treated with Chemotherapy for Solid Tumors: A Retrospective Analysis of 150 Cases. Supportive Care in Cancer, 8,366- 371. Rubenestein, E. et al, (2004). Clinical practice Guidelines for the Prevention and Treatment of Cancer Therapy – Induced Oral and Gastrointestinal Mucositis. Cancer 100, 2025-2026. Sonis, ST. et al. (2004). Perspective on Cancer Therapy Induced mucosal injury: Pathogenesis, Measurement Epidemiology, and Consequences for patients. Cancer 100, 1995-2025.