click here for slides
advertisement

Assessing Immune Correlates of
Protection Via Estimation of the Vaccine
Efficacy Curve
Peter Gilbert
Fred Hutchinson Cancer Research Center and
University of Washington,
Department of Biostatistics
ISCB Vaccines Sub-Committee Web Seminar Series
November 7, 2012
Outline
1. Introduction: Concepts and definitions of immune
correlates/surrogate endpoints
2. Evaluating an immune correlate of protection via the vaccine
efficacy curve
3. Statistical methods
2
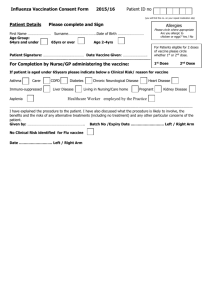
Context: Preventive Vaccine Efficacy Trial
Randomize
Vaccine
Placebo
Receive
inoculations
Measure
immune
response
• Primary Objective
– Assess VE: Vaccine Efficacy to
prevent pathogen-specific
disease
• Secondary Objective
– Assess vaccine-induced
immune responses as
correlates of protection
Follow for clinical endpoint
(pathogen-specific disease)
3
Importance of an Immune Correlate
•
Finding an immune correlate is a central goal of vaccine research
– One of the 14 ‘Grand Challenges of Global Health’ of the NIH & Gates
Foundation (for HIV, TB, Malaria)
•
Immune correlates useful for:
– Shortening trials and reducing costs
– Guiding iterative development of vaccines between basic and clinical
research
– Guiding regulatory decisions
– Guiding immunization policy
– Bridging efficacy of a vaccine observed in a trial to a new setting
•
Pearl (2011, International Journal of Biostatistics) suggests that
bridging is the reason for a surrogate endpoint
4
Two Major Concepts/Paradigms for Surrogate
Endpoints
Causal agent paradigm (e.g., Plotkin, 2008, Clin Infect Dis)
Causal agent of protection = marker that mechanistically
causes vaccine efficacy against the clinical endpoint
Prediction paradigm (e.g., Qin et al., 2007, J Infect Dis)
Predictor of protection = marker that reliably predicts the level
of vaccine efficacy against the clinical endpoint
Both are extremely useful for vaccine development, but are
assessed using different approaches
For the goal of statistical assessment of surrogate endpoint validity
in an efficacy trial, the prediction paradigm is used
As in the statistical literature, a good surrogate endpoint allows
predicting VE from the vaccine effect on the surrogate
5
Immune Correlates Terminology: Contradictions
Qin et al. (2007)
Plotkin (2008)
• Correlate (of risk) = measured
immune response that predicts
infection in the vaccine group
• Correlate (of protection) =
measured immune response that
actually causes protection
(mechanism of protection)
• Surrogate = measured immune
response that can be used to
reliably predict VE (is definitely
not a mechanism of protection)
• Surrogate = measured immune
response that can be used to
reliably predict VE (may or may
not be a mechanism of
protection)
Qin et al. correlate Plotkin correlate [very different]
Qin et al. surrogate Plotkin surrogate
6
Reconciliation of Terminology:
Plotkin and Gilbert (2012, Clin Inf Dis)
Term
Synonyms
Definition
CoP
Correlate of
Protection
Predictor of
Protection;
Good Surrogate
Endpoint
An immune marker statistically correlated
with vaccine efficacy (equivalently
predictive of vaccine efficacy)* that may or
may not be a mechanistic causal agent of
protection
mCoP
Mechanistic
Correlate of
Protection
Causal Agent of
Protection; Protective
Immune Function
A CoP that is mechanistically causally
responsible for protection
nCoP
Non-Mechanistic
Correlate of
Protection
Correlate of Protection A CoP that is not a mechanistic causal agent
Not Causal; Predictor of protection
of Protection Not
Causal
*A CoP can be used to accurately predict the level of vaccine efficacy conferred to
vaccine recipients (individuals or subgroups defined by the immune marker level).
Thus a CoP is a surrogate endpoint in the statistical literature, and may be assessed
7
with the Prentice framework or the principal stratification
framework.
A Predictive Surrogate/CoP May or May Not be a
Mechanism of Protection*
Definition of a CoP: An endpoint that can be used to reliably predict the vaccine
effect on the clinical endpoint
Plotkin and Gilbert (2012, Clin Inf Dis) Figure 1. A correlate of protection (CoP)
may either be a mechanism of protection, termed mCoP, or a non-mechanism of
protection, termed nCoP, which predicts vaccine efficacy through its (partial)
correlation with another immune response(s) that mechanistically protects.
8
Many Ways for a CoR to Fail to be a CoP
“A Correlate Does Not a Surrogate Make” –Tom Fleming
1. The biomarker is not in the pathway of the intervention's
effect, or is insensitive to its effect
– E.g., the immunological assay is noisy
2. The biomarker is not in the causal pathway of the
exposure/infection/disease process
– E.g., the antibody response neutralizes serotypes of the
pathogen that rarely expose trial participants but fails to
predominantly exposing serotypes
3. The intervention has mechanisms of action independent
of the disease process
– E.g., other immunological functions not measured by the assay
are needed for protection
9
Catastrophic Failure of a CoR to be a CoP:
the ‘Surrogate Paradox’
• Surrogate Paradox: The vaccine induces an immune response,
the immune response is inversely correlated with disease risk in
vaccinees, but VE < 0%
Three Causes of the Surrogate Paradox*
1. Confounding of the association between the potential
surrogate and the clinical endpoint
2. The vaccine positively affects both the surrogate and the
clinical endpoint, but for different sets of subjects
3. The vaccine may have a negative clinical effect in ways not
involving the potential surrogate
*From Tyler VanderWeele
10
“There is a plague on Man, the opinion that he
knows something.”
− Michel de Montaigne (1580, Essays)
Outline
1. Introduction: Concepts and definitions of immune
correlates/surrogate endpoints
2. Evaluating an immune correlate of protection via the vaccine
efficacy curve*
3. Statistical methods
*Gilbert, Hudgens, Wolfson (2011, J Inter Biostatistics) discussed the
scientific value of the vaccine efficacy curve for vaccine development
12
Two Frameworks for Assessing a CoP from a Single Vaccine
Efficacy Trial: Prentice & Principal Stratification (PS)
Key Issue: Do trial participants have prior exposure to the pathogen
under study?
If Yes, immune responses vary for both vaccine and placebo
recipients
In this case, the Prentice and PS frameworks both apply
If No, immune responses vary for vaccinees only, and the Prentice
framework does not apply (Chan et al., 2002, Stats Med)
In this case, only the PS framework applies
In this talk we consider the PS approach in both settings
13
Concept of PS Framework: Assess Association of IndividualLevel Vaccine Effects on the Surrogate and Clinical Endpoint
Vaccine Effect on Clinical Endpoint
Probability an individual is protected
Vaccine Effect on Immune Response Marker for an Individual
14
Definition of a Principal Surrogate/Principal CoP
•
Define the vaccine efficacy surface as
VE(s1, s0) = 1 –
Risk of clinical endpoint for vaccinees for subgroup with marker effect (s1, s0)
Risk of clinical endpoint for placebos for subgroup with marker effect (s1, s0)
•
Interpretation: Percent reduction in clinical risk for a vaccinated
subject with markers (s1, s0) compared to if s/he had not been
vaccinated
•
Definition: A principal CoP is a marker with large variability of
VE(s1, s0) in (s1, s0)
•
Another useful property is VE(s1 = s0) = 0
– This property is Average Causal Necessity: No vaccine effect on
the marker implies no vaccine efficacy
15
Marker Useless as a CoP
VE(s1,
CEPRs0)
(v1, v0)
16
Marker that is an Excellent CoP
VE(s1,
CEPRs0)
(v1, v0)
17
Simplest Way to Think About the PS Framework for
Assessing a CoP: It’s Simply Subgroup Analysis
• Conceptually the analysis assesses VE in subgroups defined by the
vaccine effect on the marker
– Evaluate if and how VE varies with ‘baseline’ subgroups defined
by (S1, S0)
– Principal stratification makes (S1, S0) equivalent to a baseline
covariate
• A useful CoP will have strong effect modification, i.e., VE(s1, s0)
varies widely in (s1, s0)
• It would be even more valuable to identify actual baseline covariates
that well-predict VE, but it’s much more likely that a response to
vaccination well-predicts VE
18
Simplified Definition of a Principal Surrogate/Principal CoP:
Ignore the Immune Response under Placebo, S0
•
Define the vaccine efficacy curve as
VE(s1) = 1 –
Risk of clinical endpoint for vaccinees for subgroup with marker s1
Risk of clinical endpoint for placebos for subgroup with marker s1
•
Interpretation: Percent reduction in clinical risk for a vaccinated
subject with markers s1 compared to if s/he had not been
vaccinated
•
Definition: A principal CoP is a marker with large variability of
VE(s1) in s1
•
•
The vaccine efficacy curve is useful in both settings that participants have prior
exposure to the pathogen or not
If no prior exposure, then VE(s1, s0) = VE(s1), such that the vaccine efficacy
surface simplifies to the vaccine efficacy curve
19
Vaccine Efficacy Curve: Assess How VE Varies in the Marker
Under Vaccination
Black marker: worthless
as surrogate
VE(s1)
Green and blue markers
satisfy causal necessity
Blue marker: very good
surrogate
Marker level s1
20
Excellent CoP:
Sets the Target for Improving the Vaccine
Target: Improve the vaccine regimen by increasing the
percentage of vaccinees with high immune responses
Black marker: worthless
as surrogate
Green and blue markers
satisfy causal necessity
VE(s1)
Blue marker: very good
surrogate
Marker level s1
21
Knowledge of a CoP Guides Future Research to
Develop Improved Vaccines
Identification of a good CoP in an efficacy trial is the ideal primary
endpoint in follow-up Phase I/II trials of refined vaccines
It also generates a bridging hypothesis: If a future vaccine is
identified that generates higher marker levels in more vaccinated
subjects, then it will have improved overall VE
22
Using the CoP for Improving the Vaccine
Regimen
Marker levels
Original Vaccine
New Vaccine 1
23
New Vaccine 2
Using the CoP for Improving the Vaccine
Regimen
Suppose each new vaccine is tested in an efficacy trial
Under the bridging hypothesis we expect the following efficacy
results:
Original Vaccine
New Vaccine 1
New Vaccine 2
Estimated VE
Overall TE = 75%
Overall TE = 50%
Overall TE = 31%
Marker level
Marker level
Marker level
This is the idealized model for using a CoP to iteratively improve a
vaccine regimen
24
Outline
1. Introduction: Concepts and definitions of immune
correlates/surrogate endpoints
2. Evaluating an immune correlate of protection via the vaccine
efficacy curve
3. Statistical methods
25
Challenge to Evaluating a Principal CoP: The Immune Responses to
Vaccine are Missing for Subjects Assigned Placebo
• Accurately filling in the unknown immune responses is needed
to evaluate a principal CoP
• Two approaches to filling in the missing data (Follmann, 2006,
Biometrics):
– BIP (Baseline immunogenicity predictor): At baseline, measure a
predictor(s) of the immune response in both vaccinees and placebos
– CPV (Close-out placebo vaccination): At study closeout, vaccinate
disease-free placebo recipients and measure the immune response
26
Example of a Good BIP:
Antibody Responses to Hepatitis A and B Vaccines*
Spearman rank
r = .85
No crossReactivity
N=75 subjects
27
*Czeschinski et al. (2000, Vaccine) 18:1074-1080
Baseline Immunogenicity Predictor
28
Schematic of Baseline Immunogenicity Predictor (BIP) &
Closeout Placebo Vaccination (CPV) Trial Designs*
Vx S=S(1)
W
-
BIP Approach
1 1 +
CPV Approach
S(1)
Vx
W
BIP Approach
-
29 (2006, Biometrics)
*Proposed by Follmann
Sc
1 1 +
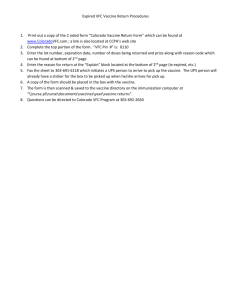
Literature on Statistical Methods for Estimating the
Vaccine Efficacy Curve via BIP and/or CPV
Article
Comment
1. Follmann (2006,
Biometrics)
Binary outcome; BIP&CPV; Estimated likelihood
2. Gilbert and Hudgens
(2008, Biometrics)
Binary outcome; BIP; Estimated likelihood; 2-phase sampling
3. Qin, Gilbert, Follmann,
Li (2008, Ann Appl Stats)
Time-to-event outcome (Cox model); BIP&CPV; Estimated likelihood; 2phase sampling
4. Wolfson and Gilbert
(2010, Biometrics)
Binary outcome; BIP&CPV; Estimated likelihood; 2-phase sampling; relaxed
assumptions
5. Huang and Gilbert
(2011, Biometrics)
Binary outcome; BIP&CPV; Estimated likelihood; 2-phase sampling; relaxed
assumptions; compare markers
6. Huang, Gilbert, Wolfson Binary outcome; BIP&CPV; Pseudolikelihood; 2-phase sampling; relaxed
(2012, under revision)
assumptions; marker sampling design
7. Miao, Li, Gilbert, Chan
(2012, under revision)
Time-to-event outcome (Cox model); BIP; Estimated likelihood with
multiple imputation; 2-phase sampling
8. Gabriel and Gilbert
(2012, submitted)
Time-to-event outcome (Weibull model); BIP+CPV; Estimated likelihood
and pseudolikelihood; 2-phase
sampling; threshold models
30
Summary of One of the Principal Stratification
Methods:
Gilbert and Hudgens (2008, Biometrics) [GH]
31
Notation (Observed and Potential Outcomes)
Z = vaccination assignment (0 or 1; placebo or vaccine)
W = baseline immunogenicity predictor of S
S = candidate surrogate endpoint/immune CoP measured at
time after randomization
Y = clinical endpoint (0 or 1; 1 = experience event during follow-up)
S(Z) = potential surrogate endpoint under assignment Z, for Z=0,1
Y(Z) = potential clinical endpoint under assignment Z, for Z=0,1
32
Assumptions
A1 Stable Unit Treatment Value Assumption (SUTVA):
(Si(1), Si(0), Yi(1), Yi(0)) is independent of the treatment assignments Zj of
other subjects
− A1 implies “consistency”: (Si(Zi), Yi(Zi)) = (Si, Yi)
A2 Ignorable Treatment Assignment:
Zi is independent of (Si(1), Si(0), Yi(1), Yi(0))
− A2 holds for randomized blinded trials
A3 Equal individual clinical risk up to time that S is measured
(zero vaccine efficacy for any individual up to time )
33
Definition of a Principal Surrogate/Principal CoP
(Frangakis and Rubin, 2002; Gilbert and Hudgens, 2008)
• Define
risk(1)(s1, s0) = Pr(Y(1) = 1|S(1) = s1, S(0) = s0)
risk(0)(s1, s0) = Pr(Y(0) = 1|S(1) = s1, S(0) = s0)
• A contrast in risk(1)(s1, s0) and risk(0)(s1, s0) is a causal effect on Y for the
population {S(1) = s1, S(0) = s0}
• VE(s1, s0) = 1 - risk(1)(s1, s0) / risk(0)(s1, s0)
• A good CoP has VE(s1, s0) varying widely in (s1, s0) [i.e., a large amount of
effect modification]
• Also, with VE(s1) = 1 - risk(1)(s1) / risk(0)(s1), a good CoP has VE(s1) varying
widely in s1
• These definitions allow for a spectrum of principal CoPs, some more
useful than others, depending on the degree of effect modification
34
Statistical Methods:
Build on Two-Phase Sampling Methods
• Case-cohort or case-control sampling (Ignore S0)
− (W, S(1)) measured in
• All infected vaccines
• Sample of uninfected vaccines
− W measured in
o All infected placebos
o Sample of uninfected placebos
• 2-Phase designs (E.g., Prentice, 1986, Biometrika; Kulich and and Lin,
2004, JASA; Breslow et al., 2009, AJE, Stat Biosciences)
− Phase 1: Measure inexpensive covariates in all subjects
− Phase 2: Measure expensive covariates X in a sample of subjects
• Our application
− Vaccine Group: Exactly like 2-phase design with X = (W, S(1))
− Placebo Group: Like 2-phase design with X = (W, S(1)) and S(1) missing
35
IPW Case-Cohort Methods Do Not Apply: Hence we use
a Full Likelihood-Based Method
• Most of the published 2-phase sampling/case-cohort failure time
methods cannot be extended to estimate the VE curve
– This is because they are inverse probability weighted (IPW) methods, using
partial likelihood score equations that sum over subjects with phase-2 data
only, which assume that every subject has a positive probability that S(1) is
observed
– However, all placebo subjects have zero-probability that S(1) is observed
• To deal with this problem, the published methods all use full
likelihood, using score equations that sum over all subjects
36
Maximum Estimated Likelihood* with BIP
•
Posit models for risk(1)(s1,0; ) and risk(0)(s1,0; )
•
Vaccine arm:
•
•
−
(Wi, Si(1)) measured:
−
(Wi, Si(1)) not measured:
Likld contribn
risk(1)(Si(1), 0; )
risk(1)(s1, 0; ) dF(s1)
Placebo arm:
−
Wi measured:
−
Wi not measured:
Likld contribn
risk(0)(s1, 0; ) dFS|W(s1| Wi)
risk(0)(s1, 0; ) dF(s1)
L(, FS|W, F) = i risk(1)(Si(1),0; )Yi (1 - risk(1)(Si(1),0; ))1-Yi]Zi }i
[Vx subcohort]
risk(0)(si,0; )dFS|W(s1|Wi)Yi (1 - risk(0)(s1,0; )) dFS|W(s1|Wi)1-Yi]1-Zi }i [Plc subcohort]
risk(1)(si,0; )dF(s1)Yi (1 - risk(1)(s1,0; )) dF(s1)1-Yi]Zi }1-i
[Vx not subcohort]
risk(0)(si,0; )dF(s1)Yi (1 - risk(0)(s1,0; )) dF(s1)1-Yi]1-Zi }1-i
[Plc not subcohort]
*Pepe and Fleming (1991) an early article on estimated likelihood
37
Maximum Estimated Likelihood Estimation
(MELE)
• Likelihood L(, FS|W, F)
− is parameter of interest [VE curve depends only on ]
− FS|W and F are nuisance parameters
Step 1: Choose models for FS|W and F and estimate them based on
vaccine arm data
Step 2: Plug the consistent estimates of FS|W and F into the likelihood,
and maximize it in
− e.g., EM algorithm
Step 3: Estimate the variance of the MELE of , accounting for the
uncertainty in the estimates of FS|W and F
− Bootstrap
38
Example: Nonparametric Categorical Models
• Assume:
− S and W categorical with J and K levels; Si(0)=1 for all i
[No prior exposure scenario: category 1 = negative
response]
− Nonparametric models for P(S(1)=j, W=k)
− A4-NP: Structural models for risk(z) (for z=0, 1)
risk(z)(j, 1, k; ) = zj + ’k for j=1, …, J; k=1, …, K
Constraint: 0 ≤ zj + ’k ≤ 1 and k ’k = 0 for identifiability
A4-NP asserts no interaction: W has the same effect on
risk for the 2 study groups (untestable)
39
Vaccine Efficacy Curve for Categorical Marker
CEPrisk(j, 1) = log (avg-risk(1)(j, 1) / avg-risk(0)(j, 1))
where avg-risk(z)(j, 1) = (1/K) k risk(z)(j, 1, k; )
VE(j, 1) = 1 – exp{CEPrisk(j, 1)}
The vaccine efficacy curve is VE(j, 1) at each level j
of S(1)
40
Tests for the Vaccine Efficacy Curve
VE(j, 1) Varying in j
• Wald tests for whether a biomarker has any surrogate value
− Under the null, PAE(w) = 0.5 and AS = 0
− Z = (Est. PAE(w) – 0.5)/ s.e.(Est. PAE(w))
− Z = Est. AS/ s.e.(Est. AS)
o Estimates obtained by MELE; bootstrap standard errors
• For nonparametric case A4-NP, test H0: CEPrisk(j, 1) = 0 vs H1:
CEPrisk(j, 1) increases in j
(like Breslow-Day trend test)
T = j>1(j-1) {Est. 0j – (Est. 0j + Est. 1j)(Est. z0 /(Est. z0 + Est. z1))}
divided by bootstrap s.e.
Est. z = (1/J) j zj
41
Simulation Study:
Vax004 HIV Vaccine Efficacy Trial*
• Step 1: For all N=5403 subjects, generate (Wi, Si(1)) from a bivariate
normal with means (0.41, 0.41), sds (0.55, 0.55), correlation
= 0.5, 0.7, or 0.9
sd of 0.55 chosen to achieve the observed 23% rate of left-censoring
Values of Wi, Si(1) < 0 set to 0; values > 1 set to 1
• Step 2: Bin Wi and Si(1) into quartiles
Under model A4-NP generate Yi(Z) from a Bernoulli(zj + ’k) with the
parameters set to achieve:
o P(Y(1) = 1) = 0.067
and
P(Y(0) = 1) = 0.134 (overall VE = 50%)
o The biomarker has either (i) no or (ii) high surrogate value
*Flynn et al. (2005, JID), Gilbert et al. (2005,
42 JID)
Simulation Plan
• Scenario (i) (no surrogate value)
− CEPrisk(j, 1) = -0.69 for j = 1, 2, 3, 4
− i.e., VE(j, 1) = 0.50 for j = 1, 2, 3, 4
• Scenario (ii) (high surrogate value)
− CEPrisk(j, 1) = -0.22, -0.51, -0.92, -1.61 for j = 1, 2, 3, 4
− i.e., VE(j, 1) = 0.2, 0.4, 0.6, 0.8
for j = 1, 2, 3, 4
43
Simulation Plan
• Step 3: Create case-cohort sampling (3:1 control: case)
− Vaccine group: (W, S(1)) measured in all infected
(n=241) and a random sample of 3 x 241 uninfected
− Placebo group: W measured in all infected (n=127) and
a random sample of 3 x 127 uninfected
• The data were simulated to match the real VaxGen trial as
closely as possible
44
Model A4-NP Simulation Results: Bias and
Coverage Probabilities [Table 1 of GH]
45
Model A4-NP Simulation Results: Power to Detect the
VE(j,1) curve varying in j [Table 2 of GH]
Trend tests for VE(j, 1) increasing in j: Power 0.83, 0.99, > 0.99 for = 0.5, 0.7, 0.9
46
Conclusions of Simulation Study
• The MELE method of Gilbert and Hudgens performs well for
realistically-sized Phase 3 vaccine efficacy trials, with accuracy,
precision, and power improving sharply with the strength of
the BIP (desire high )
• This shows the importance of developing good BIPs
• R code for the nonparametric method available at the
Biometrics website and at
http://faculty.washington.edu/peterg/SISMID2011.html
47
Remarks on Power for Evaluating a Principal
Surrogate Endpoint (For All Methods- Beyond GH)
• Crossing over more placebo subjects improves power of CPV and BIP + CPV
designs
• There is no point of diminishing returns− steady improvement with more
crossed over, out to complete cross-over
• If the BIP is high quality (e.g., > 0.50), then the BIP design is quite
powerful with only modest incremental gain by adding CPV
• However, CPV has additional value beyond efficiency improvement:
– Helps in diagnostic tests of structural modeling assumptions (A4)
– May help accrual and enhance ethics
– May adaptively initiate crossover, e.g., as soon as the lower 95%
confidence limit for VE exceeds 30%
• Pseudoscore method superior to estimated likelihood method (Huang,
Gilbert, Wolfson, 2012, under revision); recommend this method in practice
– Happy to provide the code for this method (for BIP, CPV, BIP+CPV)
48
Concluding Remarks
• Opportunity to improve assessment of immune CoPs by increasing
research into developing BIPs
– The better the BIP, the greater the accuracy and precision for estimating
the vaccine efficacy curve
49
Some Avenues for Identifying Good BIPs
• Demographic factors
– E.g., age, gender, BMI, immune status
• Host immune genetics
– E.g., HLA type and MHC binding prediction machine learning methods
for predicting T cell responses
• Add beneficial licensed vaccines to efficacy trials and use known correlates
of protection as BIPs (Follmann’s [2006] original proposal)
– The HVTN is exploring this strategy in a Phase 1 trial in preparation for
efficacy trials
• Develop ‘pathogen exposure history’ chip
• In efficacy trials where participants have prior exposure to the pathogen,
measure the potential CoP at baseline and use it as the baseline predictor
– E.g., Varicella Zoster vaccine trials: baseline gpELISA titers strongly
predict post-immunization titers
– Miao, Li, Gilbert, Chan (2012, under review) and Gabriel and Gilbert
(2012, in preparation) estimate the Zoster vaccine efficacy curve using
this excellent BIP (will constitute an excellent example when
published)
50