Ticke-Borne Illnesses
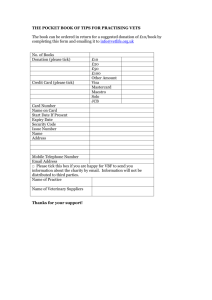
advertisement

Creepy, Crawly Killers Tick-Borne Illnesses Tick Identification Lyme Disease Transmitted by Ixodes scapularis “deer tick” Borrelia burgdorferi Most common vector-borne zoonotic infection in the United States Seasonal Variation Most cases occur in the warmer months ◦ Outdoor activity is highest ◦ Nymph activity is at its peak Stages: Primary Symptoms: 7-10 days after bite Erythema migrans: 80% of patients Belt line, axillary, inguinal, or popliteal 25% report bite Stages: Primary Flu-Like Symptoms ◦ ◦ ◦ ◦ Fatigue (54%) Anorexia (26%) Myalgias (44%) and arthralgias (44%) Fever (16%) Regional lymphadenopathy (23%) Headache (42%), neck stiffness (35%) ◦ Meningeal findings absent, CSF studies normal Stages: Secondary Rash can evolve Stages: Secondary Cranial neuropathy Meningoencephalitis Meningeal signs typically absent CSF studies may be positive Stages: Secondary Myopericarditis Stages: Secondary Atrioventricular block Stages: Secondary Rarely ◦ ◦ ◦ ◦ ◦ Conjunctivitis Keratitis Uveitis Optic neuritis Blindness Stages: Tertiary Months - Years after bite Joint complaints (usually larger joints) 60% of untreated patients: monoarticular or oligoarticular arthritis Exacerbations less frequent over years Stages: Tertiary “Lyme encephalopathy” ◦ Mood, memory, cognition, and sleep changes Polyneuropathy Both have abnormal CSF studies Diagnosis Skin findings in endemic area ELISA IgG and IgM against Borrelia (sensitivity of 89% and specificity of 72%) ◦ Many false-positives ◦ Positive or equivocal ELISA tests may be confirmed with western blot Treatment Tick removed within 72 hours: low likelihood of infection Tick attached for at least 36 hours: consider treatment Treatment: Primary + Secondary Stages Doxycycline ◦ Adults: 100 mg BID for 14-21 days ◦ Children > 8 years: 1-2 mg/kg BID Amoxicillin ◦ Pregnant or lactating: 500 mg TID for 14-21 days ◦ Children < 8 years: amoxicillin 50 mg/kg/day, divided TID (max dose of 500mg/dose) Treatment Exceptions • Ceftriaxone • Lyme Meningitis • Severe cardiac disease Second or third degree heart block PR > 300 msec Symptomatic patients Co-Infections Babesiosis ◦ 2-40% of lyme patients Human granulocytic anaplasmosis (HGA). ◦ 2-12% of lyme patients Doxycycline does not treat babesiosis Amoxicillin does not treat HGA or babesiosis Fever persists past 6 days: suspect coinfection Babesiosis Babesia species (especially microti) Transmitted by deer tick Clinical Presentation Flu-like illness: fever, chills, headache, fatigue, and anorexia Splenomegaly More severe in splenectomized ◦ Severe hemolytic anemia, hemoglobinuria, jaundice ◦ MOD: renal insufficiency, ARDS, and DIC Diagnosis Microscopy of thick and thin Giemsa stains Antibody detection through IFA staining PCR Treatment With spleen: generally recover without treatment Severe disease, splenectomized ◦ Clindamycin + quinine x 7-10 days OR ◦ Atovaquone + azithromycin x 7-10 days Ehrlichioses Human granulocytic anaplasmosis (HGA) ◦ Anaplasma phagocytophilum ◦ Black-legged tick ◦ Upper Midwest, New England, parts of the midAtlantic states, northern California Human monocytic ehrlichiosis (HME) ◦ Ehrlichia chaffeensis ◦ Lone Star tick ◦ South central and South east Ehrlichia ewingii ◦ South central Clinical Presentation Abrupt onset of flu symptoms: fever, headache, myalgia, and shaking chills Can see GI: N/V, diarrhea, abdominal pain Rashes (HME>HGA) Meningitis Carditis MOD ◦ Renal failure ◦ DIC ◦ ARDS Diagnosis Clinical Leukopenia, thrombocytopenia Elevated LFTs Acute and convalescent antibodies Enzyme immunoassay and Western blot PCR Treatment Doxycycline or tetracycline x 7–14 days Rifampin in children if concern for tooth staining Rocky Mountain Spotted Fever Rickettsia rickettsii Southeastern United States American dog tick, Rocky Mountain wood tick, common brown dog tick, Lone star tick Frequently transmitted to humans by dogs Infection Cycle Infect vascular endothelial cells and vascular smooth muscle Cell-to-cell transfer via actin-based motility Damaged endothelium with exposed subendothelium, tissue plasminogen activator, and von Willebrand's factor Clinical Presentation Vasculitis and thrombocytopenia ◦ Early rash ◦ Petechial and hemorrhagic lesions ◦ Microinfarcts Small-vessel permeability ◦ Hypotension, edema, and increased extravascular fluid • Acute renal failure and hypovolemic shock • Direct lung invasion: interstitial pneumonitis Diagnosis Clinical Immunofluorescent assay and immunoperoxidase staining of R. rickettsii in rash biopsies Serum antibody titer PCR Cell culture Treatment Doxycycline ◦ Including children! • Chloramphenicol Pregnant women (except those near term) For significant contraindication to tetracyclines • High-dose steroids in critically ill Relapsing Fever Epidemic (louse-borne) ◦ Borrelia recurrentis • Endemic (tick-borne) Borrelia hermsii Borrelia turicatae Borrelia parkeri • Mountain and Pacific states Elevations 2,000-7,000 ft with coniferous forest Relapsing Fever Rodent-Tick/Rodent-Louse life cycle Transmitted in infected saliva Clinical Presentation Febrile episode: ~ 3 days Asymptomatic period: ~7 days Relapse ◦ Antigenic variation ◦ Cycle repeats itself three to five times ◦ Successive relapses usually less severe Diagnosis Spirochetes on peripheral smear Genus-specific PCR tests from CDC Differential ◦ malaria, typhus, dengue, yellow fever, Colorado tick fever, and tularemia Treatment Tetracycline or erythromycin 33% have Jarisch-Herxheimer ◦ Approx. 4 hours after treatment ◦ Flu-like illness: fever, chills, headache, myalgia, flushing ◦ Skin lesions ◦ Hypotension Tularemia Francisella tularensis Most common in Southwest Rodents, rabbits, prarie dogs Deer tick, the Lone Star tick, and the dog tick Horse fly, and deer fly Infected food or water Inhalation of dust or water aerosol Seasonal Variation May to August: ticks December to January: hunting/skinning of infected animals Clinical Presentation Ulceroglandular ◦ Most common form ◦ Inoculation site erythematous papule ulcerates 2 to 3 days later ◦ Regional lymphadenopathy and fever Clinical Presentation Glandular ◦ LAD (usually cervical) without skin ulcer. ◦ Oropharyngeal tularemia exudative pharyngitis with associated cervical lymphadenitis ◦ Oculoglandular Unilateral conjunctivitis with regional adenopathy of pre-auricular lymph nodes Clinical Presentation Typhoidal: systemic form with no obvious entry site ◦ Fever, chills, constipation/diarrhea, abdominal pain, and weight loss ◦ 30 to 60% mortality Pulmonary ◦ Direct inhalation of aerosolized organisms or bacteremic spread from another site ◦ Fever, chills, cough, substernal burning, dyspnea Bioterrorism Category A Release of aerosolized particles ◦ ◦ ◦ ◦ ◦ 3 to 5 days after exposure Acute fever Pneumonia Pleuritis Hilar lymphadenopathy Diagnosis PCR Do not culture bubo ◦ Notify lab personnel if you do Treatment Do not need patient isolation Streptomycin I&D residual sterile buboes after completion of antibiotics Prophylaxis with doxycycline Q Fever Coxiella burnetii Cattle, sheep, goats Rocky Mountain wood tick Midwest states and California 80% of cases in males Extremely resistant One organism can cause infection Category B biologic warfare agent Clinical Presentation (Acute) Fever (often 40° C or higher), myalgia Chest pain Atypical PNA Retrobulbar headache Chronic Granulomatous hepatitis Culture-negative endocarditis ◦ Up to 68% of patients with chronic Q fever ◦ Up to 25% mortality rate ◦ Usually a history of valvular heart disease Diagnosis Do not culture (risk to lab workers) ELISA assays ◦ Takes 2 - 3 weeks Treatment • Uncomplicated acute Doxycycline • Acute disease with valvular disease Doxycycline + Hydroxychloroquine x 1 year • Chronic Doxycycline + Hydroxychloroquine x 1.5 to 3 years • Pregnant Long-term TMP/SMX • Prophylaxis Doxycyline x 5-7 days Colorado Tick Fever Coltivirus Rocky Mountain area Rocky Mountain wood tick Clinical Presentation Flu-like: fever, chills, headache, myalgia, lethargy, anorexia, and nausea Retrobulbar pain Biphasic course : “saddleback” fever curve ◦ Sick for 2 - 3 days ◦ Well for 1 - 2 days ◦ Sick 2 - 4 days Diagnosis Immunofluoroescence PCR Treatment Almost always self-limited Supportive treatment Tick Paralysis Adult female tick Releases a neurotoxin that causes cerebellar dysfunction, ascending paralysis Southeastern and northwestern regions of the United States 47 tick species: most common Rocky Mountain wood tick and American dog tick Mechanism Ixobotoxin stops sodium flux across axonal membranes loss of acetyl choline release at neuromuscular junction Clinical Presentation Restlessness and irritability Ascending flaccid paralysis +/- acute ataxia ◦ bulbar involvement, respiratory paralysis, https://www.youtube.com/watch?v=24DZ EaUN7cc Treatment Tick removal Improvement in hours References http://www.cdc.gov/ticks/diseases/ Cline D, Ma OJ, et al. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 6th edition. McGraw-Hill, 2004 Dudley, J P (2010), “Tularemia: A Case Study In Medical Surveillance And Bioterrorism Preparedness”, JMedCBR 8, 17 September 2010, http://www.jmedcbr.org/issue_0801/Dudley/Dudley_09_10.html. Halperin JJ. Prolonged Lyme disease treatment: enough is enough. Neurology 2008;70:986 http://www.michigan.gov/emergingdiseases/0,4579,7-186-25890-75870--,00.html. Accessed 9/27/15. Nadelman RB, Nowakowski J, Forseter G, et al. The clinical spectrum of early Lyme borreliosis in patients with culture-confirmed erythema migrans. Am J Med 1996; 100:502 Rosen's emergency medicine: concepts and clinical practice 7th edition. Philadelphia, PA: Mosby/Elsevier; 2010. Steere AC, Schoe RT,Taylor E. The clinical evolution of Lyme arthritis. Ann Intern Med 1987; 107:725 Wolfson A, Hendey GW, et al. Harwood-Nuss’ Clinical Practice of Emergency Medicine, 5th edition. Philadelphia: Lippincott Williams & Wilkins and Wolters Kluwer Business, 2010. Wormser GP. Clinical Practice Early Lyme Disease. N Engl J Med 1996; 354:2794.