Podiatry Clinical Educator Handbook 2015
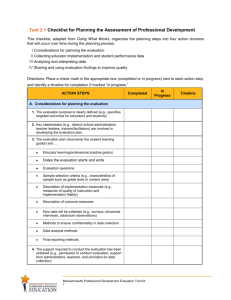
advertisement

Faculty of Health and Human Sciences School of Health Professions CLINICAL EDUCATOR HANDBOOK for BSc (Hons) Podiatry 2015-16 (leading to eligibility to apply for registration with the Health and Care Professions Council (HCPC)) BSc (Hons) Podiatry Clinical Educator Handbook 2015 1 If you require any part of this publication in larger print, or an alternative format, please contact Programme Administration at:- Faculty of Health and Human Sciences Plymouth University Rolle Building Drake Circus Plymouth PL4 8AA Telephone number: 01752 586999/01752 586964 Faculty of Health and Human Sciences Plymouth University Peninsula Allied Health Centre Derriford Road Plymouth PL6 8BH Telephone number: 01752 588800/588833 Faculty of Health and Human Sciences Plymouth University Knowledge Spa Royal Cornwall Hospital Truro TR1 3HD Telephone number: 01872 256450 BSc (Hons) Podiatry Clinical Educator Handbook 2015 2 Special Needs Notice Dear Student Important: please note If you have a disability The University is very supportive of students with disabilities, and year–onyear we are making adjustments to assist students with special needs. It may be that we have already put in place changes which will assist you – but unless we know what your needs might be, we cannot guarantee that that will be the case. If we can identify your needs sufficiently far in advance of when you intend to start a course at the University, we are better able to put in place appropriate arrangements – or, if there is a health and safety issue or an issue about the expectations of students on the course, to advise you on alternative options. However, we may not be able to do so if we do not know in advance. If you have not told us about your disability please do contact the University’s Disability Assist Services on Plymouth 01752 582278 to discuss your needs. While we are making reasonable adjustments to our provision, we may not be able to meet your individual needs if we do not have the opportunity to assess them in advance, and that could impact negatively on your experience on the course or even your ability to take up your place. If you have told us about your disability you may be asked for additional information or invited to attend an interview with Disability Assist Services. This is in order that we can properly assess your individual needs and ensure that we have the best possible chance of meeting them. Please do provide any information requested and come in to see staff if asked to do so, since otherwise you – and we - could find ourselves in a position in which it is difficult or even unsafe for you to take up your place. So please tell us about any disability – even if you do not think it will affect you while you are at the University – and respond positively to any requests for further details or for an information interview. If you do not do so, you may find yourself unable to take up your place or unable to complete the course because we have not been able adequately to meet your particular needs. BSc (Hons) Podiatry Clinical Educator Handbook 2015 3 BSc (Hons) Podiatry Clinical Educator Handbook 2015 4 CONTENTS Section Page Contact details 2 Special Needs Notice 3 Contents 5 Foreword 7 1. Purpose of the Handbook 8 2. General Information to assist the Clinical Educator 9 3. Role of the Clinical Educator 12 4. Teaching and Learning Strategies 15 5. What happens in the BSc (Hons) Podiatry programme Year One Year Two Year Three Clinical Placement 17 6. Assessment Strategy – General 22 7. Assessment Strategy within the BSc (Hons) Podiatry Programme 24 8. Practice Portfolio 25 9. Implementing the Assessment Strategy in Practice 29 10. Summary of the Assessment Process 32 11. Students’ Responsibility 33 12. Mentoring Standards 33 13. Appendices 35 BSc (Hons) Podiatry Clinical Educator Handbook 2015 17 18 19 20 5 13. Appendices 1 Glossary of Terms 37 2 Attendance Record 41 3 Sample Timesheet 43 4 Guidelines for the management of incidents that occur during undergraduate student placements 45 5 Incident Report Form 51 6 Criteria for Identifying Clinical Educators 53 7 Student Profile Document 55 8 Learning Contract 57 9 Tutorial Form (Record of Meetings) 59 10 Practice Portfolio Feedback Sheet 61 11 Reports From Others During Placement Form 63 12 Reflective Report Form 65 13 Patient Feedback Form 67 14 Learning Outcome Assessment/Sign-off Grid (Example: Communication) 69 15 Mid-Point Report Form 71 16 End of Placement Report Form 73 17 Quality Assurance Agency Benchmark Statements 75 18 Signature Record 87 19 Summary of Roles and Responsibilities 89 20 HPC Standards for Education and Training Placements 93 21 NMC Standards to support learning and assessment in practice 95 BSc (Hons) Podiatry Clinical Educator Handbook 2015 6 FOREWORD The BSc (Hons) Podiatry Programme is based in the School of Health Professions, Faculty of Health and Human Sciences, Plymouth University. The Podiatry BSc (Hons) programme, introduced in September 2002, was designed in response to the following reports: Department of Health (2000) Meeting the Challenge London, National Health Service Executive Health Professions Council (2003) Standards of Proficiency Quality Assurance Agency for Higher Education (2001) Podiatry (Chiropody) Benchmark Statement, Gloucester, Quality Agency for Higher Education Fortunately the recent revalidation of the programme in 2013 has facilitated the updating of the programme to incorporate the new Standards of Proficiency produced by the Health Professions Council (2007). This remains a very exciting and challenging time for the Podiatry profession, and the role of the Clinical Educator is central to the success of the Podiatry Programme. In accordance with other health professions, the term ‘Clinical Educator’ will be used instead of Assessor of Practice. The role however remains the same. A placement Clinical Educator is responsible for supporting and assessing the practice development of allocated students during a practice experience. We welcome your continued support, both for the programme and for the students. All the information in this Handbook is correct at the time of printing. Courses are regularly reviewed and updated so details may change. Occasionally, a module listed in the Handbook may be replaced or withdrawn. BSc (Hons) Podiatry Clinical Educator Handbook 2015 7 1. WHAT IS THE PURPOSE OF THE HANDBOOK? 1.1 The Clinical Educator Handbook for the BSc Podiatry Programme attempts to answer some of the questions that are being asked in general about assessment of practice. In addition there is specific detail about the Podiatry Programme. 1.2 The information provided in the handbook aims to increase your understanding of the content of the Programme, the assessment of practice strategy and the role of the Clinical Educator. 1.3 A glossary of terms used in the assessment of practice within the Podiatry Programme and the Practice Portfolio is provided in Appendix 1. 1.4 If you have any queries about the content, please do contact the Podiatry Placement Co-ordinator or a member of the academic staff at the Faculty of Health and Human Sciences. The academic staff are: Sally Abey Link Lecturer: Programme Lead, Podiatry Somerset Devon Plymouth sally.abey@plymouth.ac.uk Christopher Barber Lecturer, Podiatry Link Lecturer: North Devon christopher.barber@plymouth.ac.uk Margaret Bruce Lecturer, Podiatry Link Lecturer: North Somerset margaret.bruce@plymouth.ac.uk Emma Cowley Link Lecturer: Lecturer, Podiatry Wiltshire Cornwall and the Isles of Scilly emma.cowley@plymouth.ac.uk Vasileios Lepesis Link Lecturer Lecturer, Podiatry Bournemouth and Poole Bristol Vasileios.lepesis@plymouth.ac.uk Catherine Smith Link Lecturer: Lecturer & Placement Co-ordinator Gloucester, Cheltenham & Cirencester Bath and North East Somerset Torbay Care Trust South Gloucester catherine.smith@plymouth.ac.uk BSc (Hons) Podiatry Clinical Educator Handbook 2015 8 Please copy in podplacements@plymouth.ac.uk when emailing contacts in case the recipient is unable to access their emails. 2. GENERAL INFORMATION TO ASSIST THE CLINICAL EDUCATOR 2.1 Professional programmes require students to successfully complete periods of clinical/professional placement as a condition of progression and graduation. These placements are provided by external agencies such as health service providers. The University will take every care in ensuring that providers are advised of requirements in advance and in securing placements for all students at the requisite time. However, we seek to ensure that both students and Clinical Educators are made aware that circumstances beyond the reasonable control of the University may occur that mean, as a result of changes within the Health Service or personal factors, it is not possible for providers to meet placement requirements or students to attend placement. The placement providers will need to notify the University (Placement Co-ordinator and/or Link Lecturer) as soon as possible if this is the case and the University will seek to inform the placement area if the student is not coming on placement. In such circumstances, the University will make its best efforts to organize alternative arrangements for students to meet the requirements of their programme, (including identifying suitable alternative placements wherever possible), however students should be aware that it is possible that the completion of their programme may be unavoidably delayed and/or that the alternative arrangements put in place may cause some inconvenience. In such circumstances if students do not want to accept the alternative arrangements they would be entitled to terminate their studies and receive appropriate recognition of their academic achievements. It is therefore essential that as a Clinical Educator you advise your allocated Link Lecturer from the University when problems supporting students arise. You may also wish to consider informing your local Education Coordinator within your Trust and the Placement Co-ordinator at the Plymouth University. If the situation adversely affecting the student is beyond their control there may also be an opportunity for the student to submit extenuating circumstances. If so, this would require the student to contact their Personal Tutor/Module Tutor/Programme Lead to discuss the situation. You may wish to contact the academic Link Lecturer to alert them to the situation also as if it is an appropriate action it may need supporting evidence to be supplied by the placement area or the Clinical Educator. BSc (Hons) Podiatry Clinical Educator Handbook 2015 9 2.2 Placement Learning Placement experience forms an integral part of the programme, providing the opportunity to integrate academic, practical and interpersonal aspects of podiatry and develop problem solving skills and reflection abilities. Changes in health care provision have resulted in a widening range of work environments and increasing interprofessional working for the podiatrist. It is therefore essential that the modules containing professional practice elements and their associated learning outcomes reflect this trend, providing the clinical experience required for registration in a diverse variety of settings. Learning outcomes are recorded in the Practice Portfolios that are sent out to each practice area and reviewed annually with Clinical Educators. If you have any further feedback you wish to contribute then the team would welcome your contribution. Please contact either your academic Link Lecturer or Sally Abey (Placement Coordinator). 2.3 Absence from Practice Students are responsible for notifying the Clinical/Placement Area and Plymouth University via the Programme Administration Office (01752 588800/01752 588833) at the Peninsula Allied Health Centre, that they are unable to attend due to sickness. The Programme Administration office is staffed from 0830-1700 and there is an answer-phone for hours outside this time. If a student is absent without notifying the clinical placement area the Clinical Educator should notify their line manager and the Plymouth University and ensure their absence is recorded in the Portfolio Attendance Record (Appendix 2) and on the timesheet before countersigning. If the lack of notification is persistent and the student fails to respond to feedback regarding the need for notification, the Link Lecturer should be informed as it is vital the student understands this is not professional practice and the disciplinary procedure can be discussed. 2.4 Timesheets Students are required to complete and submit timesheets on a monthly basis to the appropriate Programme Administration office (Appendix 3). Timesheets are required to ensure students meet the requirements for registration, and are reviewed regularly Clinical Educators must check the form for accuracy and sign these timesheets as confirmation that the student has undertaken the identified clinical placement sessions. An attendance record has been included in the portfolio to assist with the check (see Appendix 2). 2.5 Incidents in the Clinical Area BSc (Hons) Podiatry Clinical Educator Handbook 2015 10 Guidelines for the management of incidents that occur during undergraduate student placements are available in Appendix 4. There may be an occasion when a student is a witness to an incident in the clinical area. The student should seek assurance that an initial discussion is informal and confidential so that the issues can be explored without fear of repercussion. During this discussion it is possible to examine any professional issues that may arise and the resultant professional duty. If the process to deal with the incident is required to go further, the academic Link Lecturer should be informed immediately and the student should be encouraged to raise this with their Clinical Educator if they have not done so already. The Link Lecturer or another member of academic staff will attend the placement area as a matter of priority (or through negotiation of a timeframe) in order to support the student and advise them on how to prepare a statement, if it proves necessary, and what is involved if they are asked to be a witness. If this situation transpires, it is important that the student is supported by a member of the Faculty’s academic staff as they can feel very vulnerable despite previous life experience, so they should be directed to also contact their personal tutor in the interim. Any resultant Reflective Report cannot be used as a statement/evidence without the student’s consent (on advice from the University) as it is marked ‘Private and Confidential’. 2.6 Reporting Incidents/Accidents Any incidents that occur to the student on placement that may require support in the longer term should also be reported eg High risk inoculation injuries, work related injuries, contraction of a communicable disease. If this has been recorded in a Trust Accident/Incident Report we will need the reference number for the report. The Incident Record Form (Appendix 5) must be completed and replica information emailed to the student’s personal tutor so that they can liaise with the Clinical Educator to make certain they are receiving suitable support on placement. The student is also directed to highlight it to the personal tutor when they next meet to ensure that the University can make certain they continue to receive suitable support on their return to the University. 2.7 Placements Students who feel that their placement allocation is a cause for concern for personal reasons (e.g. attending their own GP practice for long term treatment) are advised to discuss the situation with the Placement Co-ordinator and their personal tutor prior to the placement where possible, or with their Clinical Educator at the beginning of the placement if it has been BSc (Hons) Podiatry Clinical Educator Handbook 2015 11 timetabled without their prior knowledge, so that an alternative placement may be arranged. An alternative placement may need to be arranged over the summer period after the academic year where relocation is required at too short notice to be accommodated. 3. THE ROLE OF THE CLINICAL EDUCATOR 3.1 Your role as a Clinical Educator plays an essential part in facilitating students learning as they gain the knowledge and skills necessary to register with the Health and Care Professions Council. Students need to be allocated a named Clinical Educator for each practice experience. The Clinical Educator will be an appropriately qualified professional and has professional responsibility for facilitating learning, supervising and assessing the student in the practice setting. 3.2 You will work alongside the student in the practice environment or outline learning outcomes and then receive feedback from other healthcare professionals who the student is working with, and judge their proficiency against set learning outcomes at particular points in the programme. 3.3 Assessment of the student’s ability to practice to the required standard is achieved through the relationship involving the student and the practitioner as Clinical Educator. The Clinical Educator is the professional who makes the decision about whether the student is safe in practice. The Clinical Educator is supported by the Link Lecturer where requested or can obtain alternative or additional academic support from the Podiatry Team or the Placement Co-ordinator from the Programme Team at the Plymouth University. 3.4 In order to obtain information on the name of the student’s personal tutor, please ask the student or contact the Placement Co-ordinator for the Podiatry Programme. 3.5 The criteria for identifying Clinical Educators are set out in Appendix 6. BSc (Hons) Podiatry Clinical Educator Handbook 2015 12 3.6 Summary of the responsibilities of a Clinical Educator in the assessment of practice of a student Clinical Educator is responsible for arranging to attend a Clinical Educator training session (or equivalent) on the relevant assessment of practice method and documentation. This may be arranged by liaising with the Placement Coordinator, academic Link Lecturer or Education Co-ordinator for the area. Practice area informed of student placement (where possible a minimum of eight weeks before the start of the placement) via the ARC system and their Clinical Educator for the placement should be identified The student contacts the Clinical Educator ideally more than eight weeks before the start of the placement with completed Student Profile (see Appendix 7). Duty rota agreed/assessment of practice discussed. Student undertakes a self assessment and sends Learning Contract (Appendix 8) to Clinical Educator. Student and Clinical Educator negotiate a learning contract/agreement based on module learning outcomes, self-assessment by student and placement opportunities. This should occur prior to the start of the placement where possible or during an initial tutorial. Timings for formative and summative assessments are agreed in line with programme requirements. Details of meetings with the Clinical Educator should be recorded on a Tutorial Form (Appendix 9). Clinical Educator arranges contact time with the student. The Clinical Educator may identify a co-educator and other professionals from the healthcare team to contribute to the assessment of practice and facilitate learning as appropriate. Formative review of student is undertaken (minimum of one review during experience, more than one recommended). Feedback is recorded in the Practice Portfolio (see Appendix 10). Learning Contract/agreement updated. Any continuing problems are referred to the University Link Lecturer or Placement Co-ordinator as appropriate. Summative (final) assessment is undertaken after the student has had the required amount of experience and has undertaken one or more formative reviews. The assessment must be completed by the specified submission date. Evidence supporting achievement of a Learning Outcome should be collated by the student and reviewed by the Clinical Educator signing off the Learning Outcome (eg. Reports from Others (Appendix 11), Reflective Reports (Appendix 12), Patient Feedback Form (Appendix 13)). Documentation must be completed and signed in line with programme requirements (see Learning Outcome Record Sheet, Appendix 14). Any problems should be referred to appropriate member of the academic staff prior to this stage where possible. The student is responsible for submitting the documentation. BSc (Hons) Podiatry Clinical Educator Handbook 2015 13 A Mid-Point and End of Placement review meeting should take place and be recorded in the portfolio (Appendices 15 and 16) so that the student can self assess and have a record of progress provided by the Clinical Educator also to show their Personal Tutor during the review periods between placement blocks. This will facilitate discussion around any points of concern or highlighted excellent practice that the student has demonstrated whilst on the placement up to that point. Where feedback is not provided formally the personal tutor will be solely dependent on the student’s report and will not be able to discuss any issues other than those the student chooses to relay. It is preferable that a 360° perspective can be provided through feedback from student, Clinical Educator and patients so issues can be examined in more depth. It is strongly recommended that Clinical Educators have a formalised support system when undertaking their role, and receive ‘feedback’ on their effectiveness through, for example, the NHS appraisal system, student and peer review, comments from external examiners or support from the Plymouth University Link Lecturer for the area. 3.7 Allocation of Clinical Educators Where possible the practice area is informed of a student placement at least eight weeks before the start of the experience. A Clinical Educator is identified who fulfils the criteria for the role and is familiar with the programme/module content and assessment of practice strategy. The clinical placement area identifies the named Clinical Educator for the student placed in their clinical area. The student is responsible for contacting the Clinical Educator, where possible, at least eight weeks before the contact deadline i.e. eight weeks prior to placement for an exchange of information. The Clinical Educator should discuss the clinical profile and timetable of the placement and discuss the learning opportunities available with the student. BSc (Hons) Podiatry Clinical Educator Handbook 2015 14 4. TEACHING AND LEARNING STRATEGIES USED IN THE PROGRAMME 4.1 The theoretical content of the modules of the Podiatry programme is intended to provide the student with the underpinning knowledge associated with practice. 4.2 Teaching and learning in practice will reflect the novice point at which many students enter the programme. Methods such as observation, supervised practice and indirect supervision of practice will be utilised to guide the student towards gaining confidence and competence as a practitioner. 4.3 The teaching and learning strategies will: 4.4 place practice centre stage facilitate the integration of theory and practice be based on the notion of students accepting responsibility for their own learning be based on students’ active involvement in their own learning, such as enquiry based and problem based learning establish the principle of lifelong learning include interactive, collaborative/shared learning, involving other professions, disciplines and agencies Facilitate student achievement of the outcomes/proficiencies. Self Assessment and Self Awareness Self assessment gives students ownership of their learning and responsibility for learning experiences and achievements. Self assessment is to be encouraged on a regular basis in an informal manner with a Clinical Educator, clinician, or personal tutor. Self awareness is key within the reflective process to recognise personal strengths or learning needs and the students should be encouraged to reflect more formally in order to receive feedback and therefore develop the necessary reflective skills for continuing professional development. 4.5 The Programme is a three-year, modular Honours Degree course that incorporates the principles of proficiency-based assessment for the practice learning outcomes. 4.6 Each year comprises approximately 40 weeks of study, and is divided into two terms; term one operates from September to January and term two operates from February to July. 4.7 The programme is designed to emulate the patient/practitioner interaction, which takes place during a period of care. Themes are developed across the three levels of the programme. The BSc (Hons) Podiatry Clinical Educator Handbook 2015 15 theme of Year 1 is the assessment of health care needs; Year 2 focuses upon treatment; Year 3 on the evaluation of effectiveness of intervention. Thus the cyclical processes of the patient management are reflected: assess, treat, evaluate. 4.8 Practice experience is allocated throughout the three years to enable students to achieve the Health and Care Professions Council Standards of Proficiency as indicated within the practice portfolio. Clinical practice is organised into five blocks of differing duration. The first year contains one clinical block in term two, while the second and third years each contain two clinical blocks, one in each term. Year one clinical teaching occurs within the University training clinic environment, ensuring students have practical experience with patients before attending placements in Year two. Year two has longer clinical blocks in order to facilitate the application of skills in the NHS environment to a suitable level to allow successful students who may interrupt their studies to practice as a Band 4 practitioner (under supervision). Year three clinical blocks are arranged so that they may refresh their skills and study the environment more deeply prior to their theory modules at the beginning of the academic year and attend placement again when nearing completion of the year to consolidate their practice and theory in the professional setting in preparation for employment. 4.9 During each placement, the students will have ‘supernumerary status’. This means that, throughout the three-year Programme, they are part of the care team but additional to the allocated staff complement. The student is therefore able to take full advantage of all the learning opportunities and to undertake the assessment of practice. 4.10 Each module of the programme focuses on a particular area of theory and practice. The student’s knowledge and proficiency in the learning outcomes will be summatively assessed. Students are required to pass all the theory assessments and demonstrate proficiency in the practice learning outcomes that are identified in the Practice Portfolio. 4.11 By the end of the programme, all proficiencies (in accordance with the requirements of the Health and Care Professions Council (HCPC) Standards of Proficiency, Standards of Education and Training and the Quality Assurance Agency (QAA) Benchmark Statements for Podiatry (Appendix 17), will have been demonstrated through assessment prior to registration 4.12 These proficiencies are clustered into four domains namely Professional, Clinical, Communication and Interprofessional. BSc (Hons) Podiatry Clinical Educator Handbook 2015 16 5. WHAT HAPPENS IN THE BSc (HONS) PODIATRY PROGRAMME YEAR 1 5.1 Year one lasts one year and consists of two terms (Autumn and Spring/Summer). 5.2 During Year One students receive mandatory training in Fire safety, Equality and Diversity, Mental Capacity Act, Basic Life Support and Manual Handling, at different points throughout the year in readiness for going into the clinical environment in the final term. 5.3 The broad aim of the term one modules is to develop the core generic knowledge and skills required for professional practice. There is a focus is on inter-professional collaboration, highlighting shared and generic skills required for contemporary health and social care practice. This is achieved through the delivery of modules shared with cognate groups of all the professions within the Plymouth University School of Health Professions: Dietetics, Operating Department Practitioners, Optometry, Occupational Therapy, Paramedicine, Physiotherapy and, of course, Podiatry. This is achieved throughout the delivery of SOHP101: Preparation for Professional Practice and SOHP103: Functional Human Anatomy and Physiology. 5.4 During term one they are prepared for podiatric practice through attendance on the module POD106: Podiatric Studies 1. Through this module the students learn about assessing the patient (basic psychosocial and pharmacology), the structure and function of the skin and associated structures and how circulation and sensatory ability is assessed. 5.5 The aim of term two is to build on term one studies and enable students to develop clinical reasoning skills in patient/client assessment, building knowledge and understanding of the structure and function of the human body and the pathological processes relevant to podiatric practice. This is delivered in the module POD107: Podiatric Pathology, which links the normal functional and physiological anatomy learned in Term one with the pathologies that can occur. 5.6 During Term two students will also be working in the Skills Laboratory acquiring the necessary clinical skills to be able to treat patients in the final stage of the academic year. Students will undertake rudimentary patient/client management in a controlled supervised environment for POD108: Podiatric Practical Skills. This will involve applying the concepts involved in professional practice . Treatment skills are introduced for a range of conditions and the planning, selection and evaluation of appropriate podiatric techniques explored at a basic level. The BSc (Hons) Podiatry Clinical Educator Handbook 2015 17 students build a foundation for clinical work with patients with a variety of disorders. 5.7 The final part of the year introduces students to clinical practice in the module POD104: Podiatric Clinical Practice 1 where practice is undertaken treating patients in the Training Clinic (the Local Care Centre (LCC), Mount Gould, part of Plymouth Community Healthcare CIC). This provides the student with opportunities to apply first year learning in a professional practice setting. YEAR 2 5.8 Year two lasts one year and consists of two terms. 5.9 The aim of the second year is to enable students to develop approaches to podiatric interventions and apply clinical reasoning skills in the management of specific client groups using a life span approach. The emphasis will be on the development of the professional identity and expertise within the context of interprofessional practice in health and social care settings. The ethos of a research culture and study of the disciplines that inform podiatric practice continue within this level. 5.10 Theory based modules POD207: Systemic Disorders and the Lower Limb, POD212: Podiatric Studies 2, and POD215: Podiatric Studies 3 seek to develop the student’s theoretical knowledge base through the study of lower limb, foot and ankle disorders in young people and adults and older people respectively. Through the use of case studies throughout the year they build the students’ knowledge of a range of therapeutic modalities and develop skills in managing disorders of the lower limb foot and ankle in the context of best/evidence-based practice. 5.11 Relevant National Service Frameworks are reflected in the indicative syllabus content of these modules. 5.12 At this stage students will also undertake the module SOHP201: Project Studies which will enable them to develop a sound understanding of research terminology, methodology and develop the necessary skills for evidence-based learning and lifelong learning. 5.13 During year two students will have a nineteen week clinical practice block. This will be divided into two blocks with placements in different areas Each of the placement blocks will be divided into two sections so that students can have a midpoint review with their personal tutor following their mid-point review with their Clinical Educator (week four/five in a BSc (Hons) Podiatry Clinical Educator Handbook 2015 18 placement) and later return for end of placement reviews and assessments at the end of each block. This will enable them to have a suitable time period to develop their skills working under supervision in an interprofessional clinical setting. During this time they will be compiling evidence in their portfolio. This should be of a suitable standard that they would be able to practice at a Band 4 (Knowledge and Skills Framework, 2004) level should they need to step off the programme following completion of this stage. YEAR 3 5.14 Year three lasts for one year and consists of two terms. 5.15 The emphasis in the third year will be on professional mastery and fitness for practice and purpose within client centered, interprofessional health and social care settings. Knowledge and context is now more specialised and requires higher level skills of synthesis, analysis and evaluation. 5.16 POD311: Pharmacology for Podiatry enables the student to critically evaluate the role of pharmacological management within the relevant pathologies whilst obtaining knowledge and understanding of pharmacological principles. This is complemented by further study of pathologies related to the high risk patient in the delivery of POD316: The High Risk Patient in Podiatric Practice. 5.17 POD315: Local Anaesthesia and Nail Surgery introduces and develops students’ knowledge and practice within the field of nail surgery. Clinical reasoning and critical reflective skills are elaborated to effectively achieve this module and therefore obtain the Certificate of Local Anaesthesia. 5.18 The clinical placement block of year three, term one is comprised of the clinical module POD319: Podiatric Clinical Practice 4, providing the student with the opportunity to develop the clinical management skills to care for patients presenting with complex and unpredictable medical and surgical disorders. This encourages the student to synthesize acquired knowledge and apply this to podiatric practice and inter-professional collaboration. 5.19 The research module SOHP301: Project Studies 2 is ongoing throughout the third year. The students will be using the opportunity to investigate an area of particular research interest and demonstrate their ability to develop an in-depth and comprehensive research proposal. 5.20 SOHP302: Preparation for Professional Practice is a module that the students will study alongside the other healthcare BSc (Hons) Podiatry Clinical Educator Handbook 2015 19 professions. The aim of this module is to develop the application of management, leadership and inter-professional working within the context of a wider healthcare environment to improve the quality of care. As part of this module profession specific sessions will also be delivered to examine the legal, financial and ethical issues and evolving policy agenda currently impacting on the management of podiatric practice, both private and NHS. 5.21 The final clinical module POD320 Podiatric Clinical Practice 5 provides opportunities for the student to consolidate their practice as an autonomous interprofessional holistic practitioner within a variety of healthcare settings. It explores the wider issues of professional practice within the context of contemporary organisation and delivery of health and social care whilst enabling the student to refine their self-awareness, communication and practice skills prior to their final exam which will enable them to apply for registration with the HCPC on graduation. A particular skill that will be consolidated during this placement would be Nail Surgery following completion of the module POD315. CLINICAL PLACEMENT 5.22 There is a positive correlation between students’ necessary opportunity to gain experience and time spent on placement. The increased amount of time spent in placement setting in the second year enables the student to gain proficiency in the practical skills and understanding enabling them to work as an Assistant Practitioner after completion of the second year, should this be necessary. In the third year of study, the student spends time at the beginning of the year refreshing their skills and reflecting on the roles and responsibilities of the autonomous practitioner, preparing for the development of their patient and practice management skills. These skills are consolidated, linking theory and practice later in the year whilst on their final placement prior to their final exams. Practice experience is shared equally between the Plymouth University/Plymouth Community Healthcare (CIC) training clinic and time spent out on placement at NHS Trust clinics within the NHS Southwest region. The placement locations within the Trust should vary each time students are on placement to provide a variety of experience and exposure to specialisms. When not in the placement setting students will still be receiving clinical training at the training clinic allowing further skills to be taught and practiced. During the clinical block of term one at year two, students will engage in practice following completion of the theory modules POD207 Systemic Disorders and the Lower Limb and POD212 Podiatric Studies 2 which should therefore inform their BSc (Hons) Podiatry Clinical Educator Handbook 2015 20 understanding of practice. The second term begins with another clinical block allowing students to consolidate their skills in a different clinical environment, reflecting on any differences and developing an appreciation of organisational divergence. This will be further consolidated on the completion of the theory module POD215 Podiatric Studies 3 following their completion or the placement. In year three it is anticipated that students will gain the majority of their complex clinical experience within placement settings although they will still be treating patients in the training clinic when not in placement. They will also receive the initial training for their nail surgery within the minor surgery unit of Plymouth Community Healthcare (CIC). The clinical block of year three term one is comprised of the POD319 Podiatric Clinical Practice 4 module. The clinical block within term two of this Level is comprised of the clinical module POD320 Podiatric Clinical Practice 5. Both of these modules seek to encourage the student to reflect on their development of practice as an autonomous, holistic, inter-professional practitioner. 5.23 Prior to undertaking each placement learning experience, students will have received a verbal and written briefing on the placement process, their annual mandatory training and a verbal briefing outlining roles, responsibilities and expectations of both learners and facilitators of learning during the placement. Students will be encouraged to attend a tutorial to ensure they have a clear understanding of their learning goals and are duly prepared. BSc (Hons) Podiatry Clinical Educator Handbook 2015 21 6 AS A CLINICAL EDUCATOR, WHAT DO I NEED TO KNOW, IN GENERAL TERMS, ABOUT THE ASSESSMENT STRATEGY? 6.1 The assessment of theory and practice is designed to test the ability of the student to apply theory to practice, and to use practice experiences to verify or challenge theory and practice. 6.2 The assessment strategy places equal emphasis on achievements in theory and practice. 6.3 Assessments demonstrating the progression towards the academic award and proficiency in practice are submitted to the appropriate Award Assessment Board at the end of each programme year. What is the purpose of formative assessment? 6.4 The aim of planned formative assessments is to review with the student their strengths and weaknesses and provide them with constructive feedback on their performance. Plans can then be agreed on how to maintain their strengths and improve on their weaknesses. 6.5 The performance of the student in practice needs to be monitored and assessed regularly over the three-year period. Feedback needs to be provided to help the student to progress, and act as a guide towards achievement of the learning outcomes of each module. Where possible this should be recorded in the practice portfolio so that it can be accessed by the personal tutor and other professionals providing support for the student. If there should be an appeal against a verdict then the documentation is required to demonstrate that the assessment and feedback process was correctly followed and the student was correctly supported. 6.6 Formative assessments can occur at any agreed point during a placement at an agreed time that should be recorded within the relevant paperwork within the portfolio. Once the student is satisfactorily prepared for repeated competence then a summative assessment can be planned. 6.7 Formal acknowledgement that this has occurred is recorded on at least one occasion for each module using the formative assessment of practice documentation. 6.8 If a student consistently fails to modify their practice in relation to formative feedback, the Link Lecturer should be informed as this would suggest the student may fail and support mechanisms for the Clinical Educator and student may need revision. BSc (Hons) Podiatry Clinical Educator Handbook 2015 22 What is the purpose of summative assessment? 6.8 The aim of the summative assessment is to meet with the student to identify whether they have successfully achieved the practice learning outcomes set for the module. This is done through reviewing the evidence to support each performance criterion or capability. 6.9 The Clinical Educator, using their professional judgment, decides if the student has achieved or not achieved the required standard. 6.10 No grade is awarded but the student should receive both verbal and written comments about their performance. Excellence should be acknowledged, but the student also needs to be made aware of weaker areas of practice. 6.11 Summative assessment will normally have taken place by the week before the end of the placement. If both Clinical Educator and student agree, summative assessment can be undertaken after the student has had three weeks in the experience. 6.12 The placement period does safeguard the rigor of the process of assessment by allowing time for a student to benefit from formative feedback before a final summative assessment. 6.13 The student should advise you of the submission date(s) for each module in order to ensure that any outstanding paperwork can be provided in time. 6.14 A student who is weak in any performance criterion/capability should not be summatively assessed until an agreed contract date that allows them the maximum opportunity for formative assessment prior to the submission date. This ensures maximum time for the student to develop the skills, gather the required evidence of competence and achieve their potential. 6.15 Once summative assessment has been conducted the result of the assessment should be recorded in the portfolio so that it is apparent that the student has been assessed and has not achieved. 6.16 The student needs to achieve a pass in the all aspects of the assessment of practice to achieve accreditation for the module. This may include some written work (e.g. case study, reflective report) that will provide a mark for the module. Where either portfolio or coursework is not accomplished the placement may need to be retaken. BSc (Hons) Podiatry Clinical Educator Handbook 2015 23 6.17 The decision of the Clinical Educator concerning assessment of learning outcomes is final and where possible must be supported by suitable evidence. 6.18 The results of summative assessment of practice are presented at the appropriate Award Assessment Boards at the end of Year 1, Year 2 and Year 3. Any appeals will be considered under the Plymouth University regulations 6.19 The student will have two attempts at each practice module. A failed clinical module may not normally be repeated on more than one occasion. Why have both formative and summative assessments in practice? 6.19 A student’s progress should be incremental. If you, as Clinical Educator, or the student are concerned about their progress, the Link Lecturer must be contacted without delay. They will discuss the situation, and be available for support and advice. The Link Lecturer will also be available for support and if required a visit will be arranged. 6.20 Similarly the Link Lecturer should be contacted if there are aspects of a student’s attitude, performance or behaviour that does not easily fit within the learning outcomes of a module OR cause concern in any way with regards to safety in practice, behaviour or attitude. 7. THE ASSESSMENT OF PRACTICE PROCESS WITHIN THE BSc (HONS) PODIATRY PROGRAMME 7.1 Modules within the BSc (Hons) Podiatry Programme have specified learning outcomes that are assessed in practice. Each learning outcome is assessed through performance criteria, or capabilities, that specify the quality of what needs to be achieved. 7.2 The student can gather evidence, which proves to others that the learning outcome has been achieved, in a variety of ways: 7.3 Direct observation Questioning, oral or written Statements from others Simulation Evidence products of the student’s work Reflection It is expected that direct observation will normally be the main method of gathering evidence for each performance criterion, or capability. BSc (Hons) Podiatry Clinical Educator Handbook 2015 24 8. 7.4 Direct observation, to assess the proficiency of the student, can be undertaken by the Clinical Educator or an agreed member of the multi professional care team (e.g. physiotherapist, district nurse). The Clinical Educator then makes a judgment and initials the appropriate box on the Learning Outcome Sheet (Appendix 14). Details from assessors other than the Clinical Educator can be recorded on the placement record ‘Reports from Others’ provided in the portfolio if brought to the session by the student (Appendix 11). This can be encouraged where members of other professions are working with the student. 7.5 With the agreement of the Clinical Educator, judgments may be made based on ‘statements’ from others involved in the care of the patient/client (health care assistant, physiotherapist, practice nurse). The student is required to provide written evidence of proficiency for the Clinical Educator, who can initial the appropriate box(es) of the summative assessment form if the relevant performance criteria are achieved. 7.6 Students are encouraged to reflect on their experiences in practice. The reflections can be oral, diagrammatic, or written accounts. The latter may form part of a reflective journal. 7.7 Written evidence is stored in a Practice Portfolio. The student is responsible for collecting their evidence of proficiency and maintaining the Practice Portfolio. All evidence is crossreferenced by the student to the learning outcomes. 7.8 The student is responsible for making the evidence in the Portfolio available to the Clinical Educator throughout the placement as well as at assessment points. WHAT IS THE PRACTICE PORTFOLIO? 8.1 The Practice Portfolios provide a comprehensive record of the student’s learning and achievements throughout their three years of the Programme. The Portfolio is also central to the assessment of practice. 8.2 The student is expected to take responsibility for his or her own learning from the beginning of the programme. Regular updating of their Portfolios ensures that evidence is collected to support the achievement of proficiency in the modular learning outcomes. 8.3 The purpose of the Practice Portfolio is to provide a record of the students different stages of professional development towards eligibility for registration with the Health and Care Professions Council and develop the ethos of Continued Professional BSc (Hons) Podiatry Clinical Educator Handbook 2015 25 Development. It is a comprehensive record of the students learning achievements in practice throughout the three-year BSc (Hons) Podiatry programme. Theory and practice are closely linked and the material that is collected in the portfolio, for example reflective accounts, will provide opportunities for students to identify the links between the theory and practice. 8.4 The Practice Portfolio consists of and will require evidence of: 8.5 Application of theory to practice Acquisition of clinical skills Achievement of the proficiencies of a podiatrist Development of communication skills Interprofessional working Clinical experiences and reports from Clinical Educators/supervisors/ tutors/patients Completion of statutory requirements Ability of students to take responsibility for their own learning needs and achievements Students are responsible for compiling and maintaining their Practice Portfolio so that their progress in acquiring the necessary knowledge, skills and attitudes of a podiatrist can be demonstrated. It will be reviewed regularly by the student, the Clinical Educator/supervisor and personal tutor/Link Lecturer. The Portfolio is also the focus for the assessment of practice and is therefore an extremely important file of documents that will be presented at Subject Assessment Panels and Award Assessment Boards. 8.6 Confidentiality Students must ensure that all due consideration is given to the confidentiality of the material included in the file; patient details should not be included in the first instance and Trust documents should be anonymised. 8.7 Preparatory sessions held at the beginning of the year will remind students how to prepare for placement and use their portfolio and sessions will be held prior to the placement to help students prepare their documentation. 8.8 The portfolio provides explanatory sections for the documentation and each portfolio contains the learning outcomes that must be achieved during placements throughout the academic year. The Practice Assessment Document provides a record of students ongoing progression and achievement. You and your student must complete a summative assessment of practice at BSc (Hons) Podiatry Clinical Educator Handbook 2015 26 points agreed by both parties. The stage tutor/module teacher will provide students with the dates for submission of the completed portfolio. All learning outcomes within the portfolio should be assessed as “Proficient” by the submission date in order for the student to progress on the course and ultimately be eligible for registration as a Podiatrist with the HCPC. Continuation sheets are provided to attach to the Practice Assessment Document if you wish to record extra comments. The Profile of Clinical Proficiencies (Learning Outcome Record Sheet, Appendix 14) enables students and their Clinical Educator/supervisor to identify the proficiencies and the learning outcomes to be achieved in practice. Students’ progress towards achieving proficiency is self-assessed and discussed with their Clinical Educator during formative and summative assessments. 8.9 Year 3 portfolios will contain a log to record the local anaesthesia and nail ablation procedures students have undertaken at Year three. Students are required to log and administer proficiently a minimum of four local anaesthetic injections and perform a minimum of four nail surgery procedures. If students fail to achieve this they are unable to register with the Health and Care Professions Council. 8.10 The portfolio contains the Mandatory Experience Log and records the experience undertaken in each academic year. It is the student’s responsibility to get the Mandatory Experience Log needs to be signed and dated by a member of the University staff. 8.11 Records should be kept by the student and staff member of tutorials that are provided. These will be provided as a separate document and should record what was discussed and any identified outcomes from the discussion. This will act as a reference document for others who may subsequently work with the student if a Clinical Educator should go on sick leave and evidence of what was agreed if there is any dispute. This should be jointly signed by the students and the Clinical Educator to demonstrate the agreement. A Signature Record (Appendix 18) provides details of all Clinical Educators/supervisors involved in assessing students’ proficiency in practice in each clinical placement block. The record is submitted as part of the portfolio at the end of each practice experience. BSc (Hons) Podiatry Clinical Educator Handbook 2015 27 A Student Experience Record Sheet (timesheet) (Appendix 3) is used to record time spent by students in both theory and practice and students are required to submit these on a monthly basis to the programme administration office. Timesheets are necessary to ensure students meet the requirements for registration and are reviewed regularly by the academic team. The experience record is therefore a very important document and must be checked, completed and signed by the student and countersigned by their supervising Clinical Educator/supervisor during each period in the Local Centre Centre, skills laboratory or clinical practice placement. The Attendance Record (Appendix 2) should be referred to for accuracy on placement. The Practice Feedback Form is submitted with the Practice Portfolio at each summative point. A Practice Feedback form must be completed for each module with practice learning outcomes being assessed. This is obtained by the student form Programme administration office and does not require a Clinical Educator signature. 8.12 The portfolio will include selected reflections of chosen by the student from their personal reflective journal, and reflections submitted for summative assessment. Students must ensure that confidentiality of information about staff, patients and placement areas is maintained. 8.13 The Portfolios therefore provide evidence of the development and performance of the student, from novice to practitioner. The practice assessment will identify skills that have been achieved, and also any areas that need further development. 8.14 The student will maintain their Portfolios throughout their practice allocations. You are advised to review the content when the student first begins their practice experience, when agreeing a learning contract as well as at formative and summative assessment points. NB. All students undertaking programmes delivered by the Faculty of Health and Human Sciences are reminded that any alteration to University documentation, including practice portfolios, involving forgery/falsification of a Clinical Educators comments or signature/initialling will be investigated. This investigation could lead to disciplinary action, which may lead to a student’s being unable to achieve professional registration. BSc (Hons) Podiatry Clinical Educator Handbook 2015 28 9. HOW DOES THE ASSESSMENT STRATEGY WORK IN PRACTICE? 9.1 Each student should be allocated a placement Clinical Educator during each Practice experience. 9.2 A Tutorial Form (Appendix 9) should be used to keep a record of meetings and action plans or outcomes derived from the discussions. 9.2.1 Clinical Educators should establish how disclosures by students are to be addressed before meeting with students. Reflective reports are headed ‘Private and Confidential’ and cannot be used as evidence without further consultation with the Plymouth University. Students are advised not to identify staff by name where they seek advice regarding observed practice and cannot be used as witnesses without having spoken with the Link Lecturer beforehand and following consultation with the Plymouth University solicitors. 9.3 Before the placement the student should be provided with a timetable that indicates the learning opportunities. They should formulate a learning contract indicating when they would intend undertaking the different stages of assessment and the preferred method of assessment. They should then make this available to the Clinical Educator prior to the placement. At the beginning of the placement you and your student should meet to review their learning contract, any previous practice experience, and learning outcomes for the modules. Possible opportunities and forms of evidence to demonstrate achievement will be discussed. From this initial review, you and the student will agree an informal learning contract within the tutorial record, agreeing learning strategies, what evidence is to be generated and when formative assessment(s) will take place. This learning contract is an obligatory part of the formative assessment of the student. 9.4 In exceptional circumstances you may identify, when agreeing the learning contract with the student, that the practice experience may not provide the opportunity to achieve all of the learning outcomes. It is the responsibility of the student to contact the module teacher, who will make a decision about what course of action to take. When timetabling the placement a maximum period of a week should be arranged for observation only at the beginning for the student to acclimatise. Beyond this time the student should be participating in practice unless the specialism prevents it. BSc (Hons) Podiatry Clinical Educator Handbook 2015 29 9.5 The student should have planned formative assessments at agreed points during each placement. Using the feedback sheets both the student and you will review their progress, based on evidence already collected during the experience. Discussion will guide the student towards achieving the learning outcomes, and the learning contract is updated and recorded on the tutorial record. 9.6 Summative assessment is normally completed by the last week before completion of the placement. You, as Clinical Educator, are responsible for reviewing all the evidence of proficiency provided by the student. The evidence may include any reflective accounts produced by the student as part of their assessment of theory for the modules being assessed during the placement. The module teacher is responsible for marking the reflective accounts or case studies linked to the relevant modules. 9.7 All performance criteria/capabilities within a learning outcome must be attained for the student to achieve a pass for each element and the Portfolio overall. No grading is attached to the achievement but verbal and written feedback to the student will facilitate their progress. 9.8 The Clinical Educator will record on the summative assessment form (under ‘not achieved’) if the student has not achieved a performance criterion due to extenuating circumstances, for example assessor off sick, or clinic closure. The student must inform the module teacher for the relevant module and discuss the submission of extenuating circumstances where applicable. 9.9 On rare occasions a student may demonstrate poor standards following the successful achievement at summative assessment. The Clinical Educator cannot change the documentation but must give a detailed account in the feedback of the summative assessment to enable the Podiatry lecturers to discuss this with the student. The Link Lecturer must also be informed. 9.10 It is the responsibility of the student to submit it to the Programme Administration office at the Peninsula Allied Health Centre by the required date for ratification by the appropriate Award Assessment Board. 9.11 The student is responsible for keeping a permanent record of the evidence gathered for each learning outcome. The evidence must clearly state to which learning outcome(s) it can be applied. The evidence is stored in their Practice Portfolio, and must be available at all assessment points of the three-year Programme. BSc (Hons) Podiatry Clinical Educator Handbook 2015 30 9.12 If a Clinical Educator is encountering difficulties with their assessment of a student’s criteria/capability they should seek advice from the Link Lecturer. The academic team remain available to support Clinical Educators at all times. 9.13 Where a student does not achieve all learning outcomes by the end of the module they will have their submission classified as a Practice Fail. All students are allowed one resit opportunity for practice modules and so may subsequently have the opportunity to achieve the module and progress. The manner in which this is undertaken is decided by the Assessment Board which meets each summer. BSc (Hons) Podiatry Clinical Educator Handbook 2015 31 10 SUMMARY OF THE ASSESSMENT PROCESS Clinical Educator Allocated to the Student Student contacts Clinical Educator Clinical Educator sends induction pack and timetable for placement Student develops learning contract and sends to Clinical Educator Start of Experience Meet the student Review Practice Portfolio to date Discuss all the placement opportunities and review the experiences/resources available Review the learning objectives with the student (learning outcomes) Discuss evidence which will be gathered by the student to demonstrate their achievement of the learning objectives Learning contract agreed and recorded on Tutorial Form During the Experience At planned points during the placement: Review Practice Portfolio and students’ progress towards achieving their learning objectives for the placement. Review progress in the assessment of practice and written evidence in the Portfolio (e.g. management plans, reflections). Agree what still needs to be achieved, and how. Formative assessment of progress is documented, and learning contract updated Mid-point review completed Personal tutor has tutorial with student to review learning achievement and plan By the Final Week of the Experience or by the Assessment Submission Date whichever is earlier Review the learning contract, and all evidence to support achievement of each performance criteria/capability The assessment grid of each learning outcome sheet is completed. Assessors who are not the Clinical Educator must have recorded their details on the Placement Record End of placement review completed The student checks the documentation is complete and submits the summative assessment of practice module record to Programme Administration by the published date NB: The student may produce the evidence to demonstrate proficiency at any agreed point of the placement (after three weeks of experience) BSc (Hons) Podiatry Clinical Educator Handbook 2015 32 11. STUDENTS’ RESPONSIBILITIES 11.1 The student provides all the documentation for recording the outcomes of formative and summative assessment of practice. 11.2 The student stores all assessment documentation and supporting evidence in their Practice Portfolio. 11.3 The student must ensure ongoing discussion with their Clinical Educator throughout their clinical placement allocation. 11.4 The student must present the Practice Portfolio to their Stage as requested for a review of progress. 11.5 A range of people provide support for students during their practice experience and assessment of practice. It is important that if students have any questions or queries about the clinical experience, the practice portfolio or the assessment of practice, they contact the relevant person as soon as possible. 11.6 A Summary of Roles and Responsibilities is available in Appendix 19 12. MENTORING STANDARDS At present the only mentoring standards provided by the Health and Care Professions Council are incorporated within Section 5 of their Standards of Education and Training (see Appendix 20). For further guidance about areas of mentorship that should be considered when working with students please also see the Nursing and Midwifery Council Standards to support learning and assessment in practice shown in Appendix 21, as these contain more detail regarding factors that can impinge or enhance mentoring practice when taken into consideration. Plymouth University runs a Mentorship Module at both level 6 and level 7 that is available to all podiatry clinical educators working with students. This may be useful for your portfolio or can contribute credits to a further qualification. For details please ask your Link Lecturer. The Plymouth University is proud of its teaching and research and it undertakes all reasonable steps to provide educational services in the manner set out in this Handbook and in any documents referred to within it. It does not, however, guarantee the provision of such services. Should industrial action or circumstances beyond the control of the University interfere with its ability to provide educational services, the University undertakes to use all reasonable steps to minimise the resultant disruption to those services. BSc (Hons) Podiatry Clinical Educator Handbook 2015 33 BSc (Hons) Podiatry Clinical Educator Handbook 2015 34 13. APPENDICES TO CLINICAL EDUCATOR HANDBOOK 1 Glossary of Terms 37 2 Attendance Record 41 3 Sample Timesheet 43 4 Guidelines for the management of incidents that occur during undergraduate student placements 45 5 Incident Report Form 51 6 Criteria for Identifying Clinical Educators 53 7 Student Profile Document 55 8 Learning Contract 57 9 Tutorial Form (Record of Meetings) 59 10 Practice Portfolio Feedback Sheet 61 11 Reports From Others During Placement Form 63 12 Reflective Report Form 65 13 Patient Feedback Form 67 14 Learning Outcome Assessment/Sign-off Grid (Example: Communication) 69 15 Mid-Point Report Form 71 16 End of Placement Report Form 73 17 Quality Assurance Agency Benchmark Statements 75 18 Signature Record 87 19 Summary of Roles and Responsibilities 89 20 HPC Standards for Education and Training Placements 93 21 NMC Standards to support learning and assessment in practice 95 BSc (Hons) Podiatry Clinical Educator Handbook 2015 35 BSc (Hons) Podiatry Clinical Educator Handbook 2015 36 Appendix 1 Glossary Assessor A member of the multi-professional health and social care team who contributes to the assessment of practice as delegated by the Clinical Educator. Clinical Educator A professional member of the healthcare team who facilitates learning, supervises and assesses students in the practice setting. Previously termed ‘mentor’, the Clinical Educator is professionally responsible for assessing the competence of the student and signing the summative assessment of practice documentation. Faculty The BSc (Hons) Podiatry programme is based in the School of Health Professions within the Faculty of Health and Human Sciences Fail The student does not reach the required standard and is discontinued from the programme. Formative assessment The aim of formative assessment is to review the student’s progress towards successfully achieving the practice learning outcomes for the module and inform development. Strengths and weaknesses are identified and the learning contract is updated accordingly. HCPC Health and Care Professions Council HCPC SETS Health and Care Professions Council Standards of Education and Training HCPC SOPS Health and Care Professions Council Standards of Proficiency Learning contract A written agreement between two or more people that identifies individual (student) learning objectives and how they are to be achieved. Student progress is reviewed and the objectives are updated at regular intervals Learning outcome Learning outcomes are detailed in the programme specification, and identify what learners should have achieved as a result of a learning process. Mentor A term previously used for the Clinical Educator role. Module The three-year BSc (Hons) Podiatry Programme is comprised of modules. Each module accrues academic credits at Year 1, Year 2 and Year 3 that are attained through assessment and has specified learning outcomes that relate to the QAA benchmark statements and the Health and Care Professions Council BSc (Hons) Podiatry Clinical Educator Handbook 2015 37 Standards of Proficiency. Each module has a Plymouth University code and title, (e.g. POD104, Introduction to Clinical Practice) OSCE Objective structured clinical examination. PDT Placement Development Team Placement A practice area or place to which a student is allocated for a specified period of time. Portfolio A purposeful collection of examples of learning collected over a period of time that gives detailed and visible evidence of a person’s competence. The portfolio is a tool that highlights progression in competence development and is the responsibility of the person (student) involved. Adapted from Tillema and Smith (2000) Proficiency The Theterm termproficiency proficiencymeans meanstoto‘describe ‘describethe theskills skillsand andability abilitytoto practice practicesafely safelywithout withoutthe theneed needfor fordirect directsupervision’. supervision’. There Thereare arehowever howevermany manydifferent differentdefinitions definitionsand anda ageneral generallack lackofof agreement agreementabout aboutitsitsmeaning. meaning. Programme A number of modules (units) of study, the successful completion of which leads to an award. PQDD Practice Quality Development Division QAA The Quality Assurance Agency for Higher Education. The QAA has prepared a ‘Code of practice for the assurance of academic quality and standards in higher education’. Referral The student does not demonstrate proficiency/achievement of the practice learning outcomes to the required standard, normally at the first or second attempt. Three attempts at the summative assessment of a module are normally permitted before the student is failed. However students may access information concerning the University regulations at www.plymouth.ac.u,/studenthandbook “Rules and Regulations.” Reflection Reflection is a form of mental processing – like a form of thinking – which is used to fulfil a purpose or to achieve some anticipated outcome. It is largely based on the processing of knowledge, understanding and emotions that the student already possesses. Reflection should link theory and practice and lead to professional and personal development through thoughtful, innovative and critical practice. Adapted from Moon (2002). The assessment of practice method is applied objectively, Reliability BSc (Hons) Podiatry Clinical Educator Handbook 2015 38 accurately and consistently in the assessment of each student. Inter-assessor (Clinical Educator) reliability means that the result of the assessment of a student would be the same whoever assesses that student. Intra-assessor (Clinical Educator) reliability means that a Clinical Educator/assessor is consistent in their assessment of all students. SEEC Southern England Universities Consortium Summative assessment The aim of the final, summative assessment is to determine whether the student has achieved the required practice learning outcomes for the module. Term The academic year is divided into two terms of 16 weeks. The autumn term runs from September to January/ February. The summer term runs from February to June/July Timesheets Timesheets (student experience record) are used to record your time in both theory and practice and are submitted on a monthly basis to the programme administration office. Validity The assessment of practice process effectively measures what it is supposed to measure i.e. an identified practice learning outcome/ proficiency/capability. BSc (Hons) Podiatry Clinical Educator Handbook 2015 39 BSc (Hons) Podiatry Clinical Educator Handbook 2015 40 Appendix 2 Attendance Record Please can supervising clinicians sign against sessions that the student has attended so that a record is available to check against timesheets that students need signing off. Many thanks Date Am Pm Monday Tuesday Wednesday Thursday Friday Monday Tuesday Wednesday Thursday Friday Monday Tuesday Wednesday Thursday Friday BSc (Hons) Podiatry Clinical Educator Handbook 2015 41 BSc (HONS) PODIATRY TOTAL PRACTICE HOURS: STUDENT EXPERIENCE RECORD SHEET NAME: MONTH: 20____ COHORT: BASE: Week 1 Mo Tu We Th Fr Signature Week 2 Mo Tu We Th Fr Signature Week 3 Date Date Date Hours* Activity code Hours* Activity code Hours* Activity code Week 4 Mo Tu We Th Fr Signature Week 5 Mo Tu We Th Fr Signature Week 6 Mo Tu We Th Fr Signature Mo Tu We Th Fr Signature Date Date Date Hours* Activity code Activity Codes: Hours* Activity code Hours* Activity code LCC = Local Care Centre A = Absence C = Compassionate Leave* P = Placement SD = Study Day (private study) AL = Annual Leave SL FA S Hours* - Please indicate hours worked e.g. 7.5, 3.0 = Skills Lab at PAHC = Family Absence* = Sick *you must discuss this with your Personal Tutor or the Programme Lead Placement: Provide name of practice placement area Student Declaration Clinical Educator Declaration I certify that the information given above is correct I confirm that the student attended clinical placements as indicated above Signature: Signature: Date: Name: (please print) BSc (Hons) Podiatry Clinical Educator Handbook 2015 42 Student Experience Record Sheet – guideline notes for students and clinical educators The reason that the student is required to fill in a Student Experience Record sheet is so that a record of all your theory and practice hours is kept for the three year BSc (Hons) Podiatry Programme. It is essential that you complete a minimum of 1000 hours of practice before you are able to graduate. STUDENTS MUST: Complete a form for each calendar month of the year (i.e.12 per year) including vacation time. Record the date, hours and activity code(s) in the relevant boxes. If you have a day when you undertake different activities in the morning and in the afternoon, this should be recorded 6th 6th 4 3.5 T TC Sign to certify that the information on the form is correct. When you are undertaking skills lab sessions, attending LCC or on a placement your mentor(s) must also sign the form. Submit the completed and signed form to Programme Administration, PAHC Marjon, by the first day of the next month Compassionate Leave and Family Absence should be discussed with your Personal Tutor or the Programme Lead before being declared Report all absences to your placement (if applicable) and PAHC Programme Administration if you are unable to attend. Each site is manned from 08.30 – 17.00 hours on Monday to Thursday, and 08.30 - 16.30 hours on Friday. There is an answer- phone outside these times, the number for PAHC is 01752 588800 or email pahc.reception@plymouth.ac.uk NOTE THAT TRAVEL CLAIMS CANNOT BE PROCESSED WITHOUT A CORRESPONDING EXPERIENCE RECORD AND THEREFORE BOTH MUST BE SUBMITTED BY THE 1ST OF EACH MONTH Note for mentors It would be appreciated if practitioners could contact the PAHC Marjon Site if a student does not attend a practice placement as planned DISCLAIMER: All students undertaking programmes delivered by the Faculty of Health and Human Sciences are reminded that any alteration to University documentation, including practice portfolios, involving forgery/falsification of a mentors comments or signature/initialling will be investigated. This investigation could lead to disciplinary action, which may lead to a student being unable to achieve professional registration. BSc (Hons) Podiatry Clinical Educator Handbook 2015 43 Appendix 4 Guidelines for the management of incidents that occur during undergraduate student placements (South West Region NHS funded Podiatry Services) Introduction Undergraduate Podiatry Students from the Plymouth University (Plymouth University) undertake clinical placements with NHS funded Podiatry Services throughout the South West region. The Clinical Educators Handbook contains guidance on what is expected of placement providers however the following are guidelines produced in collaboration with the Plymouth University for the actions that are recommended to take place in some circumstances that may not be included. This includes what support may be required for the student and also placement providers. This doesn’t override organisational policies that are in place within Service or University protocols. 1. 2. Incident Allegation made about NHS staff by student to Plymouth University Allegation made about NHS staff by student to NHS staff Action to be taken Student statements collected or interviews conducted. Considerations NHS manager contacted. Seriousness of allegations will affect timeframes to contact placement provider Plymouth University may need to provide written evidence/attend interview with student. Seriousness of allegations will affect timeframes to contact Plymouth University. Local NHS organisational procedures to be followed if required. Local NHS organisational procedures to be followed. Plymouth University link lecturer to be informed as soon as is reasonably practicable by relevant person. Student statements collected or interviews conducted. BSc (Hons) Podiatry Clinical Educator Handbook 2015 If the link lecturer is occupied elsewhere there may be a delay in receiving notification so Programme Lead should be copied in. Students should not be asked to provide statements/be interviewed without support or advice from Plymouth University. Reflective reports are 44 labelled Private and Confidential and cannot be used for statement purposes unless informed consent is given (student should contact Plymouth University beforehand). 3. Inoculation Injury Local NHS organisational procedures to be followed. If a high risk event has occurred the Plymouth University link lecturer to be informed as soon as is reasonably practicable by Clinical Educator. Required details to be recorded in student’s portfolio (Incident Record Form) and replica information sent in email to link lecturer (so they can liaise with personal tutor if required). 4. Student fails to attend for clinic without making contact Placement provider/Clinical Educator to report absence and lack of report to Plymouth University link lecturer. Any further concerns should also be reported to the link lecturer. BSc (Hons) Podiatry Clinical Educator Handbook 2015 If the event will have repercussions for the student then Plymouth University will need to ensure the support is continued when the student returns from placement, or may need to withdraw the student from placement. If the event requires further action the Plymouth University will ensure the student is receiving suitable support and advice once notified. Where the event is low risk (trip, sterile inoculation, near miss) a record will be filed but no further action taken. Absence should simultaneously be reported to Plymouth University Programme Administration (01752 588800) by student at time of reporting to Clinical Educator. The Clinical Educator is entitled to contact the student and information from the Student Profile should enable this, however there is no obligation. 45 5. Student reports in sick 6. Student causes injury to a patient & suffers anxiety as a result & doesn’t tell anyone at the time. Absence should be noted on the attendance record and subsequently the timesheet. The reason for the lack of notification should be checked on their return and can be recorded as feedback in relation to professional behaviour if required. Clinical Educator to remind student that this should also be reported to Programme Administration and ensure that this is subsequently recorded on Attendance Record and timesheet accurately. All patients and the record of treatment should be checked by the supervising Clinical Educator before the patient leaves the clinic to ensure that all interventions are recorded and the supervisor is happy with the treatment delivered to the patient before countersigning the records. As soon as possible after the Clinical Educator recognises the student is anxious or disturbed they should take the opportunity to enquire about the cause and address it according to BSc (Hons) Podiatry Clinical Educator Handbook 2015 It should be clarified at induction what lines of communication are expected and enabled for students, and an alternative to contact if someone is sick/on leave. Local procedures are to be followed. Where a student has Swine Flu this needs to be reported to Plymouth University immediately. If there is repeated illness/circumstances affecting a student please advise Plymouth University as a review of their Fitness to Practice may be required. Records of treatment are countersigned by the supervisor to indicate that the student has acted under their direction and they hold responsibility. If a short discussion can be held, an offer to talk later can allay a student’s concerns without affecting clinic management. If a student is significantly disturbed then it may be necessary to remove 46 the level of anxiety. 7. 8. Service user raises a concern about care received by a student Student hasn’t completed mandatory training before attending placement A Patient Feedback Form can be used to record the patient’s concerns directly to the student and the Clinical Educator can assist them on reflecting on the encounter. If the concerns are considered valid the Clinical Educator could request a reflective report from the student to outline the learning from the experience and proposed future actions. Plymouth University to contact placement provider to notify them of circumstance prior to placement to discuss significance and any possible readjustments BSc (Hons) Podiatry Clinical Educator Handbook 2015 them from the room until a suitable time for further discussion. Providing company for them may be a consideration if they are very disturbed and the availability will depend on the clinic. Plymouth University should be informed by either the Clinical Educator or student – this can be the link lecturer and/or personal tutor or Programme Lead. A record of the occurrence and actions undertaken can be recorded in the tutorial section of the portfolio. If this is a consistent and valid concern then the Clinical Educator should help the student address the issue if possible. If the student is not responding to the constructive feedback assistance either from the link lecturer or Trust colleagues should be sought. If the student does not modify their behaviour/practice the Plymouth University link lecturer should be informed. The Mandatory Training Record in students’ portfolios is signed off prior to placement. If it is not signed off and the Plymouth University has not been in contact it is possible that the 47 (alternative training dates may occur shortly after commencement of placement). 9. Student expectations not met If the lack of training cannot be suitably accommodated to the satisfaction of the placement provider the student will be withdrawn from the placement. Students complete a Pre-Placement Form indicating the exchange of information prior to commencement of the placement. Expectations and provision should be an area that is discussed. Students should provide Learning Contract documents outlining their requests prior to start of placement and in response to the provision of their timetable. If placement provision is altered and the student is dissatisfied with the reason or concerned that it will affect their achievement of the module, they should discuss it with their Supervising Clinical Educator initially, and be directed to the Plymouth University BSc (Hons) Podiatry Clinical Educator Handbook 2015 paperwork is incomplete (due to a pressing timescale) although the student has attended all training – please check with Plymouth University link lecturer before taking further action. Clinical Educators should be prepared for contact by the student when they secure the information required for the PrePlacement Form and be able to discuss the timetable of the placement and any alternative experiences suitable for their level of learning. Clinical Educators can request a Learning Contract from a student. It is necessary to ensure that students’ are able to gain the experiences required to achieve the Portfolio Learning Outcomes from the outset of the module. Where modifications prevent this, they will need supporting evidence from the Placement provider to support their Extenuating 48 Link lecturer if the matter remains unresolved. 10 Compliment received from a service user about a student Circumstances procedure. Student to document this in their portfolio using the Patient Feedback Form. BSc (Hons) Podiatry Clinical Educator Handbook 2015 49 Appendix 5 Plymouth University Faculty of Health and Human Sciences BSc (Hons) Podiatry Incident Record Form Incident 1 Student name: Clinical Educator name: Incident form number: Brief summary of accident/near miss and actions undertaken: University informed (please tick) by student/Clinical Educator (please delete as applicable) Recommended Further Actions: Signed (Clinical Educator)……………………. Date……………………… Incident 2 Student name: Clinical Educator name: Incident form number: Brief summary of accident/near miss and actions undertaken: University informed (please tick) (please delete) Recommended Further Actions: by student/Clinical Educator Signed (Clinical Educator)……………………. BSc (Hons) Podiatry Clinical Educator Handbook 2015 Date……………………… 50 BSc (Hons) Podiatry Clinical Educator Handbook 2015 51 Appendix 6 Criteria for Identification of Clinical Educators All Clinical Educators should meet the following criteria before they summatively assess a student during the Years 2 and 3 of the Programme: a) Have completed a training programme or statutory approved programme in teaching and assessing in practice or its equivalent. b) Post qualifying experience of a minimum of one year. c) Be aware of the aims, content, and structure of the BSc (Hons) Podiatry Programme. This may be achieved by attendance at one of the preparation sessions organised by the Institute staff or via self-study materials. Allocation of Clinical Educators The University is responsible for ensuring that sessions are provided for Clinical Educators on the method for the assessment of practice and general information on the Programme. A record will be kept by the Placement Area of those individuals who attend any sessions of preparation. The University will provide an opportunity for Clinical Educators to have an annual up-date on the role as assessors of practice. This process will be recorded. BSc (Hons) Podiatry Clinical Educator Handbook 2015 52 BSc (Hons) Podiatry Clinical Educator Handbook 2015 53 Appendix 7 Faculty of Health and Human Sciences School of Health Professions BSc (Hons) Podiatry Student Profile Name: Gender: Date of Birth: Contact Numbers: Email address: Current level of study: Level Placement date From: To: Car available for placement (Yes/No): Accommodation required (Yes/No): Work history: Hobbies/Interests BSc (Hons) Podiatry Clinical Educator Handbook 2015 54 BSc (Hons) Podiatry Clinical Educator Handbook 2015 55 Appendix 8 LEARNING CONTRACT Name of Placement: …………………………………………………………… Date of commencement of Placement:……………………………………… Name of sign-off Clinical Educator:…….……………………………………… The following are my identified learning needs for this placement: I will liaise with my Clinical Educator and any other supervising practitioners to ensure that I do all that I can to achieve my learning objectives. I will liaise with my personal tutor if I have any concerns. I will practise safely and professionally at all times. Student signature: ……………………… Date: …………………….. I will work with the student, and will liaise with all other practitioners supervising her/his practice when I am not available, to ensure that the student’s learning needs are being met and that I am able to monitor her/his progress. I have explained the health and safety issues and emergency procedures relevant to this placement to the student. Sign-off Clinical Educator Signature: ……………………….Date:…..………… BSc (Hons) Podiatry Clinical Educator Handbook 2015 56 Student name:……………………………………………………………. Name of placement area:……………………………………………….. Date:……………………………………………………………………….. Name of Clinical Educator:…………………………………………... Learning Contract Objectives Strategies/resources Timeframe Evidence Verification/evaluation (What do I plan to learn?) (How do I plan to learn it?) (When do I plan to finish?) (How will I show I have completed the task?) (How will I demonstrate that I have learned it?) Objectives Strategies/resources Timeframe Evidence Verification/evaluation (What do I plan to learn?) (How do I plan to learn it?) (When do I plan to finish?) (How will I show I have completed the task?) (How will I demonstrate that I have learned it?) BSc (Hons) Podiatry Clinical Educator Handbook 2015 57 Objectives Strategies/resources Timeframe Evidence Verification/evaluation (What do I plan to learn?) (How do I plan to learn it?) (When do I plan to finish?) (How will I show I have completed the task?) (How will I demonstrate that I have learned it?) Objectives Strategies/resources Timeframe Evidence Verification/evaluation (What do I plan to learn?) (How do I plan to learn it?) (When do I plan to finish?) (How will I show I have completed the task?) (How will I demonstrate that I have learned it?) Objectives Strategies/resources Timeframe Evidence Verification/evaluation (What do I plan to learn?) (How do I plan to learn it?) (When do I plan to finish?) (How will I show I have completed the task?) (How will I demonstrate that I have learned it?) BSc (Hons) Podiatry Clinical Educator Handbook 2015 58 BSc (Hons) Podiatry Clinical Educator Handbook 2015 59 Appendix 9 Tutorial Form (Record of Meetings) Plymouth University Faculty of Health and Human Sciences BSc (Hons) Podiatry Tutorial Form Student name Clinical Educator name Areas for Discussion Signed (student) Dated Record of Discussion Signed (Clinical Educator) Dated Agreed Action Points Date for review……………………………………………….. Signed (student)……………………… Date…………..……. Signed (Clinical Educator)……………………………. Date………………… BSc (Hons) Podiatry Clinical Educator Handbook 2015 60 BSc (Hons) Podiatry Clinical Educator Handbook 2015 61 Appendix 10 Portfolio Feedback Form Learning Outcome Formative Feedback Form and Specific Action Points Code Clinical Educator Signature and Date Student Signature …………………………………………………………………………………………. BSc (Hons) Podiatry Clinical Educator Handbook 2015 62 Date…………………. BSc (Hons) Podiatry Clinical Educator Handbook 2015 63 Appendix 11 REPORTS FROM OTHERS DURING PLACEMENT Those podiatrists, or other health professionals, contributing to a significant part of the student’s supervision during the placement may like to record comments which will help inform the sign-off Clinical Educator of evidence of progress Others may also document comments on the student’s progress (eg, other medical/ nursing staff; student peers; service-users or their carers) Name:........................................Position:..................................Date:................. Name:.....................................Position:.....................................Date:................. Name:.......................................Position:.....................................Date:............... Name:........................................Position:..................................Date:................. BSc (Hons) Podiatry Clinical Educator Handbook 2015 64 BSc (Hons) Podiatry Clinical Educator Handbook 2015 65 Appendix 12 Private and Confidential REFLECTIVE ACCOUNT STUDENT NAME SETTING e.g. Acute care, community Date REFLECTIVE ACCOUNT Student Signature Date Assessor/Clinical Educator Signature Date BSc (Hons) Podiatry Clinical Educator Handbook 2015 66 BSc (Hons) Podiatry Clinical Educator Handbook 2015 67 Appendix 13 Plymouth University BSc (Hons) Podiatry Student name: Patient Feedback Form Please could you comment on your encounter with the student who just treated you. This will remain anonymous and your comments will help them to improve their practice. Did the student present themselves professionally? Eg Were they clean and tidy, could you understand them, were they courteous, did they ensure you understood and consented to what they were going to do before starting? Please comment: Was the treatment to your satisfaction? Eg Was the treatment as thorough as previous treatments, did they give clear advice, was the advice possible in your circumstances? Did you feel the student communicated clearly with you? Eg Did they speak clearly and use terms you understood, did you feel that they listened to what you had to say, did you feel you had their full attention when spoke with them? Was there anything you would have preferred the student to do differently? Please indicate on the line below how satisfied you were with the overall treatment from the student Very I___I___I___I___I___I___I___I___I___I___I Extremely Unhappy 0 10 happy BSc (Hons) Podiatry Clinical Educator Handbook 2015 68 BSc (Hons) Podiatry Clinical Educator Handbook 2015 69 Appendix 14 Coding POD208 LO2 C11 Placement POD208 LO2 C12 Placement POD208 LO2 C13 Placement POD208 LO2 C14 Placement Learning Outcome Sign-off Sheet COMMUNICATION Self Assessment O A S C The student is able to: demonstrate effective listening and reassessing skills to ensure that podiatric treatment is appropriate; (QAA B4) Formative Assessment Date(s) Summative Assessment Achieved/ Not achieved communicate effectively with the patient, or the patient’s relative/guardian/carer or other health care practitioner, to obtain a general physical, medical, social, and behavioural history together with a detailed history of the presenting complaint; (QAA B1) be able to select, move between and use appropriate forms of verbal and non-verbal communication with service users and others (HPC1b3 STAGE TWO SOP) Achieved/ Not achieved Demonstrate an understanding of the need to empower patients to manage their foot health and related issues and recognise the need to provide advice to the patient on selftreatment where appropriate. (HPC 1b.4 STAGE TWO SOP) Achieved/ Not achieved BSc (Hons) Podiatry Clinical Educator Handbook 2015 Achieved/ Not achieved 70 Evidence of Achievement BSc (Hons) Podiatry Clinical Educator Handbook 2015 71 Appendix 15 MID-POINT REPORT For documentation of student progress during placement Student’s self-assessment of progress to date: PUNCTUALITY APPEARANCE PROFESSIONAL BEHAVIOUR Student signature: Date:............................. .................................................... Sign-off Clinical Educator’s assessment of student’s progress to date: PUNCTUALITY APPEARANCE Sign-off Clinical Educator signature: Date:..................... PROFESSIONAL BEHAVIOUR .............................................. Personal tutor/podiatry lecturer comments: Lecturer’s signature: Date:............................. ................................................... BSc (Hons) Podiatry Clinical Educator Handbook 2015 72 BSc (Hons) Podiatry Clinical Educator Handbook 2015 73 Appendix 16 END OF PLACEMENT REPORT Please note, a report must be written at the end of a placement. Student’s self-assessment of progress during the placement: PUNCTUALITY APPEARANCE PROFESSIONAL BEHAVIOUR Student signature: ........................................................... Date:............................. Sign-off Clinical Educator’s assessment of student’s progress during the placement: PUNCTUALITY APPEARANCE PROFESSIONAL BEHAVIOUR I confirm that ……………………………………………..…. (insert student name) has behaved professionally and safely throughout this placement. Sign-off Clinical Educator signature: ........................................... Mentorship/Education qualification: …………………………….. Date: …………............................. Personal tutor’s/podiatry lecturer’s comments: Lecturer’s signature : ......................................................... Date ……………. BSc (Hons) Podiatry Clinical Educator Handbook 2015 74 BSc (Hons) Podiatry Clinical Educator Handbook 2015 75 Appendix 17 Quality Assurance Agency (QAA) Subject Benchmark Statements for Podiatry A The podiatrist working as a professional A1 Professional autonomy and accountability The award-holder should be able to: Maintain the standards and requirements for state registration in podiatry; Appreciate the role of professional and statutory bodies in podiatry; Understand the legal responsibilities and ethical considerations of professional podiatric practice; Have a detailed knowledge and understanding of the legal implications of the supply and administration of prescription only medicines available to chiropodists/podiatrists in accordance with the relevant exemption order of the 1968 Medicine Act and subsequent orders; Comply with the requirements of the Statement of Conduct of the Chiropodists Board in accordance with the 1960 Professions Supplementary to Medicine Act and any subsequent statutory regulation; Comply with statutory obligations in respect of the limitations placed on the podiatrist, e.g. in the use of local anaesthetic drugs; Demonstrate an awareness of aspects of employment law and health and safety regulations in relation to the self employed podiatric practitioner; Understand the particular considerations relating to podiatric private practice, e.g. business planning, confidentiality, informed consent, appropriate fee structures, taxation, local licensing, planning and marketing; Demonstrate an understanding of the ‘professional self’ including aspects of professionalism in manner, dress, speech, integrity and confidentiality consistent with contemporary standards and values and which recognise cultural differences; Recognise the need for lifelong learning and continuing professional development in order to maintain fitness for practice; BSc (Hons) Podiatry Clinical Educator Handbook 2015 Contributing Module(s) POD104 (LO 1-4) POD310 (LO 1-5) POD312 (LO 2) POD313 (LO 1,2) POD104 (LO 2) POD208 (LO 4) POD310 (LO 1) POD312 (LO 2) POD315 (LO 1) POD311 (LO 2) POD311 (LO 2) POD315 (LO 1) POD104 POD208 POD310 POD312 POD315 POD311 (LO 3) POD313 (LO 1) POD313 (LO 1) POD104 (LO 2) POD208 (LO 6) POD312 (LO 2) POD104 POD310 POD312 76 Demonstrate time management skills including the ability to prioritise competing demands. POD208 (LO 3) POD310 (LO 1) POD312 (LO 2) A2 Professional relationships The award-holder should be able to: Contributing Module(s): Participate effectively in multi-professional approaches to POD208 (6) Clin 3 health care appropriate to the practice of podiatry; (LO 2) POD312 (LO 3) Recognise the unique contribution that podiatric practice POD208 (6) Clin 3 can make to multi-professional care; (LO 2) POD312 (LO 3) Recognise the value of the podiatrist as a health educator; POD208 (LO 2) POD310 (LO 1) POD312 (LO 1) Demonstrate the ability to recognise the limits of one’s own POD310 (LO 1) practice, referring or discharging the patient as necessary; POD312 (LO 1+2) Understand the principles involved in working with foot care POD310 (LO 2) assistants, technical, support and administrative staff, POD312 (LO 3) delegating tasks and responsibilities where appropriate and in accordance with accepted practice; Understand that patients' rights override POD208 (LO 3) personal/commercial considerations in the practice of POD310 (LO 1) podiatry. POD312 (LO 1+2) A3 Personal and professional skills The award-holder should be able to: Exercise a professional duty of care to patients/clients/carers in the context of independent single-handed practice within the NHS, private practice and the industrial setting; Practise in an anti-discriminatory/anti-oppressive manner; Contributing Module(s): POD310( 6) POD312 (LO 1) POD208 (LO 3) POD310 (LO 1+6) POD312 (LO 1,2,3) Understand the responsibilities associated with POD312 (LO 1) independent podiatric diagnosis and the use of all of those POD310 (LO 1,3) podiatric techniques and treatments that fall within the podiatrist's scope of practice; Administer or supply pharmacological agents relevant to POD315 (LO 2) podiatric practice (to include local analgesia, anaesthetics, topical pharmacology and prescription only medicines schedules with reference to podiatrists' access to drugs); Conduct surgical interventions for foot pathologies (i.e. POD315 (LO 2) procedures performed under local anaesthesia, skin and nail surgery); BSc (Hons) Podiatry Clinical Educator Handbook 2015 77 Perform operative and psychomotor skills using a high degree of manual dexterity (e.g. scalpel reduction of skin and nail lesions); POD104 (LO 1) POD208 (LO 2) POD310 (LO 1) POD312 (LO 1+2) Conduct Non-Surgical Interventions for Foot Pathologies in the Administration of: Appropriate mechanical therapies (e.g. taping, padding POD104 (LO 1) and strapping, footwear modifications, casted POD208 (LO 2) and non-casted orthoses, chair-side orthoses); POD310 (LO 1) POD312 (LO 1+2) Appropriate physical therapies (e.g. exercise, POD208 (LO 2) manipulation, rehabilitation, principles of POD210 physio-therapeutic modalities - i.e. ultrasound, POD310 (LO 1) electrosurgery, laser therapy, infra-red, heat & cold, POD312 (LO 1+2) cryo-surgery and chemical cautery). Understand the principles of orthopaedic foot surgery; POD315 (LO 5) Recognise the need to develop and maintain current POD104 (LO 1) psychomotor skills necessary for effective patient POD208 (LO 2) assessment and management. In doing so ensure that POD310 (LO 1) skills development satisfies medico-legal requirements of POD312 (LO 1+2) podiatric practice and meets the needs of the work place setting obligation to maintain fitness for practice; Practise with an appropriate degree of self-protection and POD104 (LO 1) contribute to the well-being and safety of people in the POD208 (LO 3) work place; POD310 (LO 1) POD312 (LO 1+2) Demonstrate an understanding of the need to manage POD312 and respond effectively to the rapidly changing nature of the profession of podiatry and the context in which it is practised; Evaluate podiatric and related research and other POD314 evidence to inform and develop practice with regard to the HEAA219 function and disorders of the lower limb and foot; Continue to develop specific podiatric treatment strategies POD104 for the treatment of loco motor and foot disorders; POD208 POD310 POD312 Demonstrate a basic level of understanding of the POD313 evolving policy agenda that impacts on the delivery of health care and the practice of podiatry; Uphold the principles and practice of clinical governance. POD312 POD210 BSc (Hons) Podiatry Clinical Educator Handbook 2015 78 A4 Profession and employer context The award-holder should be able to: Contributing Module(s): Contribute to and maintain a safe health care POD104 (LO 1) environment within a range of working environments e.g. POD208 (LO 3) private practice, the national health service, patients' own POD310 (LO 1) homes, care homes; POD312 Demonstrate an understanding of the role of the podiatrist POD313 (LO 1) within public and private health care sectors; Know about current developments in health care policy POD313 (LO 2) and how these impact on podiatry; Recognise the value of research and other scholarly POD314 (LO 2) activity in relation to the development of the podiatry POD314 ( LO 3) profession and for the benefit of patient care; Practise podiatry independently, particularly in the context POD312 (LO1) of both the public and private sectors, recognising the particular demands of the commercial sector in relation to self-employment; Recognise the value of professional, organisational, POD313 (LO 1) business and financial skills needed for self-employed single-handed podiatric practitioners. B The application of practice in podiatry This section describes the principles and concepts held by the profession of podiatry that are applied to maintain or improve lower limb and foot health. B1 Identification and assessment of health and social care needs The award holder should be able to: Communicate effectively with the patient, or the patient’s relative/guardian/carer or other health care practitioner, to obtain a general physical, medical, social, and behavioural history together with a detailed history of the presenting complaint; Conduct appropriate and valid neurological, vascular, biomechanical, dermatological and podiatric examinations of the patient’s lower limb and associated structures, modifying practice according to patient need; BSc (Hons) Podiatry Clinical Educator Handbook 2015 Contributing Module(s): POD104 (LO 3) POD208 (LO 4) POD310 (LO 4) POD312 (LO 4) POD104 (LO 4) POD208 (LO 2) POD310 (LO 3) POD312 (LO 1) 79 Conduct or requisition, where appropriate, specialist clinical or laboratory tests (e.g. X-ray, blood test, microscopy and culture) in order to reach accurate conclusions relating to lower limb health status; Utilise contemporary technologies that aid in patient assessment, e.g. computerised gait analysis equipment; Recognise situations where the best interests of the patient can be more appropriately served by a different health professional or a multi-disciplinary approach to care. POD208 (LO 2) POD310 (LO 3) POD312 (LO 1) POD208 (LO 2) POD310 (LO 3) POD312 (LO 1) POD208 (6) POD310 (LO 2) POD312 (LO 3) B2 Formulation of plans and strategies for meeting health and social needs The award holder should be able to: Contributing Module(s): POD104 (LO 4) POD208 (LO 2) POD310 (LO 1,5) POD312 (LO 1) POD105 (LO 1) POD208 (6) POD310 (LO 1,2) POD312 (LO 1,3) POD208 (LO 2) POD310 (LO 1) POD312 (LO 1,2) Use a problem-solving approach to identify and integrate the findings gathered from patient history taking and physical examination, to formulate and test a diagnosis and arrive at and implement a negotiated podiatric treatment plan; Understand the need to seek a second opinion and/or consult with colleagues and/or other members of the health care team to inform the treatment plan; In negotiation with the patient/patient guardian/carer, select appropriate podiatric techniques in accordance with current best practice/research. These can be selected from mechanical debridement of skin and nails, prescription and manufacture of orthoses, administration of prescription only and non-prescription medicines, local analgesia techniques, surgical procedures for skin and nail conditions, physical therapeutic modalities, and use of chair-side devices; Demonstrate the ability to record and communicate POD104 (LO 3) accurately the outcomes of patient assessment, POD208 (LO 4) diagnosis and management plans. POD310 (LO 4) POD312 (LO 1,2,4) B3 Practice The award holder should be able to: Demonstrate the ability to utilise safely the full scope of treatment regimes available to the podiatrist in the successful management of a patient presenting with a lower limb problem; Effectively use appropriate clinical techniques in accordance with the best accepted practice; BSc (Hons) Podiatry Clinical Educator Handbook 2015 Contributing Module(s): POD208 (LO 2) POD310 (LO 1+5) POD312 (LO 1,) POD208 (LO 2) POD310 (LO 1) 80 POD312 (LO 1) Demonstrate competence in: Mechanical debridement of skin and nails; Prescription and manufacture of orthoses Administration of prescription only and non-prescription medicines, Local anaesthesia techniques; Surgical procedures for skin and nail conditions; Physical therapeutic modalities; Use of chair-side orthoses Demonstrate competency in the use of appropriate therapeutic technologies that aid patient treatment, e.g. ultrasound, electrosurgery, laser therapy, infra-red, heat and cold, cryosurgery and chemical cautery; Demonstrate a competence in the recognition and adaptation of approaches to practice to meet the needs of modifying circumstances to include specific client groups e.g. children and the older person, and taking into consideration physical, psychological, social, environmental, cultural, occupational activity and economic factors; Demonstrate the ability to identify and respond to a range of clinical incidents, threats and psycho-social crises, e.g. violent patients, alcohol, substance and drug abuse; Demonstrate the ability to act swiftly and appropriately in the best interest of the patient and in accordance with contemporary practice for the maintenance of life in a clinical emergency, such as anaphylaxis, toxic reaction, epileptic attack, faint, hypo/hyperglycaemic attack, heart attack; Provide written instructions to a patient concerning details of a podiatric treatment regime requiring patient self-treatment/advice; Obtain and record informed consent for the treatment plan; Conform to current data protection legislation; The podiatric management plan and its evaluation in order to convey precise meaning to the podiatrist and/or others who may be required to follow-up the treatment and to satisfy medico-legal requirements. BSc (Hons) Podiatry Clinical Educator Handbook 2015 POD104 (LO 1) POD208 (LO 2) POD208 (LO 2) POD315 (LO 1,2) POD315 (LO 1,2) POD208 (LO 2) POD208 (LO 2) POD208 (LO 2) POD208 (LO 2) POD310 (LO 1) POD312 (LO 1) POD104 (LO 5) POD104 (LO 5) POD315 (LO 3+4) POD208 (LO 2, 4) POD208 (LO 3) POD104 (LO 2) POD310 (LO 1) POD312 (LO 1) POD208 (LO 4) POD310 (LO 1) POD312 (LO 1,2) 81 B4 Evaluation The award holder should be able to: In the context of evidence based practice, demonstrate the ability to conduct an ongoing evaluation of the podiatric management plan against treatment milestones using recognised health outcome measures; Use information gathered in evaluating the podiatric management plan to judge its effectiveness, reviewing and revising the plan as necessary in negotiation with the patient; Demonstrate effective listening and re-assessing skills to ensure that podiatric treatment is appropriate; Recognise that clinical problem solving can be an inexact art, and in solving one problem another may arise for which further action may need to be taken; Demonstrate an ability to undertake clinical audit in a podiatric context; Use the knowledge and critical appraisal of relevant podiatric and related research and evaluation methodologies to enable and facilitate an evidence based approach; Demonstrate the ability to recognise the limits of one's own practice, referring or discharging the patient as necessary. Contributing Module(s): POD208 (LO 2) POD310 (LO 1) POD312 (LO 5) POD208 (LO 2) POD310 (LO 1,2,5) POD312 (LO 1,2,3) POD208 (LO 2,4) POD310 (LO 1,4) POD312 (LO 1,4) POD208 (LO 5) POD310 (LO 1,2,3) POD312 (LO 1,2,3) POD312 POD208 (LO 2) POD310 (LO 5) POD312 (LO 1,2) POD208 (LO 2,3,6) POD310 (LO 1,2,6) POD312 (LO 1,2,3) C Subject knowledge, understanding and associated skills that underpin the education and training of a podiatrist This section describes the subject knowledge, understanding and associated skills that are essential to underpin informed, safe and effective podiatric practice. In order to be able to carry an appropriate podiatric assessment, diagnosis and treatment plan, the award holder should be able to demonstrate: C1 Systematic knowledge and understanding of the key concepts that underpin podiatry Anatomy and human locomotion studies Human anatomy with particular reference to the foot and lower limb, that includes an overview of the gross anatomy of organ systems underpinning the later study of podiatry, podiatric biomechanics, surgery, pharmacology and medicine. He/she will have an understanding of the development of normal human bipedal stance and locomotion across the life cycle in order to develop competence in analysing gait. BSc (Hons) Podiatry Clinical Educator Handbook 2015 Contributing Module(s): POD103 (LO 1-6) HEAA138 (all) 82 Histology Detailed knowledge of the cell and its intra-cellular components, the structure and function of tissues with special reference to skin that underpins understanding of general and podiatric tissue pathology. Physiology/immunology Homeostatic mechanisms, cell physiology and biochemistry; cardiovascular, respiratory, neurological and endocrine systems plus an overview of hepatic, renal and digestive systems that provides knowledge of normal human functioning and underpinning for the study of pathology and medicine. Understanding of aspects of microbiology and immunology to underpin understanding of pathological processes as applied to the lower limb and foot. Podiatric orthopaedics and biomechanics General knowledge and understanding of the basic principles of biomechanics; causes and mechanisms of dysfunction with a specific focus on effects on the lower limb and foot; detailed study of congenital and acquired changes to normal structure and function; the effects of abnormal structure and function on stance and locomotion and the tissues of the lower limb. Contributing Module(s): HEAA318 POD105 Contributing Module(s): HEAA138 (all) POD105 (LO 2,3,4) Contributing Module(s): POD103 (LO 3,4,5,6) POD208 (LO 2) Systemic and podiatric pathology Contributing Module(s): Systemic disease and the local manifestations that POD207 (LO 1) occur in the lower limb and foot, e.g. diabetes mellitus, POD210(LO 1,2,3) the arthropathies, neurological disorders, peripheral POD209(LO 1,2) vascular disease, dermatology, oncology, blood POD311 (LO 1,2) dyscrasias; the sources and effects of acute and chronic POD316 (LO 1) trauma to the foot and lower limb; effects of systemic POD315(LO 1) and local infections on the foot. BSc (Hons) Podiatry Clinical Educator Handbook 2015 83 Podiatric therapeutic sciences Contributing Module(s): The Underpinning Theory that Relates to the Management of Podiatric Pathologies. This includes Therapeutic Indications, Contraindications and Complications that may Arise from Podiatric Intervention Using: Pharmacology (to include local analgesia, anaesthetics, POD311 (LO 3,4,5) topical pharmacology and prescription only medicines POD315 (LO 1,2) schedules with reference to podiatrists' access to drugs); Surgical interventions (this includes procedures POD315 (LO 1,2) performed under local analgesia, skin and nail surgery, principles of orthopaedic foot surgery); Operative and psychomotor skills (including scalpel POD104 (LO 1) reduction of skin and nail lesions and foot ulcer POD208 (LO 2) debridement); Mechanical therapies (to include the therapies POD208 (LO 2) underpinned by biomechanical principles such as the prescription of casted and non-casted orthoses, chairside devices and footwear modifications); Physical therapies (to include exercise, manipulation, POD208 (LO 2) rehabilitation, principles of physio-therapeutic modalities, e.g. ultrasound, electrosurgery, laser therapy, infra-red, heat and cold, cryosurgery and chemical cautery). Behavioural sciences Social and psychological factors that have an impact on patients' health and their implications for, and contribution to, patient care, recognising the psychosocial effects of loss of mobility and pain and the role of the podiatrist in their amelioration. This is in the context of improving the patient's quality of life, mobility and independence; The significance of non-compliance/concordance in relation to foot health and its effect on the patient/practitioner relationship; The human factors that impact on the patient/practitioner relationship, e.g. in special populations; The principles of non-discriminatory practice. BSc (Hons) Podiatry Clinical Educator Handbook 2015 HEAA137 POD210 (LO 5) POD209 (LO 1) POD210 (LO 5) POD209(LO 1) POD310 (LO 4) POD312 (LO !,2) POD207 (LO 5) POD210 (LO 5) POD209 (LO 1,) POD312 (LO 1) POD207 (LO 4) POD210 (LO 5) POD209(LO 1) POD310 (LO 4,6) POD312 (LO 1,2) 84 Foot health promotion/education The principles and challenges of behaviours and extrinsic factors that impinge on foot health. The principles underlying strategies employed by patients' in self-care of the feet. Contributing Module(s): POD207 (LO 1,2) POD210 (LO 4,5) POD209 (LO 3) Professional studies Contributing module(s) The Nature and Scope of the Podiatry Profession to include: Concepts of the 'professional self' including aspects of POD207 (LO 4) professionalism in manner, dress, speech, integrity and POD210 (LO 5) confidentiality consistent with contemporary standards POD209 (LO 1) and which recognise cultural differences; POD104 (LO 2) POD208 (LO 3) POD310 (6) POD312 (LO 1,2) Health service policies, the organisation and delivery of POD313 (LO 2) health care; Multi-disciplinary working; HEAA218 HEAA312(LO 3) POD208 (6) POD310 (LO 2) Codes of conduct, regulatory and legislative frameworks POD104 (LO 1,2) that apply to podiatry. C2 Skills The award holder should be able to demonstrate: Information gathering The ability to gather, evaluate and synthesise evidence and information from a wide range of sources in order to derive a credible podiatric diagnosis; The ability to use validated methods of enquiry to collect and interpret data in order to provide information that informs the podiatric evidence base Problem solving Logical and systematic thinking in the management of their individual patient and also in their management of podiatric practice; BSc (Hons) Podiatry Clinical Educator Handbook 2015 Contributing Module(s): POD207 (LO 1) POD210 (LO 4) POD209 (LO 2) POD104 (LO 4) POD208 (LO4) POD310 (LO 1+5) POD312 (LO 1,2) POD314 1+ HEAA219 Contributing module(s) POD208 (LO 1) POD310 (LO 1) POD312 (LO 1) 85 The ability to draw reasoned conclusions and sustainable judgements in the context of podiatric practice; The ability to undertake a research project that includes some original thinking utilising established methods of enquiry. Communication Effective skills in communicating information, advice, instruction and professional opinion to colleagues, patients, clients, their relatives and carers; and, when necessary, to groups of colleagues or clients; The ability to provide information to the patient in the context of obtaining informed consent; Competence in the maintenance of patient records in order to meet their medico-legal responsibilities. Numeracy The ability in understanding, manipulating, interpreting and presenting data; The ability to use number skills to enable good practice in respect of calculation of dose, interpretation of physiological, biomechanical and research data. Information technology The ability to engage with technology, particularly the effective and efficient use of information and communication technology; A working knowledge of the specialist equipment used in analysing gait, assessing vascular and neurological status; The ability to safely use a range of therapeutic equipment in podiatric management; The ability to operate technological systems that facilitate the management of podiatric practice; Information technology skills that include knowledge of the use of statistical packages and the ability to make use of word processing packages for report writing. BSc (Hons) Podiatry Clinical Educator Handbook 2015 POD208 (LO 1) POD310 (LO 1) POD312 (LO 1) POD314 1+ HEAA219 Contributing module(s) POD104 (LO 3) POD208 (LO 4) POD310 (LO 4) POD312 (LO 4) POD208 (LO 3) POD310 (LO 4) POD312 (LO 2,4) POD104 (LO 2) POD208 (LO 3) POD310 (LO 4) POD312 (LO 2,4) Contributing Module(s): POD105 (LO 1) POD105 (LO 1) POD208 (LO1) Contributing Module(s): All Modules POD104 (LO 4) POD208 (LO 1) POD105 (LO 1) POD208 (LO 2) POD208 (LO 2) POD314 (4) 86 BSc (Hons) Podiatry Clinical Educator Handbook 2015 87 Appendix 18 SIGNATURE RECORD For all whose signatures appear elsewhere in the portfolio I consent to share my Ongoing Achievement Record and electronic portfolio with my sign-off Clinical Educators, other supervising practice staff and academic staff at their request, to enable my fitness for practice to be assessed. Name of student …………………………………………………………………. Signature Date/s ……………………………… Placement Name of signatory BSc (Hons) Podiatry Clinical Educator Handbook 2015 Date……………………………. Role (i.e. sign-off Clinical Educator/ supervising podiatrist/ serviceuser) Signature Mentorship qualification (if applicable) 88 BSc (Hons) Podiatry Clinical Educator Handbook 2015 89 Appendix 19 Summary of Roles and Responsibilities on Placement Before Placement Student Student completes Student Profile and sends to Clinical Educator If student is unable to attend placement they must inform their Personal Tutor, the Placement Coordinator, Placement Clinical Educator and podplacements@plymouth.ac.uk as soon as possible Clinical Educator On receipt of profile Clinical Educator sends prepared placement timetable to student (the beginning of the first week should include an induction and can be mostly observational – students should have a majority of practical experience beyond this phase) If a Clinical Educator is unable to support student on placement they, or their Head of Department must inform the Placement Co-ordinator and podplacements@plymouth.ac.uk as soon as possible STUDENTS MUST HAVE CONTACTED THEIR TRUST BY THE 8 WEEK DEADLINE OTHERWISE THE TRUST MAY WITHDRAW PROVISION The student should then review their portfolio and highlight any learning targets to their Clinical Educator The Clinical Educator is not obliged to provide any learning requirements that are not already indicated through the learning outcomes in the relevant portfolio The student will need to liaise with the The Clinical Educator needs to have Clinical Educator to assess what supplied an Induction Pack for the travel/transport plans are necessary placement, including who to contact in and if nursing accommodation is case of illness/absence, contact names available for booking and addresses, clinic addresses, parking and public transport details, relevant Trust policies and procedures (or links to electronic resources) and any further information about the placement. This can/should be placed on ARC. The student needs to prepare plans for Where possible the Clinical Educator the assessment of learning outcomes would ideally be able to contribute to from the relevant portfolio (the mode of the student's planning prior to the assessment and learning outcomes that placement are to be demonstrated) and send to Clinical Educator in preparation for induction BSc (Hons) Podiatry Clinical Educator Handbook 2015 90 During Placement Student Clinical Educator The student is expected to behave in a professional manner throughout the placement and report to the University (01752 588800) and the Placement Contact (refer to Trust induction pack) if unable to attend a clinic or will be late If a student is not attending their placement or is behaving unprofessionally in any way the Clinical Educator should inform the Placement Co-ordinator, University Link Lecturer (and student's Personal Tutor if known) The student should familiarise themselves with the information provided for induction An induction should be held on the first day to ensure the students are familiar with Fire, Health and Safety protocols and Trust policies, and to negotiate and discuss the achievement of learning outcomes throughout the placement and other considerations for practice learning The Clinical Educator should monitor attendance and performance and feedback to student. If behaviour is not modified the Plymouth University Link Lecturer should be contacted. Ideally a minimum of 2 tutorials should be held a week to provide students with the opportunity to prepare for the week ahead and receive feedback on the previous week (ideally in written and verbal form). All negotiated 'learning agreements' should be recorded in tutorial documentation and countersigned by both student and Clinical Educator to indicate their agreement regarding the format and content of the assessment If you believe a student is not performing to the best of their ability, is not responding to feedback appropriately, is experiencing personal difficulties, is not engaging with the learning process please alert the Plymouth University Link Lecturer (and Personal Tutor if known) The student should organise themselves so that they are prepared for each day - clean uniform, travel to destination, prior reading, prepared documentation The student should be proactive in identifying learning opportunities and formulating assessments in preparation for negotiation in tutorials If a student is experiencing a personal difficulty that may be affecting their placement experience and they are concerned about disclosing it to their Clinical Educator they should contact their Personal Tutor to discuss it BSc (Hons) Podiatry Clinical Educator Handbook 2015 91 If a student is experiencing problems regarding accommodation, learning disability provision, resource provision (computer access, library access) the Clinical Educator should be notified If a student is experiencing problems regarding accommodation, learning disability provision, resource provision (computer access, library access) the Plymouth University Link Lecturer should be notified Students should seek frequent feedback on performance throughout the placement and use it constructively to inform their practice If a student is considered to be 'failing' please ensure the Plymouth University Link Lecturer has been informed as soon as possible to ensure that support can be provided for the Clinical Educator and student involved. Frequent feedback to the student will enable them to improve their performance and enhance their progress. A student may be considered to be failing where there is consistently no progression occurring. If a Clinical Educator requires further guidance supporting a student in practice e.g.. using the portfolio, assessing, providing feedback they should contact the Plymouth University Link Lecturer for advice and support If a student is concerned that a placement is not meeting their learning needs and the Clinical Educator is aware of their concerns, they should contact the Placement Co-ordinator The student should ensure their portfolio is up to date and bring it to their midpoint review with their Personal Tutor The student should ensure that the portfolio records are kept up to date throughout the placement. It is the student's responsibility to ensure that all paperwork is appropriately completed and collated at the end of the placement prior to departure The student should complete a feedback form for the Clinical Educator BSc (Hons) Podiatry Clinical Educator Handbook 2015 The Clinical Educator should ensure that a midpoint review report has been completed and the Plymouth University Link Lecturer is informed of any problems It is essential that all failed learning outcomes are supported by documentation detailing feedback from formative assessments and the summative assessment The Clinical Educator should secure any feedback that is required for placement or personal development 92 The student should ensure that all outstanding accommodation fees or library fines are paid and books are returned prior to departure If any fines or fees are due, the student is responsible for payment. The Placement Co-ordinator can assist with communication between the Trust and the student but the University is not liable After Placement Student The student will need to submit the completed portfolio in full by the published submission date Clinical Educator Where there are queries regarding a portfolio we may need to contact the Clinical Educator concerned to get clarification Students will be required to complete a placement evaluation which is then sent back to Trusts via ARC. BSc (Hons) Podiatry Clinical Educator Handbook 2015 93 Appendix 20 Standards of Education and Training (HPC 2009). Section 5: Practice Placement For Allied Health Professions 5. Practice placement standards 5.1 Practice placements must be integral to the programme. 5.2 The number, duration and range of practice placements must be appropriate to support the delivery of the programme and the achievement of the learning outcomes. 5.3 The practice placement settings must provide a safe and supportive environment. 5.4 The education provider must maintain a thorough and effective system for approving and monitoring all placements. 5.5 The placement providers must have equality and diversity policies in relation to students, together with an indication of how these will be implemented and monitored. 5.6 There must be an adequate number of appropriately qualified and experienced staff at the practice placement setting. 5.7 Practice placement educators must have relevant knowledge, skills and experience. 5.8 Practice placement educators must undertake appropriate practice placement educator training. 5.9 Practice placement educators must be appropriately registered, unless other arrangements are agreed. 5.10 There must be regular and effective collaboration between the education provider and the practice placement provider. 5.11 Students, practice placement providers and practice placement educators must be fully prepared for placement which will include information about an understanding of: the learning outcomes to be achieved; the timings and the duration of any placement experience and associated records to be maintained; expectations of professional conduct; the assessment procedures including the implications of, and any action to be taken in the case of, failure to progress; and BSc (Hons) Podiatry Clinical Educator Handbook 2015 94 communication and lines of responsibility. 5.12 Learning, teaching and supervision must encourage safe and effective practice, independent learning and professional conduct. 5.13 A range of learning and teaching methods that respect the rights and needs of service users and colleagues must be in place throughout practice placement BSc (Hons) Podiatry Clinical Educator Handbook 2015 95 Appendix 21 Standards to support learning and assessment in practice NMC (2008) 1. Establishing effective working relationships: Demonstrate an understanding of factors that influence how students integrate into a new practice setting Provide ongoing and constructive support to support transition from one learning environment to another. Have effective professional and Interprofessional working relationships to support learning for entry to the register. 2. Facilitation of learning: Use knowledge of the student’s stage of learning to select appropriate learning opportunities to meet individual needs. Facilitate the selection of appropriate learning strategies to integrate learning from practice and academic experiences. Support students in critically reflecting upon their learning experiences in order to enhance future learning. 3. Assessment and Accountability: Foster professional growth, personal development and accountability through support of students in practice. Demonstrate a breadth of understanding of assessment strategies and the ability to contribute to the total assessment process as part of the teaching team. Provide constructive feedback to students and assist them in identifying future learning needs and actions. Manage failing students so that they may enhance their performance and capabilities for safe and effective practice or be able to understand their failure and the implications of this for their future. Be accountable for confirming that students have met, or not met, the NMC competencies in practice. As a sign-off Clinical Educator confirm that students have met, or not met, the NMC standards of proficiency in practice and are capable of safe and effective practice. 4. Evaluation of Learning: Contribute to evaluation of student learning and assessment experiences - proposing aspects for change resulting from such evaluation. Participate in self and peer evaluation to facilitate personal development and contribute to the development of others. 5. Creating an environment for learning: Support students to identify both learning needs and experiences that are appropriate to their level of learning. Use a range of learning experiences, involving patients, clients, carers and the professional team, to meet defined learning needs. BSc (Hons) Podiatry Clinical Educator Handbook 2015 96 Identify aspects of the learning environment which could be enhanced negotiating with others to make appropriate changes. Act as a resource to facilitate personal and professional development of others. 6. Context of practice: Contribute to the development of an environment in which effective practice is fostered, implemented, evaluated and disseminated. Set and maintain professional boundaries that are sufficiently flexible for providing interprofessional care. Initiate and respond to practice developments to ensure safe and effective care is achieved and an effective learning environment is maintained. 7. Evidence-based practice Identify and apply research and evidence based practice to their area of practice. Contribute to strategies to increase or review the evidence base used to support practice. Support students in applying an evidence base to their own practice. 8. Leadership: Plan a series of learning experiences that will meet students defined learning needs. Be an advocate for students to support them accessing learning opportunities that meet their individual needs - involving a range of other professionals, patients, clients and carers. Prioritise work to accommodate support of students within their practice roles. Provide feedback about the effectiveness of learning and assessment in practice. BSc (Hons) Podiatry Clinical Educator Handbook 2015 97