Renal Hypertension
advertisement

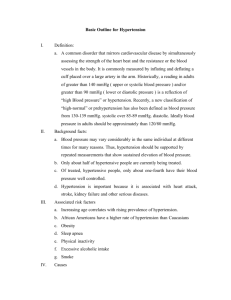
Renal Hypertension Shahram Taheri M.D. Associated Prof. IUMS INTRODUCTION • Hypertension is a frequent finding in both acute and chronic kidney disease, particularly with glomerular or vascular disorders. • The pathogenesis and preferred treatment of hypertension vary with the type of renal disease and its duration. PATHOGENESIS • The pathogenesis of hypertension varies with the type of disease (eg, glomerular versus vascular) and with the duration of disease (acute versus chronic). Acute glomerular disease • Patients with acute glomerular disease, such as poststreptococcal glomerulonephritis or membranous nephropathy, tend to be volume expanded and edematous due to sodium retention. • As a result, the elevation in blood pressure is primarily due to fluid overload, as evidenced by suppression of the renin-angiotensin-aldosterone system and enhanced release of atrial natriuretic peptide. Acute glomerular disease • Although these changes are most prominent with severe disease, the incidence of hypertension is increased even in patients with a normal serum creatinine concentration. • Both a familial predisposition to hypertension and subclinical volume expansion are thought to be important in this setting. Acute glomerular disease • Experimental studies of the nephrotic syndrome or glomerulonephritis suggest that sodium retention in these disorders is due to increased reabsorption in the collecting tubules. Acute vascular disease • Hypertension is also common in acute vascular diseases, such as vasculitis or scleroderma renal crisis. • In these settings, the elevation in blood pressure results from ischemia-induced activation of the reninangiotensin system rather than volume expansion. Acute vascular disease • This difference in mechanism between glomerular and vascular disease may be of diagnostic importance. • As an example, a patient presenting with acute kidney injury, hypertension, and red cells and red cell casts in the urine sediment almost certainly has either glomerulonephritis or vasculitis. • The absence of edema in this setting would point strongly toward a primary vascular disease. Chronic kidney disease • Hypertension is present in approximately 80 to 85 percent of patients with chronic kidney disease (CKD). The prevalence of hypertension is elevated in patients with kidney damage and a normal glomerular filtration rate, and increases further as the glomerular filtration rate falls. Chronic kidney disease • Data from the Modification of Diet in Renal Disease Study, for example, showed that the prevalence of hypertension rose progressively from 65 to 95 percent as the glomerular filtration rate fell from 85 to 15 mL/min per 1.73 m2. • As in patients without renal disease, the prevalence of hypertension is also higher in patients with higher body weight and in blacks. Stage GFR* Description Treatment stage 1 90+ Normal kidney function but urine findings Observation, control of blood or structural abnormalities or genetic trait pressure. More on point to kidney disease management of Stages 1 and 2 CKD. 2 60-89 Mildly reduced kidney function, and other Observation, control of blood findings (as for stage 1) point to kidney pressure and risk factors. disease More on management of Stages 1 and 2 CKD. 3A 3B 45-59 30-44 Moderately reduced kidney function Observation, control of blood pressure and risk factors. More on management of Stage 3 CKD. 4 15-29 Severely reduced kidney function Planning for endstage renal failure. More on management of Stages 4 and 5 CKD. 5 <15 or on Very severe, or endstage kidney failure (sometimes call established renal dialysis failure) Treatment choices. More on management of Stages 4 and 5 CKD. • There is a strong association between CKD and an elevated blood pressure whereby each can cause or aggravate the other. • BP control is fundamental to the care of patients with CKD and is relevant at all stages of CKD regardless of the underlying cause. • Hypertension is present in approximately 80 to 85 percent of patients with CKD. • The prevalence of hypertension is elevated in patients with kidney damage and a normal glomerular filtration rate, and increases further as the glomerular filtration rate falls. • Data from the Modification of Diet in Renal Disease Study, for example, showed that the prevalence of hypertension rose progressively from 65 to 95 percent as the glomerular filtration rate fell from 85 to 15 mL/min per 1.73 m2. • As in patients without renal disease, the prevalence of hypertension is also higher in patients with higher body weight and in blacks. • A variety of factors can contribute to the increased prevalence of hypertension in patients with CKD: – Sodium retention is generally of primary importance, even though the degree of extracellular volume expansion may be insufficient to induce edema. – Increased activity of the renin-angiotensin system is often responsible for at least part of the hypertension that persists after the restoration of normovolemia, particularly in patients with vascular disease since renal ischemia is a potent stimulus of renin secretion. – Regional ischemia induced by scarring may also play a role. – Hypertension can be a causative (eg, hypertensive nephrosclerosis) or contributory factor in the development of kidney disease. – Enhanced activity of the sympathetic nervous system. The afferent signal may arise in part within the failing kidneys, since it is not seen in patients who have undergone bilateral nephrectomy. – Secondary hyperparathyroidism raises the intracellular calcium concentration, which can lead to vasoconstriction and hypertension. – Lowering parathyroid hormone secretion by the chronic administration of an active vitamin D analog can reduce both intracellular calcium and the systemic blood pressure. – Treatment with erythropoietin, an effect that is in part related to the degree of elevation in the hematocrit. – Impaired nitric oxide synthesis and endothelium-mediated vasodilatation has been demonstrated in patients with uremia. Although the mechanisms are unclear, potential explanations include reduced nitric oxide availability due to a state of increased oxidative stress, or cofactor deficiencyinduced uncoupling of nitric oxide synthase. TREATMENT OF HYPERTENSION IN ACUTE GLOMERULAR OR VASCULAR DISEASE • Initial therapy with diuretics (particularly loop diuretics in patients with reduced glomerular filtration rates) to treat hypertension in patients with acute glomerular disease and edema, since diuretics will also treat the hypervolemia and associated edema. • If the hypertension persists, angiotensin converting enzyme (ACE) inhibitors may be effective, even in the low renin hypertension often associated with acute glomerulonephritis. • This response may reflect activation of tissue reninangiotensin systems, such as that in the kidney, vascular endothelium, and adrenal gland. • ACE inhibitors as initial antihypertensive therapy in patients with acute vascular diseases, since renal ischemia leads to activation of the renin-angiotensin system. • Strong data support this approach in patients with scleroderma renal crisis and prefer angiotensin inhibition in polyarteritis nodosa and other vasculitides as well. TREATMENT OF HYPERTENSION IN CKD • Treatment of even mild hypertension is important in patients with CKD to protect against both progressive renal function loss and cardiovascular disease, the incidence of which is increased with mild to moderate CKD. Goal blood pressure • In patients with proteinuric CKD, usually defined as greater than or equal to 500 mg/day or higher, the blood pressure should be lowered to less than 130/80 mmHg. • In patients with nonproteinuric CKD, defined as less than 500 mg/day, the blood pressure should be lowered to less than 140/90 mmHg. LIFESTYLE MODIFICATION • The impact of lifestyle-related factors on BP and the risk of cardiovascular and other diseases have been well documented. • Encourage lifestyle modification in patients with CKD to lower BP and improve long-term cardiovascular and other outcomes: • We recommend achieving or maintaining a healthy weight (BMI 20 to 25). Salt Restriction • A relationship between average daily salt intake and BP levels has long been recognized, leading to calls from the World Health Organization (WHO) for salt intake to be restricted to improve BP levels (http://www.who.int/cardiovascular_diseases/guidelines/ Full%20text.pdf) • We recommend lowering salt intake to o90mmol (<2 g) per day of sodium (corresponding to 5 g of sodium chloride), unless contraindicated. Physical Exercise • Increased physical exercise has been linked to a broad range of positive health outcomes through a wide variety of mechanisms. • A clear inverse relationship between exercise and average daily BP has been demonstrated by a large volume of previous epidemiological data in the general population, although exercise may lead to modest and acute physiological increases in BP during the time of the activity. Physical Exercise • We recommend undertaking an exercise program compatible with cardiovascular health and tolerance, aiming for at least 30 minutes 5 times per week. Choice of antihypertensive therapy • Attainment of goal blood pressure in patients with CKD typically requires multidrug therapy. • The choice of agent depends in part upon whether or not the patients have proteinuria. First-line therapy in proteinuric CKD • Strong evidence favors the use of an ACE inhibitor or angiotensin II receptor blocker (ARB) as first-line therapy in patients with proteinuric CKD (protein excretion greater than 500 mg/day) because, in addition to lowering the blood pressure, these drugs slow the rate of progression of CKD. • Common side effects of angiotensin inhibition must be considered including the acute reduction in glomerular filtration rate and hyperkalemia that are more likely to occur in patients with CKD. First-line therapy in proteinuric CKD • ACE-Is and ARBs should be used with caution or even avoided in certain CKD subgroups, particularly in patients with bilateral renal-artery stenosis or with intravascular fluid depletion, because of the risk of a large reduction in GFR. • The normal capacity of the kidney to auto-regulate GFR in the face of fluctuations in BP is impaired in CKD and further compromised by the use of ACE-Is or ARBs. Second- and third-line therapy in proteinuric CKD • In patients with CKD who have proteinuria and edema, initial therapy usually consists of both an angiotensin inhibitor for renal protection and a loop diuretic for edema, which, by increasing renin release, may also enhance the antihypertensive effect of the angiotensin inhibitor. • The use of a diuretic may also restore the antiproteinuric effect of ACE inhibitor therapy in patients without an adequate antiproteinuric response, since volume expansion reduces angiotensin II release and makes the blood pressure less dependent upon angiotensin II. • If further antihypertensive therapy is required, we suggest a non-dihydropyridine calcium channel blocker (eg, diltiazem or verapamil) since these drugs also lower proteinuria. • In contrast, dihydropyridines (eg, amlodipine) have little or no effect on protein excretion. • In patients with CKD who have proteinuria but not edema, we suggest either a diuretic or a nondihydropyridine calcium channel blocker as secondline and then third-line therapy. • Volume expansion, even in the absence of edema, often plays a major role in hypertension associated with CKD. Antihypertensive therapy in nonproteinuric CKD • In patients with edema, initial therapy with a loop diuretic. Once the edema is controlled, an angiotensin inhibitor or a calcium channel blocker can be added in either order if hypertension persists. Antihypertensive therapy in nonproteinuric CKD • In patients without edema, start with an angiotensin inhibitor, and then add a calcium channel blocker as second-line therapy. • If needed, we suggest adding a diuretic as third-line therapy. Fourth-line therapy with other agents • Other antihypertensive drugs can be used as necessary in patients with CKD who have resistant hypertension. • An aldosterone antagonist (spironolactone and eplerenone) is an effective fourthline agent for the treatment of resistant hypertension in general and in patients with CKD. • In addition to reducing blood pressure, aldosterone antagonists also have antiproteinuric properties that may be associated with a slower decline in renal function. • However, trials with patient-important outcomes are not available. • The efficacy of aldosterone antagonists was evaluated in a study of 46 patients with a mean estimated glomerular filtration rate (eGFR) of 57 mL/min per 1.73 m2 and hypertension that was not controlled with three mechanistically complementary drugs, including a diuretic and angiotensin inhibitor. • The mean fall in systolic pressure induced by aldosterone antagonists was 14.7 mmHg. • The main adverse effects of aldosterone antagonists in patients with CKD are a reduction in kidney function and hyperkalemia. • In the above study, 39 percent had a decline in estimated glomerular filtration rate (eGFR) of 30 percent or more when goal blood pressure was achieved and 17 percent developed hyperkalemia occurred in 17 percent. • Risk factors for hyperkalemia included a baseline eGFR ≤45 mL/min in patients with a serum potassium above 4.5 meq/L, and a fall in eGFR of more than 30 percent after therapy. Evaluation Testing for renovascular hypertension -Renovascular hypertension is the most common correctable cause of secondary hypertension. -Severe or refractory hypertension -Including retinal hemorrhages or papilledema - Bilateral renovascular disease may be present in those patients who also have a plasma creatinine above 1.5 mg/dL (132 µmol/L) Renovascular hypertension • Renovascular hypertension is likely the most common correctable cause of secondary hypertension. The incidence of this condition varies with the clinical setting. It probably occurs in less than 1 percent of patients with mild hypertension. In comparison, between 10 and 45 percent of white patients with severe or malignant hypertension have renal artery stenosis Renovascular hypertension • Workup for renovascular hypertension: Additional testing for renovascular disease is indicated only in patients in whom the history is suggestive and in whom a corrective procedure will be performed if significant renal artery stenosis is detected. Renovascular hypertension • The conditions to suspect to renovascular or secondary hypertension: Severe or refractory hypertension, including retinal hemorrhages or papilledema a plasma creatinine above 1.5 mg/dL (132 µmol/L). An acute rise in blood pressure over a previously stable baseline Suspicious to Renovascular hypertension Proven age of onset before puberty or above age 50. An acute elevation in the plasma creatinine concentration that is either unexplained or occurs after the institution of therapy with an angiotensin converting enzyme inhibitor or angiotensin II receptor blocker (in the absence of an excessive reduction in blood pressure). Suspicious to Renovascular hypertension Moderate to severe hypertension in a patient with diffuse atherosclerosis or an incidentally discovered asymmetry in renal disease. A unilateral small kidney ( 9 cm) has a 75 percent correlation with the presence of large vessel occlusive disease. Suspicious to Renovascular hypertension A systolic-diastolic abdominal bruit that lateralizes to one side. This finding has a sensitivity of approximately 40 percent (and is therefore absent in many patients) but has a specificity as high as 99 percent. Systolic bruits alone are more sensitive but less specific. The patient should be supine, moderate pressure should be placed on the diaphragm of the stethoscope, and auscultation should be performed in the epigastrium and all four abdominal quadrants. Suspicious to Renovascular hypertension Negative family history for hypertension. Moderate to severe hypertension in patients with recurrent episodes of acute (flash) pulmonary edema or otherwise unexplained congestive heart failure. Renovascular hypertension • An intraarterial digital subtraction angiogram has usually been the initial test when the history is highly suggestive; however, spiral CT scanning or 3D time-of-flight MR angiography provide a minimally invasive and, in most cases, equally accurate alternative to angiography. • In addition, Doppler ultrasonography may help predict the outcome of renovascularization procedures.