Ethical Issues in Interacting with Families about Death by Neurologic
Ethical Issues in Interacting with
Families about Death by
Neurologic Criteria?
Neil Wenger MD, MPH
UCLA Health Ethics Center
January 18, 2015
Case
• A man in his 50s battled a life-threatening illness and credited his rabbi ’s intensive assistance with helping him to do better than the physicians expected. The patient viewed his treatment as a combination of the surgery, radiation and chemotherapy provided by his physicians and a dedicated religious effort undertaken with his rabbi.
• In the midst of this illness, he presented to the hospital with a large stroke that required mechanical ventilation and agents to sustain blood pressure.
• Despite maximal therapy, he developed complete loss of all brain function proven by several clinical tests as well as a blood flow analysis.
• The man was declared dead by neurologic criteria.
Case
(cont.)
• The man’s wife requested that the ventilator and blood pressure agents be continued until their children could come to see their father later that evening.
• When the children, ages 5 and 9, arrived six hours later, she led them to the bedside and told them that their father was doing fine. They should go home to sleep.
They could return to see their father, who would be better, in the morning.
Case
(cont.)
• The patient’s wife and family then related to the physicians that the rabbi had instructed that all lifesustaining treatments should be maintained and any additional needed treatments be added to keep the patient “alive” for another 15 hours.
• According to his emissaries, the rabbi was aware that the doctors had declared the patient dead, but he rejected that contention.
• The family insisted that treatment continue anticipating the effect of the rabbi ’s prayer. Life-sustaining treatment could be withdrawn at noon the following day. The family insisted that the patient would want this.
Case
(cont.)
• At noon the next day, family and rabbinic representatives gathered at the bedside to watch as the ventilator was withdrawn.
Declaration of Death by
Neurological Criteria is Unusual
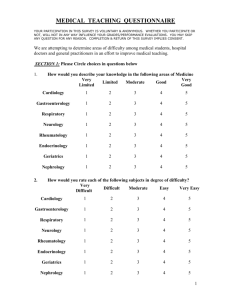
• 1-2% of all in-hospital deaths
• 10,000 – 15,000 per year
• Canadian study:
– 1% of deaths in hospitals w/o trauma centers
– 4.5% of death in hospitals w trauma centers
• Small hospital: 1-5/year
• Large academic hospital: ~25/year
-Cloutier R, Baran D, Morin JE, et al. Brain death diagnoses and evaluation of the number of potential organ donors in Quebec hospitals. Can J Anaesth.
2006;53:716-21.
Death by Neuro Criteria Declining
Proportion of patients in Calgary ICUs with traumatic brain injury, subarachnoid hemorrhage, intracerebral hemorrhage or anoxic brain injury who progressed to neurologic death, 2002-2012.
-Kramer AH, Zygun DA, Doig CJ, Zuege DJ. Incidence of neurologic death among patients with brain injury. CMAJ. 2013. DOI:10.1503 /cmaj.13027
Complicated Process to Declare
Death by Neurologic Criteria
…after Dorothy and her house fell on the Wicked Witch of the East…
Mayor: As mayor of the Munchkin City, In the county of the Land of Oz,
I welcome you most regally.
Barrister: But we ’ ve got to verify it legally. To see...
If she... Is morally, ethic ’ ly
City Father 1: Spiritually, physically
City Father 2: Positively, absolutely
All City Fathers: Undeniably and reliably DEAD!
Coroner (with death certificate): As Coroner, I must aver, I thoroughly examined her, And she ’ s not only MERELY dead, She ’ s really, most
SINCERELY dead.
Mayor: The Wicked Old Witch ... is dead!
-Shaner DM, Orr RD, Drought T, Miller RB, Siegel M. Really, most SINCERELY dead: Policy and procedure in the diagnosis of death by neurologic criteria.
Neurology. 2004;62:1683-6.
Checklist for Determination of Death by
Neurological Criteria
• Prerequisites
– Coma, irreversible and cause known
– Neuroimaging explains coma
– No CNS depressant or paralytic drug effect
– No severe acid-base or endocrine abnormality
– Temperature normal (> 36 ° C), Blood pressure ≥ 100, RR = 0
• Examination
– Pupils nonreactive
– Reflexes absent:
Corneal, Oculocephalic, Oculovestibular, Gag, Cough
– No facial or limb movement to noxious stimuli
• spinal reflexes permissible
-American Academy of Neurology. Evidence-based guideline update: determining brain death in adults. Neurology. 2010;74:1911-8.
Checklist for Determination of Death by
Neurological Criteria
• Apnea testing
• Ancillary testing: only 1 needed. To be ordered only if clinical examination cannot be fully performed due to patient factors, or if apnea testing inconclusive or aborted.
– Cerebral angiogram
– HMPAO SPECT
– EEG
– Transcranial doppler
-American Academy of Neurology. Evidence-based guideline update: determining brain death in adults. Neurology. 2010;74:1911-8.
Hospital Policy Variation in Testing for
Death by Neurological Criteria
Compliance with
American
Academy of
Neurology guidelines for preclinical testing for death by neurological criteria (%).
-Greer D, Varelas P, Haque S, Wijdicks E. Variability of brain death determination guidelines in leading US neurologic institutions. Neurology. 2008;70:284-9.
Hospital Policy Variation in Testing for
Death by Neurological Criteria
Compliance with
American
Academy of
Neurology guidelines for clinical testing for death by neurological criteria (%).
-Greer D, Varelas P, Haque S, Wijdicks E. Variability of brain death determination guidelines in leading US neurologic institutions. Neurology. 2008;70:284-9.
Hospital Policy Variation in Testing for
Death by Neurological Criteria
Compliance with
American
Academy of
Neurology guidelines for apnea testing for death by neurological criteria (%).
-Greer D, Varelas P, Haque S, Wijdicks E. Variability of brain death determination guidelines in leading US neurologic institutions. Neurology. 2008;70:284-9.
WHAT, EXACTLY, IS BRAIN DEATH?
• What is the difference between someone in a coma, who may or may not improve, and someone who is truly brain dead and may be a candidate to donate their organs? Brain death is the irreversible cessation of all functions of the entire brain, including the all-important brain stem that houses the RAS and the mechanism that controls our breathing. Dead is dead. Brain death isn't a different type of death, and patients who meet the criteria of brain death are legally dead.
-Richard Senelick. Nobody Declared Brain Dead Ever Wakes Up Feeling Pretty
Good. The Atlantic. Feb 27 2012.
WHAT, EXACTLY, IS BRAIN DEATH?
• It can be difficult to predict a person's outcome after a severe brain injury, but it can be said with certainty that a brain dead individual is dead.
-Richard Senelick. Nobody Declared Brain Dead Ever Wakes Up Feeling Pretty
Good. The Atlantic. Feb 27 2012.
Getting back to Dorothy and the
Wicked Witch of the East….
This scene illustrates that the process of declaring death is no mere footnote, but must be legal, moral, dignified, spiritual, certain, transparent, ceremonial, and sincere.
-Shaner DM, Orr RD, Drought T, Miller RB, Siegel M. Really, most
SINCERELY dead: Policy and procedure in the diagnosis of death by neurologic criteria. Neurology. 2004;62:1683-6.
Choreography of a Diagnosis of
Death by Neurological Criteria
Recognize possible death by neuro criteria
Prepare family
Perform diagnostic testing
Declare death
Discuss possible organ donation
Reasonably accommodate
Withdraw machines
Preparing the Family
• Breaking bad news
– S – SETTING up the discussion
– P – Assessing the family ’ s PERCEPTION
– I – Obtaining family ’ s INVITATION
– K – Providing KNOWLEDGE in small chunks
– E – Empathetically addressing EMOTIONS
– S – STRATEGY and SUMMARY
• Educating about death by neurological criteria
Educational Materials
Case 2
• In February 2014, an 18yo M with a gunshot wound to the head was transported to the Neuro ICU.
• Despite emergency surgery, neurologic status deteriorated and the physicians suspected that the patient – on a ventilator and receiving pressors – had died.
• Family refused the apnea test to diagnose death.
Evaluation of death by neurological criteria not optional
• Impossible to appropriately treat a patient unless clinician knows whether patient is alive.
– Dead patients do not benefit from treatment
• If patient is not to be transferred elsewhere to receive treatment, then brain death evaluation must be performed.
• Thus, consent is not needed
– But best practice is to inform family
Disclosing Death
• Directness, clarity, and veracity enhance communication.
• Avoidance of euphemisms and jargon
• A family needs to hear that their loved one has died.
• Disentangle from organ donation
– Linkage by family, not clinician
Adapted from: Shaner DM, Orr RD, Drought T, Miller RB, Siegel M.
Really, most SINCERELY dead: Policy and procedure in the diagnosis of death by neurologic criteria. Neurology. 2004;62:1683-6.
Spirituality and Ceremony
Study of Family Requests for Extended
Mechanical Support after DDNC
• 13 ethics consults at the Cleveland Clinic for family requests of continuation of physiologic support after death by neurologic criteria
• Evaluation of patient characteristics, reason for request, time of accommodation and outcome
-Flamm AL, Smith ML, Mayer PA. Family members' requests to extend physiologic support after declaration of brain death: a case series analysis and proposed guidelines for clinical management. J Clin Ethics. 2014;25:222-37.
Ethics Consults for Accommodation
Age
47
47
31
64
65
87
26 F
31
73
Sex
F
M
F
M
M
M
54 F
45 F
F
F
Dx
Suicide
MOSF
Stroke
Stroke
Tumor
Stroke
Stroke
MOSF
Request
Family gather
Hrs Outcome
18 Heart stopped
Family gather <6 Withdrawal p arrival
Decide re: donation 29 Withdrawal unilateral
Disbelieve DDNC 45 “ usual procedures ”
Disbelieve dx
Family gather
Disbelieve DDNC
Family gather
Found down Disbelieve DDNC
C-sect emb Anger
14 F Post op Isc Disbelieve DDNC
Cardiac
17 M TBI
Son disbelieved DDNC
Awaiting miracle
<4
6-8
<10
5
Eventual agreement
Withdrawal p arrival
Heart stopped
Withdrawal p arrival
>75* Transferred
72 Eventual agreement
125* Transferred
3 Withdrawal
22 Eventual agreement
* DNC not performed
Absurd Proposition
Permit use of “ life support machines ” in death to “ reasonably accommodate ” but refuse to permit use of life support to maintain patients in permanent vegetative state.
Types of Requests for Accommodation
• Finite-goal accommodations – usually emotionally driven and practically achievable (<24 hours)
– Family arrival
– Emotional closure
• Indefinite accommodations – usually beliefs, trust and anger (often >24 hours)
– Not accepting death
Balancing “ Reasonable Accommodation ”
• Respect patient ’ s beliefs
• Reduce family grief
• Address emotional needs
• Professional standards
• Moral distress
• Respect for dead
• Care and resource needs of other patients
Case 3
• 82yo F sustained a massive stroke not amenable to treatment. Over 2 days she progressed to DDNC.
• Family asked that ventilator be maintained until family arrives from Asia in 1 week.
• Medical team explained that this would be attempted. Patient had Medicare so charges would accrue to the family starting the next day.
Approach to Accommodation
• Address accommodation at the outset
– Discuss what is “ reasonable ” and set limits
– Clearly disclose hospital policy
• Intensive support of family
• Include all medical team members in plan
• No ethical justification for continued physiologic support of dead person without finite goal
Choreography of a Diagnosis of Death by Neurological Criteria
Recognize possible death by neurological criteria
Prepare family
• Empathic breaking of bad news
• Foreshadowing
• Written materials
Perform diagnostic testing
Declare death
Discuss possible organ donation
Withdraw machines
• Rigorous testing per guidelines must be performed
• Forthright disclosure
• Anticipate accommodation
• Separate organ donation from death declaration
• Set plan for withdrawal
Reprise of Case 1
• Little doubt that the patient would have wanted treatments maintained and escalated to permit the chance for a miracle
• Finite request of < 24 hours
• However continuing physiologic support:
• Served no medical purpose
• Harmed the children
• Compromised professional standards
• Grievously disturbed nursing staff
• Led to a crisis of faith when the man did not breath when extubated at noon.