Care Select - indianamedicaid.com
advertisement

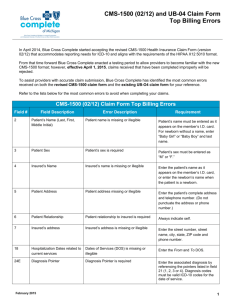
CMS-1500 Billing Presented by EDS Provider Field Consultants October 2009 Agenda • Objectives • CMS-1500 • Claim Form Billing Guidelines - Various Specialties • Crossover Claims • Consent Form, Sterilization and Partial Sterilization • Incontinence, Ostomy, and Colostomy Supplies • Program Guidelines • Prior Authorization • Code Sets • Fee Schedule • Common Denials • Helpful Tools • Questions CMS-1500 Billing 2 / October 2009 Objectives • Following this session, providers will be able to: –Identify their provider classification –Bill claims correctly for various specialties –Submit crossover claims successfully –Understand the sterilization consent completion –Know the program exclusions –Have more information about prior authorization –Identify the various provider code sets –Find and understand how the fee schedule can assist providers –Know the common denial causes and resolutions CMS-1500 Billing 3 / October 2009 CMS-1500 Claim Form DRAFT 17a: Enter qualifier ZZ and referring provider taxonomy number (if applicable) or qualifier 1D and referring provider or PMP (atypical providers) LPI. 24I and J: Qualifier ZZ and rendering provider taxonomy or 1D and rendering provider LPI for atypical providers. 17b: NPI of the referring provider. 24J: Rendering provider NPI 33: Billing provider service location – must include ZIP Code + 4. 33a: NPI for billing provider and 33b: Qualifier ZZ and billing provider taxonomy or qualifier 1D and billing provider LPI. CMS-1500 Billing 4 / October 2009 Billing Guidelines Provider Classifications • Billing Provider – Provider classification assigned to a billing entity or solo practitioner at a service location • Group Provider – The classification given to a corporation or other business structure that has rendering providers linked that are the performers of the services provided • Rendering Provider – A provider that performs the services for a group or clinic and is linked to the group or clinic • Dual – A billing provider performing services as a sole proprietor at an assigned service location and is also a rendering provider working for a group CMS-1500 Billing 5 / October 2009 Billing Guidelines Anesthesia Effective October 16, 2003, and after: • Use Current Procedural Terminology (CPT®) codes 00100-01999 (refer to IHCP Provider Manual for more information) • Bill the actual time in minutes and include it in field 24G • One unit = 15 minutes • Additional units are allowed based on a patient’s age when billing for emergency services (bill using procedure code 99140) CMS-1500 Billing 6 / October 2009 Billing Guidelines Anesthesia • Providers bill postoperative pain management using code 01996 • The IHCP does not separately reimburse this code on the same day the epidural is placed – However, it is reimbursed for subsequent days when an epidural is managed CMS-1500 Billing 7 / October 2009 Billing Guidelines Chiropractic Services • Package A services are limited to 50 chiropractic services per member, per calendar year – The IHCP reimburses for no more than five office visits within the 50 visits • Package B reimbursement is available for medically necessary pregnancyrelated services. The following are appropriate chiropractic diagnosis codes for package B members: – 646.93, 648.73, 648.93 • Package C members are allowed five office visits and 14 therapeutic physical medicine treatments per member, per calendar year CMS-1500 Billing 8 / October 2009 Billing Guidelines Chiropractic Services • The following are covered codes for office visits: –99201, 99202, 99203, 99211, 99212, 99213 • The following are covered codes for manipulative treatment: –98940-98943 CMS-1500 Billing 9 / October 2009 Billing Guidelines Injections • The IHCP reimburses for physician office injectable drugs using Healthcare Common Procedure Coding System (HCPCS) J codes and CPT immunization codes • Pricing includes the current average wholesale price plus a $2.90 administration fee • The IHCP reviews pricing for a physician office administered drug each quarter • To price appropriately, HCPCS code J3490 must be submitted with the appropriate NDC, name, strength, and quantity CMS-1500 Billing 10 / October 2009 Billing Guidelines Injections and NDC Codes • The IHCP Provider Manual contains lists of J codes that require a National Drug Code (NDC) –Chapter 8, Section 4 • For paper CMS-1500 claims forms, report NDC information in the shaded area of field 24 of the CMS-1500 claim form • The NDC is not used for provider reimbursement CMS-1500 Billing 11 / October 2009 Billing Guidelines Mental Health RBMC • Effective January 1, 2007, outpatient mental health services are carved-in to the risk-based managed care (RBMC) delivery system • Services provided to RBMC members by the following specialty types are the responsibility of the managed care organizations (MCOs), effective January 1, 2007: – Freestanding Psychiatric Hospital – Outpatient Mental Health Clinic – Community Mental Health Center – Psychologist – Certified Psychologist – HSPP – Certified Clinical Social Worker – Psychiatric Nurse – Psychiatrist CMS-1500 Billing 12 / October 2009 Billing Guidelines Mental Health RBMC • Services that are the MCO’s responsibility: –Office visits with a mental health diagnosis –Services ordered by a provider enrolled in a mental health specialty, but provided by a non-mental health specialty (such as a laboratory and radiology) –Mental health services provided in an acute care hospital –Inpatient stays in an acute care hospital or freestanding psychiatric facility for treatment of substance abuse or chemical dependency CMS-1500 Billing 13 / October 2009 Billing Guidelines Mental Health RBMC • MCOs –Anthem www.anthem.com –Managed Health Services (MHS) www.managedhealthservices.com –MDwise www.mdwise.org • Behavioral Health Organizations (BHOs) –Magellan (Anthem) www.magellanhealth.com –Cenpatico (MHS) www.cenpatico.com –MDwise www.mdwise.org CMS-1500 Billing 14 / October 2009 Billing Guidelines Surgical Services Cosurgeons: • Cosurgeons must append modifier 62 to the surgical services • Modifier 62 cuts the reimbursement rate to 62.5 percent of the rate on file Bilateral Procedures: • To indicate a bilateral procedure, providers bill with one unit in field 24G, using modifier 50 • Use of this modifier ensures that the procedure is priced at 150 percent of the billed charges or the rate on file Note: If the CPT code specifies the procedure as bilateral, then the provider must not use modifier 50 CMS-1500 Billing 15 / October 2009 Billing Guidelines Surgical Services • Postoperative care for a surgical procedure includes 90 days following a major procedure surgical procedure and 10 days following a minor surgical procedure • Separate reimbursement is available for care during the global postoperative period for: - Services unrelated to the surgical procedure - Care not considered routine - Postoperative care for surgical complications CMS-1500 Billing 16 / October 2009 Billing Guidelines • Submit claims on Web interChange, including the following: – Surgery payable at reduced amount when related postoperative care paid – Postoperative care within 90 days of surgery – Preoperative care on day of surgery – Surgery payable at reduced amount when preoperative care paid same date of service • In the claim note, the IHCP accepts the following: – Information that documents the medical reason and unusual circumstances for the separate evaluation and management (E/M) visit – Information supporting that the medical visit occurred because of a complication, such as cardiovascular complications, comatose conditions, elevated temperature for two or more consecutive days, medical complications due to anesthesia other than nausea and vomiting, postoperative wound infection requiring specialized treatment, or renal failure CMS-1500 Billing 17 / October 2009 Billing Guidelines Multiple Surgery Procedures • When two or more covered surgeries are performed during the same operative session, multiple surgery reductions apply to the procedure based on the following adjustments: – 100 percent of the global fee for the most expensive procedure – 50 percent of the global fee for the second most expensive procedure – 25 percent of the global fee for the remaining procedures • All surgeries performed on the same day, by the same rendering physician, must be billed on the same claim form; otherwise, the claim may be denied and the original claim may be adjusted CMS-1500 Billing 18 / October 2009 Billing Guidelines Therapy Services • Per 405 IAC 5-22-6, prior review and authorization by the office is required for all therapy services with the following exceptions: – Initial evaluations – Emergency respiratory therapy – Any combination of therapy ordered in writing prior to a member’s release or discharge from inpatient care, which may continue for a period not to exceed 30 units, sessions, or visits in 30 calendar days – Deductible and copayment for services covered by Medicare Part B – Oxygen equipment and supplies necessary for the delivery of oxygen with the exception of concentrators – Therapy services provided by a nursing facility or large private ICF/MR, included in the facility’s per diem – Physical therapy, occupational therapy, and respiratory therapy ordered in writing by a physician to treat an acute medical condition, except as required in Sections 8, 10, and 11 of this rule CMS-1500 Billing 19 / October 2009 Billing Guidelines Therapy Services – Physical Therapist Assistant’s Rule Change • Physical therapy assistants (PTAs) are eligible for reimbursement using the HM – Less than a bachelor’s degree, modifier • The IHCP reimburses services rendered by PTA at 75 percent of the reimbursement level for a physical therapist CMS-1500 Billing 20 / October 2009 Billing Guidelines Therapy Services – Physical Therapist Assistant’s Rule Change • Indiana Administrative Code (IAC) 405 IAC 1- 11.5-2 was amended to allow for the reimbursement of services provided by certified PTAs, whether independent or hospital-based • The PTA is precluded from performing and interpreting tests, conducting initial or subsequent assessments, and developing treatment plans – Under direct supervision, a PTA is still required to consult with the supervising physical therapist daily to review treatment – The consultation can be either face-to-face or by telephone CMS-1500 Billing 21 / October 2009 Billing Guidelines Podiatric Services – Routine Foot Care • Routine foot care is only covered if a member has been seen by a medical doctor or doctor of osteopathy for treatment or evaluation of a systemic disease during the six-month period prior to rendering routine foot care • A maximum of six routine foot care services is covered per rolling 12-month period when the member has one of the following: – Systemic disease of sufficient severity that a treatment of the disease may pose a hazard when performed by a nonprofessional – Systemic conditions that result in severe circulatory embarrassment or has had areas of desensitization in the legs or feet CMS-1500 Billing 22 / October 2009 Billing Guidelines Podiatric Services – Routine Foot Care • ICD-9-CM diagnosis codes that represent systemic conditions that justify coverage for routine foot care: – Diabetes mellitus: ICD-9-CM codes 250.00-250.91 – Arteriosclerotic vascular disease of lower extremities: ICD-9-CM codes 440.20440.29 – Thromboangitis oblierans: ICD-9-CM code 443.1 – Post-phlebitis syndrome: ICD-9-CM code 459.1 – Peripheral neuropathies of the feet: ICD9-CM codes 357.1-357.7 • Routine foot care is not a covered service for Package C members CMS-1500 Billing 23 / October 2009 Billing Guidelines Podiatric Services – Routine Foot Care • Reimbursement is limited to one office visit using procedure code 99211, 99212, and 99213 per member, per 12 months, without obtaining prior authorization • New patient office visits, using procedure codes 99201, 99202, and 99203 are reimbursable at one per member, per provider, within the last three years as defined by the CPT guidelines • A visit can be billed separately only on the initial visit • For subsequent visits, reimbursement for the visit is included in the procedure performed on that date and not billed separately –Exception: If a second, significant problem is addressed on a subsequent visit, the visit code may be reported with the 25 modifier CMS-1500 Billing 24 / October 2009 Billing Guidelines Evaluation and Management Codes • Reimbursement is available for office visits to a maximum of 30 per rolling 12 month period, per IHCP member, without prior authorization (PA), and subject to the restrictions in Section 2 of 405 IAC 59-1 • Per 405 IAC 5-9-2, office visits should be appropriate to the diagnosis and treatment given and properly coded Procedure Codes 99201-99215 99241-99245 99381-99397 99401-99429 99271-99275 CMS-1500 Billing 25 / October 2009 Billing Guidelines Evaluation and Management Codes • Professional services rendered during the course of a hospital confinement must be submitted on the paper CMS-1500 claim form or using the electronic 837P transaction • The IHCP makes reimbursement in accordance with the appropriate professional fee schedule • The inpatient diagnosis-related group (DRG) reimbursement methodology does not provide payment for physician fees, including the hospital-based physician fee • New patient office visits are limited to one visit per member, per provider – once every three years CMS-1500 Billing 26 / October 2009 Crossover Claims Processing Electronic Claims • The Coordination of Benefits Contractor (COBC) crosses over HIPAA-compliant Medicare claims to the IHCP –The Centers for Medicare & Medicaid Services (CMS) selected Group Health, Inc. (GHI) to be the COBC • When Medicare-denied services cross over to the IHCP, IndianaAIM adjudicates these with a denied status • The IHCP created edits for these claims –The edits are 0592 and 0593 – Medicare denied details –Resubmit denied details separately from paid details and include the MRN from Medicare CMS-1500 Billing 27 / October 2009 Crossover Claims Processing Paper Claims • Allow 60 days for claims to automatically cross over to the IHCP • Bill denied charges to the IHCP and include the Medicare Remittance Notice (MRN) • Complete field 22 as follows: - Left side = Coinsurance, deductible, and psychiatric reduction - Right side = Medicare payment • Include the commercial payment amount in field 29 (not used for traditional Medicare) CMS-1500 Billing 28 / October 2009 Billing Guidelines Obstetric Services • The IHCP covers the following 14 antepartum visits: – Three visits in trimester one – Three visits in trimester two – Eight visits in trimester three • Providers use the following codes to bill for visits: – First visit – Evaluation and management (E/M) – 9920199205 – Visits one through six – 59425 – Seventh and subsequent visits – 59426 • Providers use the following modifiers with procedure codes: – U1 for trimester one – Zero through 14 weeks – U2 for trimester two – 14 weeks, one day through 28 weeks – U3 for trimester three – 28 weeks, one day through delivery CMS-1500 Billing 29 / October 2009 Billing Guidelines Pregnancy-Related Claims • For pregnancy-related claims, indicate the last menstrual period (LMP) in MM/DD/YY format in field 14 – The IHCP does not process claims for pregnancy-related services if there is no LMP • Indicate a pregnancy-related diagnosis code as the primary diagnosis when billing for pregnancyrelated services CMS-1500 Billing 30 / October 2009 Billing Guidelines Pregnancy Diagnosis Codes • Use normal low-risk pregnancy diagnosis codes: –V22.0 –V22.1 • Use high-risk pregnancy codes: –V60.0 through V62.9 For additional information, refer to the IHCP Provider Manual, Chapter 8, Section 4 CMS-1500 Billing 31 / October 2009 Consent Form CMS-1500 Billing 32 / October 2009 Sterilization and Partial Sterilization Partial Sterilization • A sterilization form is not necessary when a patient is rendered sterile as a result of an illness or injury – Providers must note partial sterilization with an attachment to the claim indicating “Partial Sterilization” and no consent required • Partial sterilization can also be submitted on the electronic 837P transaction when “Partial Sterilization” is indicated in the claim notes CMS-1500 Billing 33 / October 2009 Sterilization Procedure Essure • Can be performed in the office, as an outpatient or an ambulatory surgical center (ASC) • Device billed separately on CMS-1500 form using sterilization HCPCS code A9900- Miscellaneous supply, accessory, and/or service component of another HCPCS code • Use primary diagnosis code of ICD-9-CM V25.2 Sterilization • Submit cost invoice with claim • Submit a valid, signed Sterilization Consent form • Print Essure Sterilization on the claim form or on the invoice Refer to BR200734 for more information CMS-1500 Billing 34 / October 2009 Mail Order Incontinence, Ostomy, and Colostomy Supplies • Effective February 1, 2008, the Office of Medicaid Policy and Planning (OMPP) contracted with three vendors to provide incontinence, ostomy, and urological supplies to fee-forservice members: – Binson’s Home Health Care Center 1-888-217-9610 www.binsons.com – Healthcare Products Delivery, Inc (HPD) 1-800-291-8011 www.hpdinc.net – J & B Medical 1-866-674-5850 www.jandbmedical.com CMS-1500 Billing 35 / October 2009 Mail Order Incontinence, Ostomy, and Colostomy Supplies • Members obtain supplies via mail order • The policy applies to Traditional Medicaid and Care Select members only • Only paid Crossovers and TPL claims are excluded from the program – If Medicare or the TPL denies the claim, the services are limited to the 3 contracted vendors • The contracted vendors began providing services February 1, 2008 (partial implementation) • Full implementation was completed June 1, 2008 • A full listing of codes affected by this change is listed on BT200823 CMS-1500 Billing 36 / October 2009 Prior Authorization • Providers must verify member eligibility to determine the care management organization (CMO) that will process the PA or Update request – CMO information via Web interChange is real time – Send the PA request to the assigned CMO as of the date of the request – Send PA updates to the original CMO • Example: Member is assigned to MDwise on 4/3/08, when the PA is requested. On 4/15/08, the member transitions from MDwise to ADVANTAGE. On 4/23/08, the primary medical provider (PMP) requests a System Update to the PA. The PMP must request the System Update from MDwise. CMS-1500 Billing 37 / October 2009 Prior Authorization • Members can change between traditional Medicaid fee-for-service, Hoosier Healthwise/RBMC, and Care Select • When the member changes programs, the receiving organization must honor PAs approved by the prior organization for the first 30 days following the reassignment, or for the remainder of the PA dates of service, whichever comes first • Example: Member transitions from Hoosier Healthwise/RBMC to a Care Select CMO on September 15, 2008. The MCO approved PA for dates of service 9/6/08 through 10/30/08. The Care Select CMO must honor the approved PA for 30 days from September 15, 2008. CMS-1500 Billing 38 / October 2009 Prior Authorization Member Changes within a Program • When members transition from one CMO to another CMO, or from Traditional Medicaid to a CMO, the receiving organization must honor the approved PA until the PA expires CMS-1500 Billing 39 / October 2009 Prior Authorization • Each CMO is responsible for processing medical service PA requests and updates for members assigned to their organization at the time of the request • Traditional Medicaid fee-for-service PA requests are processed by ADVANTAGE Health Solutions • The PA number format is alphanumeric – Alphanumeric PA numbers will identify the CMO that processed the PA – The three Eligibility Verification Systems (EVS) will accommodate the alphanumeric value • Pharmacy PA requests continue to be processed by Affiliated Computer Services (ACS) CMS-1500 Billing 40 / October 2009 Prior Authorization Contact Information • ADVANTAGE Health Solutions (fee-for-service) P.O. Box 40789 Indianapolis, IN 46240 1-800-269-5720 1-800-689-2759 (Fax) • ACS (Pharmacy) 1-866-879-0106 1-866-780-2198 (Fax) CMS-1500 Billing 41 / October 2009 Prior Authorization Contact Information • MDwise – CMO P.O. Box 44214 Indianapolis, IN 46244-0214 1-866-440-2449 1-877-822-7186 (Fax) • ADVANTAGE Health Solutions – CMO P.O. Box 80068 Indianapolis, IN 46280 1-800-784-3981 1-800-689-2759 (Fax) CMS-1500 Billing 42 / October 2009 Code Sets The following provider types have specific code sets: • Chiropractic – April 28, 2005 • Durable Medical Equipment – February 12, 2009 • Hearing Services – February 1, 2005 • HIV Care Coordination – October 1, 2004 • Home Medical Equipment – February 12, 2009 • Optician – February 1, 2005 • Optometrist – June 24, 2008 • Transportation – September 16, 2004 • Vision – October 1, 2004 • All Code Sets can be referenced on the www.indianamedicaid.com home page CMS-1500 Billing 43 / October 2009 Fee Schedule • The IHCP Fee Schedule is available on the IHCP Web site and provides the following information: – Pricing for procedure codes – PA requirements for individual procedure codes – List of noncovered codes CMS-1500 Billing 44 / October 2009 Common Denials – CMS-1500 Claims CMS-1500 Billing 45 / October 2009 Edit 1111 Refer/PMP NPI Information Submitted Reports to Multiple LPIs • Cause — A one-to-one match cannot be established between the PMP’s National Provider Identifier (NPI) and the Legacy Provider Identifier (LPI) — Affects claims for Care Select and the Restricted Card Program • Resolution — Add the PMP’s taxonomy code to the claim in addition to the NPI — CMS-1500 • PMP Taxonomy Code: Box 17a Precede the taxonomy with Qualifier “ZZ” • PMP NPI: Box 17b CMS-1500 Billing 46 / October 2009 Edit 558 Coinsurance and Deductible Amount Missing • Cause — Coinsurance and deductible amount is missing indicating this is not a crossover claim • Resolution — Add coinsurance and/or deductible amount and/or Medicare paid amount to the CMS1500 — CMS-1500 • Add coinsurance and/or deductible amount on the left side of field 22 • Add the Medicare Payment amount on the right side in field 22 CMS-1500 Billing 47 / October 2009 Edit 1049 Care Select Member’s PMP is Missing • Cause — The member is enrolled in the Care Select Program — Affects claims for Care Select and the Restricted Card Program • Resolution — Add the member’s PMP information to the claim — CMS-1500 • PMP Taxonomy Code: Box 17a Precede the taxonomy with Qualifier “ZZ” • PMP NPI: Box 17b CMS-1500 Billing 48 / October 2009 Edit 2505 Recipient Covered by Private Insurance • Cause — This member has private insurance, which must be billed prior to Medicaid • Resolution — Add the other insurance payment to the claim — CMS-1500 • Add other insurance excluding Medicare payments to field 29 – If the primary insurance denies, the explanation of benefits (EOB) must be sent with the claim, either on paper with a paper claim, or as an attachment if claim is sent on Web interChange CMS-1500 Billing 49 / October 2009 Edit 1047 Certification Code Missing – Care Select Member • Cause — This is a Care Select member • Must have two-digit certification code from the primary medical provider • Resolution — Add the two-digit certification code from the primary medical provider for that quarter — CMS-1500 • PMP Certification Code – Box 19 CMS-1500 Billing 50 / October 2009 Edit 2017 Recipient Ineligible on Date of Service Due to Enrollment in a Managed Care Organization • Cause –The member was not eligible for fee-forservice medical assistance on the date of service because he or she was enrolled in the risk-based managed care program • Resolution –Verify eligibility on any EVS and bill the appropriate managed care organization CMS-1500 Billing 51 / October 2009 Edit 5001 Exact Duplicate • Cause –Claim being processed is an exact duplicate of a claim on the history file or another claim being processed in the same cycle • Resolution –Research prior claims billed for “paid” status CMS-1500 Billing 52 / October 2009 Edit 0593 Medicare Denied Detail • Cause –Occur when Medicare denies a detail line –Are not crossover claims –Do not include the paid detail lines on the new claim –Processed as third-party liability (TPL) claims –Include the Medicare Remittance Notice (MRN) with the claim • Resolution –Denied detail lines must be billed on a separate claim form CMS-1500 Billing 53 / October 2009 Edit 4021 Procedure Code vs. Program Indicator • Cause –Procedure code billed is restricted to a specific program • Resolution –Verify eligibility and submit claim with appropriate procedure code CMS-1500 Billing 54 / October 2009 Edit 0513 Member Name and Number Disagree • Cause –The member name and the member identification number (RID) on the claim do not match the member database • Resolution –Verify member name and RID on any EVS –Resubmit claim with corrected name and/or RID CMS-1500 Billing 55 / October 2009 Helpful Tools Avenues of Resolution • IHCP Web site at www.indianamedicaid.com • IHCP Provider Manual (Web, CD-ROM, or paper) • HCBS Waiver Provider Manual (Web) • Customer Assistance –1-800-577-1278, or –(317) 655-3240 in Indianapolis local area • Written Correspondence –P.O. Box 7263 Indianapolis, IN 46207-7263 • Provider Relations field consultant CMS-1500 Billing 56 / October 2009 Questions CMS-1500 Billing 57 / October 2009 Office of Medicaid Policy and Planning (OMPP) 402 W. Washington St, Room W374 Indianapolis, IN 46204 EDS, an HP Company 950 N. Meridian St., Suite 1150 Indianapolis, IN 46204 EDS and the EDS logo are registered trademarks of Hewlett-Packard Development Company, LP. HP is an equal opportunity employer and values the diversity of its people. ©2009 Hewlett-Packard Development Company, LP. October 2009