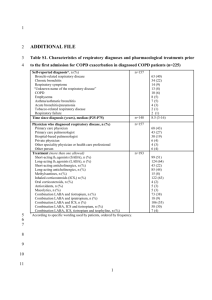
COPD
advertisement

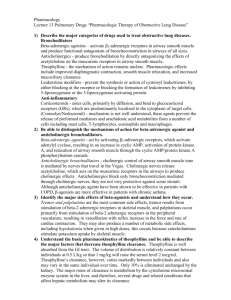
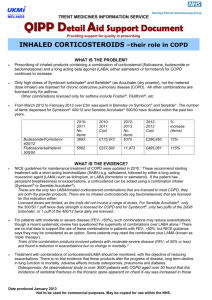
Kathleen McNamara, PharmD PGY1 Pharmacy Resident 2015-2016 NEIMEF & WHC Therapy Goals & Assessment Non-pharmacologic & Pharmacologic Therapy ◦ Medications ◦ Mechanism of Action Adverse Effects Pricing & Usual Dose Summary Reduce symptoms ◦ Relieve symptoms ◦ Improve exercise tolerance Reduce Risk ◦ Prevent disease progression ◦ Prevent & treat exacerbations ◦ Reduce mortality Classification of Severity of Airflow Limitation in COPD GOLD 1 Mild FEV₁ ≥ 80% predicted GOLD 2 Moderate 50% ≤ FEV₁ < 80% predicted GOLD 3 Severe 30% ≤ FEV₁ < 50% predicted GOLD 4 Very Severe FEV₁ < 30% predicted Cost of pre & post spirometry test at FPC: $141 Smoking cessation Immunizations ◦ Influenza Annually for all patients with COPD ◦ Pneumococcal All smokers & All patients < 65 years old with COPD Anyone > 65 years of age Regular assessment of lung function Bronchodilators ◦ Beta₂-agonists ◦ Anticholinergics Inhaled & oral corticosteroids Phosphodiesterase-4 (PDE-4) Inhibitor Methylxanthine Oxygen Patient Group Recommended 1st Choice Alternative Choice A SA Anticholinergic PRN OR SABA PRN (Grade 1A) LA Anticholinergic OR LABA OR SABA & SA Antichoinergic B LA Anticholinergic OR LABA (Grade 1B) LA Anticholinergic AND LABA C ICS + LABA &/or LA Anticholinergic LA Anticholinergic & LABA OR LA Anticholinergic & PDE-4 inhibitor OR LABA& PDE-4 inhibitor ICS + LABA &/or LA Anticholinergic (Bronchodilator Grade1B) (ICS - Grade 2B) ICS +LABA and LA Anticholinergic OR ICS + LABA & PDE-4 inhibitor OR LA Anticholinergic & LABA OR LA anticholinergic & PDE-4 inhibitor (Bronchodilator - Grade1B) (ICS - Grade 2B) D SA= Short-acting LA= Long-acting ICS= Inhaled Corticosteroid PDE-4= phosphodiesterase-4 Oxygen therapy Supplemental Therapy Pulmonary rehab Short-acting inhaled bronchodilator for acute relief of symptoms Combination of inhaled corticosteroid, long-acting β-agonist, and long-acting anticholinergic Combination of anticholinergic and β-agonist bronchodilator Stepwise Drug Therapy Pneumococcal and annual influenza vaccination, smoking cessation and regular assessment of lung function Health Care Maintenance Sutherland, 2004 Mechanism of action: Bind to beta-2 receptors causing relaxation of bronchial smooth muscle, resulting in bronchodilation. Short-acting Long-acting ◦ Albuterol (ProAir, Ventolin, Proventil) T ½= 4-6 hours ◦ Levalbuterol (Xopenex) T ½= 4 hours ◦ ◦ ◦ ◦ Formoterol (Foradil) T ½= 10 hours Salmeterol (Serevent) T ½= 5.5 hours Arformoterol (Brovana) T ½= 26 hours Indacaterol (Arcapta) T ½= 40-56 hours Mechanism of action: block the action of acetylcholine & decrease cGMP (cyclic guanosine monophosphate) in bronchial smooth muscle causing bronchodilation. Short-acting ◦ Ipratropium (Atrovent) T ½=1.5 hours Long-acting ◦ Tiotropium (Spiriva) T ½= 5-6 DAYS ◦ Aclidinium bromide (Tudorza) T ½=5-8 hours Do you choose between anticholinergic or β₂agonist? 1-yr, randomized, double-blind, doubledummy , parallel-group trial ◦ 7,376 patients Tiotropium, as compared with salmeterol: ◦ increased time to 1st exacerbation 187 vs. 145 days 17% risk reduction (hazard ratio 0.83; 95% CI 0.770.90 ◦ Increased time to 1st severe exacerbation Hazard ratio 0.72; 95% CI 0.61-0.85 ◦ Reduced annual # severe exacerbations 0.09 vs 0.13, rate ratio 0.73; 95% CI 0.66-0.82 Review of 7 clinical studies ◦ >12,000 patients with COPD Spiriva has shown to be more effective at reducing exacerbations compared with LABA ◦ OR=0.86; (95% CI 0.79-0.93) Symptom improvement & changes in lung function were similar between the two groups NO significant difference ◦ ◦ ◦ ◦ FEV Quality of life Overall all-cause hospitalizations Mortality Mechanism of action: Anti-inflammatory, exact mechanism is unknown Fluticasone (Flovent) Budesonide (Pulmicort Flexhaler) Beclomethasone (QVAR) 12-month, double-blind, parallel-group study 2485 patients with history COPD exacerbation Methods ◦ All participants received triple therapy of Spiriva, Serevent & Flovent x 6 week run-in period ◦ Then randomized to continue triple therapy or withdrawal Flovent in 3 steps over 12 weeks Primary end point: time to first moderate or severe COPD exacerbation Results ◦ Compared with continued glucocorticoid use, withdrawal met noninferiority criteria with respect to the first moderate or severe exacerbation PDE-4 Inhibitor Mechanism of action: increases cAMP levels, leading to reduction in lung inflammation ◦ Roflumilast (Daliresp) Methylxanthine Mechanism of action: true mechanism not fully understood, bronchodilation through smooth muscle relaxation and suppression of airway stimuli. ◦ Theophylline General ◦ Respiratory: 5% or more: bronchitis, cough, sore throat, rhinitis 5-16%, upper respiratory infection 5-21% ◦ GI: nausea 10%, pharyngitis 14% ◦ Neuro: feeling nervous 7%, tremor 5-7% Serevent: ◦ Musculoskeletal: pain 12% ◦ Neuro: headache 13-17% Arcapta ◦ Respiratory: cough 6-24% Atrovent ◦ Respiratory: bronchitis 10-23%, sinusitis 14% ◦ GI: xerostomia 4% Spiriva ◦ Respiratory: pharyngitis 10%, upper respiratory infection 43% (w/ powder formulation) ◦ GI: xerostomia 4% (w/ respimat spray), 12-16% (w/ powder formulation) Flovent ◦ Respiratory: sinusitis 4-10%, throat irritation 322%, upper respiratory infection 14-21% ◦ Neuro: headache 2-16% Pulmicort ◦ Respiratory: respiratory tract infection 3-38% Methylprednisone ◦ Cardio: hypertension ◦ Immunologic: at risk for infection Daliresp ◦ Endocrine metabolic: decreased weight 7-20% ◦ GI: diarrhea 10% Theophylline ◦ ◦ ◦ ◦ Cardio: tachycardia, arrhythmia GI: nausea/vomiting/diarrhea Neuro: headache Psychiatric: irritability/restlessness/insomnia SA β-agonists ProAir (albuterol) Xopenex (levalbuterol) Usual Dose Price 2 inhalations q4-6h $59.17 prn 2 inhalations q4-6h $72.46 prn LA β-agonists Foradil (formoterol) 12mcg inhaled BID $137.78 Serevent (salmeterol) 50mcg inhaled BID $312.73 Brovana (arformoterol) 15mcg inhaled BID $755.26 Arcapta (indacaterol) 75mcg inhaled daily $225.83 SA Anticholinergic Atrovent (ipratropium) Usual Dose 2 inhalations q6h prn Price $290.04 LA Anticholinergics Spiriva (tiotropium) 18mcg inhaled daily $351.41 Tudorza (aclidinium bromide) 400mcg BID $313.70 Inhaled Corticosteroids Usual Dose Price Flovent HFA (fluticasone) 1-2 inhalations BID $216.22 Pulmicort Flexhaler (budesonide) QVAR (beclomethasone) 1-2 inhalations BID $156.63 1-2 inhalations BID $150.00 40-80mg daily in 1-2 divided doses Usual Dose then taper $27.75 500mcg daily $287.83 (#30) 300mg ER BID $57.80 (#100) Systemic Corticosteroids methylprednisolone Phosphodiesterase-4 Inhibitor Daliresp (roflumilast Methylxanthine Theophylline 300mg ER Price Combination Products Usual Dose Price Combivent (albuterol/ipratropium) 1 inhalation QID $329.44 Advair 100/50 (salmeterol/fluticasone) 1 inhalation BID $278.46 Symbicort 160 (formoterol/budesonide) 2 inhalations BID $306.35 Stiolto Respimat (tiotropium/olodaterol) 2 inhalations QD $ 340.00 Breo Ellipta (fluticasone/vilanterol) 1 inhalation QD $320.00 Generally NOT indicated for majority of patients with COPD. BUT, some antibiotics (macrolides) may have anti-inflammatory effects in addition to antibiotic effect. ◦ May be appropriate for continued, frequent exacerbations despite optimal therapy with bronchodilators and anti-inflammatory agents. Chong J, Karner C, Poole P. Tiotropium versus long-acting beta-agonists for stable chronic obstructive pulmonary disease (Review). The Cochrane Collection. Published by John Wiley & Sons, Ltd. Global Strategy for the Diagnosis, Management, and Prevention of COPD. Scientific information and recommendations for COPD programs. Updated 2015. Magnussen, Disse, Rodriguez-Roisin, et al. Withdrawal of Inhaled Glucocorticoids and Exacerbations of COPD. NEJM 371;14. 2 October, 2014. Micromedex Drug Index Thank you!