Popliteal Artery Aneurysm - VCU Department of Surgery
advertisement
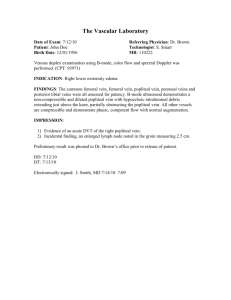
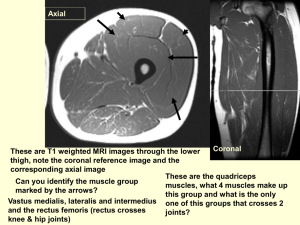
VCU Death and Complications Conference Rajesh Ramanathan VAMC Vascular Surgery 9/18/14 Case History 61yo man presented to OSH ED with acute complaints of blue discoloration of the left great toe + petechaie along the left shins Case History 61yo man presented to OSH ED with acute complaints of blue discoloration of the left great toe + petechaie along the left shins US with 4x6cm popliteal aneurysm with intramural thrombus Placed on heparin ggt and transferred to Richmond VAMC RESIDENT 1 1. Rough percentage of men who have popliteal artery aneurysms? 2. What is the percentage of contralateral popliteal artery aneurysm? 3. What is the percentage of infra-renal aortic aneurysm in the setting of unilateral popliteal artery aneurysm ANSWERS • Male = 95% to 100% of patients • Contralateral aneurysms were found ~ 50% • Aortic aneurysms in 36% to 51% Hospital Course No pain/discomfort/parasthesias. No h/o claudication, abdominal/back pain. PMH: HTN | PSH: wrist surgery | SH: 1ppd tobacco, beer daily Meds: Amlodipine, lisinopril Afebrile, 164/104, 90, 20 Abd: soft, no pulsatile mass Left side: +femoral pulse, easily palpable popliteal pulse, petechia over left foot dorsum extending proximally, palpable DP and PT Right side: +femoral and distal pulses. No sensory/motor deficit RESIDENT 2 You have 62 year old male who has a popliteal artery aneurysm. He undergoes lysis for distal emboli. What is the common “lytic” medicine that is used, what is its mode of action, what labs must you follow why “lysis” treatment? ANSWERS • Tissue plasminogen activator • 1 mg/hr • Fibrinogen • > 150 - continue • 100 – 150 - half • Less 100 - stop RESIDENT 3 You have 54 year old male with a focal 4 cm popliteal artery aneurysm confined to the popliteal space. How would you approach other than a above to below the knee popliteal artery bypass. Describe your incision. 1st operation Pre-op vein mapping identified adequate GSV on both sides CTA with high AT take-off Operation: - Ligation of below-knee popliteal artery - Ligation and transposition of AT to tibio-peroneal trunk - Femoral-tibioperoneal bypass using in-situ saphenous vein - Due to the lie of the vein, kink noted about 5cm proximal to distal anastamosis, but good signals distally Post-operative course End of case in OR: weak PT pulse and DP signal PACU: no DP or PT signal Stat duplex: flow in the bypass but no distal flow Heparin ggt started and taken back within 2.5 hours of first operation 2nd operation - Distal wound opened above distal anastamosis - Thrombosed conduit – Fogarty-thrombectomized - Distal Fogarty with thrombus - AT transposition open with evidence of retrograde flow - Distal anastamosis taken down, vein cut back and reanastomosed, with no obvious kink - Triphasic signals distally in tibioperoneal trunk and signals present in the AT Summary • Was the complication potentially avoidable? – Yes: Technical error • Would avoiding the complication change outcome? – Yes: Reoperation • What factors contributed to the complication? – Kink in the vein leading to increased turbulence and diminished flow distally – Technical anastomotic narrowing Popliteal aneurysms • 30:1 ratio in males:females • 60-70y onset • Those with AAA: ~10% have popliteal aneurysm • Those with Pop. Aneurysm: Bilateral in 60-70% AAA in 40-50% of those with popliteal aneurysm (70% in those with bilateral pop. a.) • Associations: Tobacco, HTN, DM • Most asymptomatic at diagnosis • 50% present with claudication Popliteal aneurysms • Complications: – Thrombosis 40% – Embolization 25% – Rupture <5% • Treatment – Repair if >2cm – If no complication: AAA first, then popliteal – If limb-threatening: Pop first then AAA • Outcomes: – Before ischemic complications: 5 & 10 year patency >80% – After complications: 60% and 48% at 5 & 10 years Evaluation of the Vascular Study Group of New England registry for patient undergoing lower extremity bypass Discharge and 1-year graft patency compared between surgeons who used routine (>80%) vs. selective completion 48 surgeons (33% routine), 2032 LEB, 67.4% imaging Increased imaging in ESRD, elective surgery, GSV, distal bypass No improvement in graft patency at discharge or at 1-yr