AIC November 15, 2012 Webinar Presentation
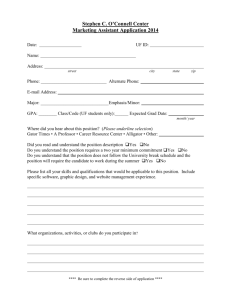
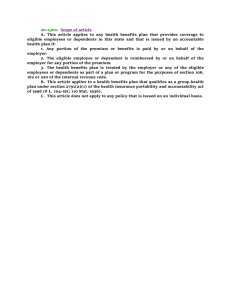
advertisement

Association Insurance Cooperative PPACA 2013 – 2014 Presentation Handouts: Click Here PPACA Topology Minimum Essential Coverage Minimum Value Health Insurance Premium Tax Credit Employer Shared Responsibility Payment Essential Health Benefits Compliance With Cost-Sharing Limits Affordable Premiums Disclosure of Return Information Qualified Health Plans (QHPs) State Essential Benefits Package Option Large/Small Employer Employer Penalty Flow Chart Pay or Play Strategies by Employer Size Affordable Care Act Tax Provisions http://www.irs.gov/uac/Affordable-Care-Act-Tax-Provisions Minimum essential coverage means coverage under any of the following: Government-sponsored program – such as Medicare Part A, Medicaid, the CHIP program An “eligible employer-sponsored plan” A health plan offered in the individual market A grandfathered health plan; or Other health benefits coverage (such as a State health benefits risk pool) Minimum Value On April 26, 2012, the Department of the Treasury and IRS issued Notice 2012-31, which provides information and requested public comment on an approach to determining whether an eligible employersponsored health plan provides minimum value. Starting in 2014, whether such a plan provides minimum value will be relevant to eligibility for the premium tax credit and application of the employer shared responsibility payment. Affordable Care Act Tax Provisions http://www.irs.gov/uac/Affordable-Care-Act-Tax-Provisions Health Insurance Premium Tax Credit Starting in 2014, individuals and families can take a new premium tax credit to help them afford health insurance coverage purchased through an Affordable Insurance Exchange. Tax credits or subsidies are provided to purchase health insurance through the exchange on a sliding scale to individuals and families with incomes up to 400% of the federal poverty level(under current guidelines, about $92,000 a year). The portion of the law that will allow eligible individuals to use tax credits to purchase health coverage through an Exchange is not effective until 2014. Affordable Care Act Tax Provisions http://www.irs.gov/uac/Affordable-Care-Act-Tax-Provisions Employer Shared Responsibility Payment Starting in 2014, certain employers must offer health coverage to their full-time employees or a shared responsibility payment may apply. Information may be found in news releases IRS-2011-92 and IRS-2011-50 and Notices 2011-73, 2011-36 and 2012-17. Additionally, Notice 2012-58 expands upon and modifies previous guidance and describes safe harbors that employers may use to determine whether certain workers are full-time employees and to establish that coverage is affordable at least through the end of 2014. Notice 2012-59 provides related guidance for group health plans on the waiting periods they may apply before starting coverage. Essential Health Benefits To be defined by regulations, but they include minimum benefits in ten general categories and the items and services covered within those categories: Ambulatory patient services Emergency services Hospitalization Maternity and newborn care Mental health and substance use disorder services, including behavioral health treatment Prescription drugs Rehabilitative and habilitative services and devices Laboratory services Preventive and wellness services and chronic disease management Pediatric services, including oral and vision care. Employer Must Comply With Cost-Sharing Limits The four prescribed coverage levels vary based on the percentage of full actuarial value of benefits the plan is designed to provide, as follows: Bronze: designed to provide benefits actuarially equivalent to 60% of full value; Silver: designed to provide benefits actuarially equivalent to 70% of full value; Gold: designed to provide benefits actuarially equivalent to 80% of full value; Platinum: designed to provide benefits actuarially equivalent to 90% of full value. The Kaiser Foundation estimates that the annual deductible for a bronze plan could range from $2,750 to $6,350 Affordable Premiums Individuals who get insurance through their employer can get subsidized coverage in an Exchange if their premiums are unaffordable (more than 9.5 percent of their household income) or the plan is inadequate (pays less than 60 percent of the cost of covered benefits). Disclosure of Return Information On April 27, 2012, the Department of the Treasury and the IRS issued proposed regulations with rules for disclosure of return information to be used to carry out eligibility determinations for advance payments of the premium tax credit, Medicaid and other health insurance affordability programs. The proposed regulations solicit public comments. ◦ Reporting Employer Provided Health Coverage in Form W-2 The Affordable Care Act requires employers to report the cost of coverage under an employersponsored group health plan on an employee’s Form W-2, Wage and Tax Statement, in Box 12, using Code DD. Informational only. No final guidance for this reporting requirement. FSA Limit Effective January 1, 2013 - Limits the amount of contributions to a flexible spending account for medical expenses to $2,500 per year, increased annually by the cost of living adjustment. Health Plan Requirements TD 9575 and REG-4003810, issued by DOL, HHS and IRS, provide information on the summary of benefits and coverage and the uniform glossary. Notice 2012-59 provides guidance to group health plans on the waiting periods they may apply before coverage starts – 90 day Employers are required provide all new hires and current employees with a written notice about the health benefit Exchange and some of the consequences if an employee decides to purchase a qualified health plan through the Exchange in lieu of employer-sponsored coverage. This disclosure requirement is generally effective for employers in a state beginning on March 1, 2013. Employees hired on or after the effective date must be provided the Notice of Exchange at the time of hiring. Employees employed on the effective date must be provided the Notice of Exchange no later than March 1, 2013). PPACA Topology Qualified Health Plans (QHPs) Minimum Essential Coverage Minimum Value Health Insurance Premium Tax Credit Employer Shared Responsibility Payment Essential Health Benefits Compliance With Cost-Sharing Limits Affordable Premiums Disclosure of Return Information State Essential Benefits Package Option Large/Small Employer Employer Penalty Flow Chart Pay or Play Strategies by Employer Size Health Insurance Exchanges Qualified Health Plans (QHPs): An Exchange will be required to make qualified health plans (QHPs) available to qualified individuals and qualified employers. An Exchange cannot make available any health plan that is not a QHP. A qualified health plan (QHP) is an Exchange-certified “health plan” that offers an “essential health benefits package.” To provide the essential health benefits package, a plan must provide: essential health benefits; limit cost-sharing; provide either bronze, silver, gold, or platinum level coverage (that is, benefits that are actuarially equivalent to 60%, 70%, 80%, or 90% (respectively) of the full actuarial benefits provided under the plan State Essential Benefits Package Option One of the three largest products in the small group market in the state ◦ New Mexico: Lovelace One of the three largest health plans offered to federal or state employees The Health Maintenance Organization (HMO) with the largest commercial enrollment in the state PPACA Topology Qualified Health Plans (QHPs) Minimum Essential Coverage Minimum Value Health Insurance Premium Tax Credit Employer Shared Responsibility Payment Essential Health Benefits Compliance With Cost-Sharing Limits Affordable Premiums Disclosure of Return Information State Essential Benefits Package Option Large/Small Employer Employer Penalty Flow Chart Pay or Play Strategies by Employer Size PPACA Topology Minimum Essential Coverage Minimum Value Health Insurance Premium Tax Credit Employer Shared Responsibility Payment Essential Health Benefits Compliance With Cost-Sharing Limits Affordable Premiums Disclosure of Return Information Qualified Health Plans (QHPs) State Essential Benefits Package Option Large/Small Employer Employer Penalty Flow Chart Pay or Play Strategies by Employer Size Putting the Numbers Together Example A: Employee earns $35,000 per year as reported on W-2 Penalty Flow Chart Question: Do any employees have to pay more than 9.5% of family income (regulation revised to use W-2 wages) for the employer coverage? 1. In this example: Average Full-Time eligible employee earns $35,000.00 (as reported on W-2). 2. Affordable Insurance for the employee is 9.5% = $3,335.00. 3. $3,335÷12 = $277.00 is the maximum monthly portion of W-2 that the employee should pay for insurance and not trigger a penalty based on affordability. What is the minimum monthly insurance premium that the employer must pay and avoid the penalty based on affordability and the employer mandate? 1. The actuarial value of a Bronze Plan based on an employee share of .40% and an employer share of 60%. Taking the $277.00 monthly maximum employee premium share ÷ .40% will equal $692.50 per month. What is the employer cost sharing/month using a Bronze Plan as the baseline? Employee Portion Employer Portion Monthly Premium Bronze: @40% = $277.00 @60% = 415.50 $692.50 Silver: @30% = $ 207.75 @70% = 484.75 $692.50 Gold: @20% = $138.50 @80% = 554.00 $692.50 Platinum: @10% = $ 69.25 @90% = 623.25 $692.50 Putting the Numbers Together Example B: Employee earns $12,000 per year as reported on W-2 Penalty Flow Chart Question: Do any employees have to pay more than 9.5% of family income (regulation revised to use W-2 wages) for the employer coverage? 1. In this example: Average Full-Time eligible employee earns $12,000.00 (as reported on W-2). 2. Affordable Insurance for the employee is 9.5% = $1,140.00. 3. $1,140÷12 = $95.00 is the maximum monthly portion of W-2 that the employee should pay for insurance and not trigger a penalty based on affordability. What is the minimum monthly insurance premium that the employer must pay and avoid the penalty based on affordability and the employer mandate? 1. The actuarial value of a Bronze Plan based on an employee share of .40% and an employer share of 60%. Taking the $95.00 monthly maximum employee premium share ÷ .40% will equal $237.5 per month. What is the employer cost sharing/month using a Bronze Plan as the baseline? Employee Portion Employer Portion Monthly Premium Bronze: @40% = $95.00 @60% = 142.00 $237.50 Silver: @30% = $71.10 @70% = 165.90 $237.50 Gold: @20% = $47.40 @80% = 189.60 $237.50 Platinum: @10% = $23.70 @90% = 213.30 $237.50 PPACA Topology Minimum Essential Coverage Minimum Value Health Insurance Premium Tax Credit Employer Shared Responsibility Payment Essential Health Benefits Compliance With Cost-Sharing Limits Affordable Premiums Disclosure of Return Information Qualified Health Plans (QHPs) State Essential Benefits Package Option Large/Small Employer Employer Penalty Flow Chart Pay or Play Strategies by Employer Size Your Company is Grandfathered Grandfathered Health Plans – ACA Exceptions www.healthcare.gov/law/features/rights/grandfathered-plans/index.html Grandfathered Plan: March 23, 2010 and not make any major changes in coverage Examples of changes in coverage that would cause a plan to lose grandfathering include: • Eliminating benefits to diagnose or treat a particular condition. • Increasing the up-front deductible patients must pay before coverage kicks in by more than the cumulative growth in medical inflation since March 23, 2010 plus 15 percentage points. • Reducing the share of the premium the employer pays by more than five percentage points since March 23, 2010. Alternatives: Self-Fund; Defined Contribution Arrangement Your Company Employs Under 50 FTEs No financial requirements to contribute toward workers’ health care costs Have most to gain under the ACA Tax credits for some to maintain or begin offering coverage started in 2010 ◦ Credit varies with employer size and average wage ◦ As of 2014 employer can only get them for 2 consecutive years; For 25 or fewer workers - max tax credit of 35% of employer contribution now, 50% starting in 2014. Small group health insurance market already has guaranteed issue http://www.statehealthfacts.org/comparetable.jsp?ind=350&cat=7 2014 – new insurance options through SHOP exchanges Your Company Employs Under 50 FTEs Considerations: Those with Group Coverage – Group Insurance Rates Will Increase Significantly in 2014 10 plus FTEs – Self Fund with a comprehensive insurance carrier Defined Contribution Arrangement In 2014, employees earning less than 400% of the Federal Poverty Level ($92,000 for a family of four) per year who purchase a personal policy will receive a federal subsidy on their premium if their company doesn’t offer a group plan. o Every employer with less than 50 employees should switch from group coverage to simply giving employees tax-free allowances via an HRA to purchase their own individual policy. o Currently, employers and their employees can save up to 50% in 2013 by switching now to individual vs. group health insurance. o Large employers are already implementing Sears (60K FT/45K PT); Darden (olive Garden, Red Lobster) Your Company Employs 50 to 100 FTEs Same option as smaller employers to purchase coverage through the exchanges Considerations: ◦ Play or Pay? ◦ Group Insurance Too Expensive ◦ High Deductible Health Plan + GAP ◦ Self-Fund ◦ Defined Contribution Arrangement Your Company Employs 101+ FTEs Almost all currently offer health insurance - 90% in 2010 and coverage unlikely to change Same penalties as outlined for mediums No access to Exchange/SHOP options until 2017 Group Insurance Will Cost will Continue to Increase Expense Incurred Mini-Meds Gone 2014 Considerations: ◦ Play or Pay? ◦ High Deductible Health Plan + GAP ◦ Self-Fund ◦ Defined Contribution Arrangement SELF-INSURED PLANS DEFINED CONTRIBUTION PLANS Links and Contact Information AIC Website: www.AssociationInsurance.us Handouts: Click Here Kenneth Lee: Email: klee@mynpi.org Phone: 765.352.1776