Status Epilepticus 2 - Pediatric Emergency Medicine Database
advertisement

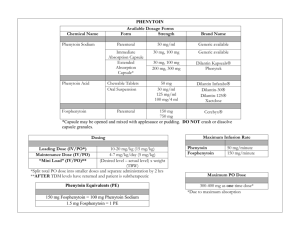
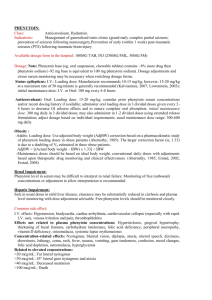
Status Epilepticus Stan Bernbaum MD CCFP-EM May 31, 2001 Outline - Status Epilepticus (SE) Case Presentation Definitions Epidemiology Clinical Features Causes / Outcomes Pathophysiology Management * – General – Drugs CASE Patient BNW - 14 month female PMH: -Recurrent Grand Mal seizures since birth, lasting up to 1 hour -On meds: Carbamazepine, Topiramate, & Clobazam -Family had detailed instructions from neurologist regarding management of her seizures HX: -Unwell all day- frequent vomiting, fever -Generalized tonic-clonic seizures began 1/2 hr ago -Presents to ER at PLC by EMS having generalized convulsions CASE - continued P/E: -Generalized seizure activity, drooling, shallow respirations; being bagged by EMS -Pale, warm, diaphoretic -VS: P 180, R 28, T 40.3, Sat 88% CASE - continued Management: AT HOME: -Had been given Lorazepam PR 0.1 mg/kg by father -EMS repeated Lorazepam PR, and also gave Midazolam IM 0.2 mg/kg -Glucometer by EMS - 7.2 -IV started just before arrival at hospital CASE - continued MANAGEMENT IN EMERGENCY: -Bagging --> O2 sat 100% -Lorazepam 0.1 mg/kg IV -Phenytoin 20 mg/kg IV over 20 min -Acetaminophen 15 mg/kg supp -pt exposed to help cool -ABG, labs drawn ......still seizing CASE - continued MANAGEMENT IN ER - continued: -Lorazepam 0.1 mg/kg repeat -consults - Peds PLC - Ped Neurologist and ICU @ ACH -O2 sat still 100% -ordered Phenobarbital 20 mg/kg IV ......still seizing CASE - continued MANAGEMENT IN ER - continued: -ABG: pH 7.01 pCO2 elevated (other results not in chart) -Thiopental 5 mg/kg -Intubated (#5 uncuffed ET tube) ...... seizure activity stopped. -Phenobarbital given (from previous order) CASE - continued MANAGEMENT IN ER - continued: repeat ABG: pH 7.4 pO2 359 sat 99 pCO2 18 HCO3 13 BE -9 Lactate 3.8 Gluc 8.3 CBC OK Na 144 K 3.2 Cl 108 CO2 12 A Gap = 24 -transferred to ACH ICU via transport team Severe Myoclonic Epilepsy in Infants recognized as a syndrome in 1982 features: – – – – – – – family history of epilepsy or febrile convulsions seizures begin during first year of life very resistant to all treatment unknown etiology ataxia, pyramidal signs, & myoclonus develop psychomotor development retarded from 2nd year all have intellectual deficiency Outline - Status Epilepticus (SE) Case Presentation Definitions Epidemiology Clinical Features Causes / Outcomes Pathophysiology Management * – General – Drugs Definition - Status Epilepticus continuous or rapidly repeating seizures no consensus on exact definition - “abn prolonged” – “no recovery between attacks” – “20-30 min” --> injury to CNS neurons – more practical definition: since isolated tonic clonic seizures rarely last > few minutes ... consider Status if sz > 5 min or 2 discrete sz with no regaining of consciousness between vs. serial sz - close together - regained consciousness in between Outline - Status Epilepticus (SE) Case Presentation Definitions Epidemiology Clinical Features Causes / Outcomes Pathophysiology Management * – General – Drugs Epidemiology - SE life threatening USA: -102,000 -152,000 cases / year - 52,000 deaths / year of new cases of epilepsy, 12 -30% present in Status generalized Status is most common form - and subject of this review Outline - Status Epilepticus (SE) Case Presentation Definitions Epidemiology Clinical Features Causes / Outcomes Pathophysiology Management * – General – Drugs Clinical - Generalized SE at onset - usu obvious tonic / clonic as continues often subtle - slight twitch of face / extremities, nystagmoid eye movements may be NO observable motor sz ***still risk for CNS injury - assume still seizing if SE pt not waking » need EEG to definitely dx - not uncommon in comatose hospital inpatients Outline - Status Epilepticus (SE) Case Presentation Definitions Epidemiology Clinical Features Causes / Outcomes Pathophysiology Management * – General – Drugs Outcome of SE overall adult mortality 20% (>80 yr : 50%) – >90% mortality is d/t underlying disease – children - better outcomes - mortality 2.5 % increase risk future SE / chronic sz worse outcome if prolonged / severe physiologic disturbance outcome depends on cause - acute vs chronic Outcome of SE continued Acute causes - difficult to control / higher mortality – – – – – sepsis - esp CNS CNS - infx, stroke, head trauma, neoplasm drug toxicity hypoxia metabolic encephalopathy » abn lytes, renal failure Outcome of SE continued Chronic causes - usu better response to Rx – known epilepsy - breakthrough sz +/- low anticonvulsant levels – ETOH / drug abuse / withdrawal – remote CNS process (eg brain surgery / CVA / trauma) --> SE after long latent period Outline - Status Epilepticus (SE) Case Presentation Definitions Epidemiology Clinical Features Causes / Outcomes Pathophysiology Management * – General – Drugs Pathophysiology - SE numerous mechanisms - poorly understood – failure of mechanisms that usu abort isolated sz – excess excitation or ineffective inhibition – there are excitatory and inhibitory receptors in the brain - activity is usually in balance Pathophysiology - SE cont’d GLUTAMATE = the major excitatory AA neurotransmitter in brain – any factor which increases Glutamate activity can lead to seizures – e.g. 1987- mussels contaminated with Domoic acid, a glutamate analog --> profound SE / deaths Pathophysiology - SE continued GABA = main inhibitory neurotransmitter – GABA antagonists can cause SE eg Penicillins, other antibiotics – prolonged sz can desensitize GABA receptors Pathophysiology - SE continued CNS damage can occur - mechanism: – uncontrolled neuronal firing -> excess glutamate -> this sustained high influx of calcium ions into neurons leads to cell death (“excitotoxicity”) – GABA released to counteract this, but GABA receptors eventually desensitize – these effects worsened if hyperthermia, hypoxia, or hypotension Pathophysiology - SE continued PHASE 1 (0-30 min) -- compensatory mechanisms remain intact – – – – – adrenaline or noradrenaline release ++ increased CBF & metabolism hypertension, hyperpyrexia hyperventilation, tachycardia lactic acidosis Pathophysiology - SE continued PHASE 2 (>30 min) -- compensatory mechanisms failing – – – – – – – cerebral autoregulation fails / cerebral edema respiration depressed cardiac arrhythmias hypotension hypoglycemia, hyponatremia renal failure, rhabdomyolysis, hyperthermia DIC Outline - Status Epilepticus (SE) Case Presentation Definitions Epidemiology Clinical Features Causes / Outcomes Pathophysiology Management * – General – Drugs OUTLINE - Management of SE General approach Anti - Epileptic Drugs: – – – – – Benzodiazepines Phenytoin / Fosphenytoin Barbiturates Propofol others / new possibilities Management of SE ABC’s (+ monitor / O2 / large IV’s) START PHARMACOTHERAPY ASAP Metabolic acidosis common - if severe, give Bicarb if intubating / ventilating - avoid long-acting n-m blockers - masks sz activity beware hyperthermia 2º sz - in 30-80% --> passive cooling Management of SE continued consider underlying causes: – – – – infection (systemic / CNS) structural: trauma, CVA, IC bleed CNS malformations metabolic - hypoxia, abn electrolytes, hypoglycemia – toxic - alcohol, other drugs – drug withdrawal - AED’s, benzos – congenital - inborn errors of metabolism Management of SE continued History & Physical - do once Rx initiated Hx: events, trauma, meds, sz hx, ETOH, infx P/E: Neuro - look for focal signs vs. generalized tonic-clonic – look for signs of underlying causes - trauma, infection, etc LAB: gluc, lytes, creat, BUN, CBC, Ca, Mg, Phos, LFT’s, AED levels, ETOH / toxicology, PTT / INR -ABG Management of SE continued consider.... – Thiamine – Glucose – Pyridoxine 5 gm IV (70 mg/kg kids) » reverses INH action inhibiting GABA synthesis » now recommended routinely by NYC Poison Control in REFRACTORY SE d/t frequency of INH OD OUTLINE - Management of SE General approach Anti - Epileptic Drugs: – – – – – Benzodiazepines Phenytoin / Fosphenytoin Barbiturates Propofol others / new possibilities Drug Rx of SE Starting Rx ASAP has been correlated with a better response rate to drug Rx, and lower morbidity – Lowenstein DH, Alldredge BK Neurology 1993 (43): 483-8 » < 30 min - 80% stopped » > 120 min - < 40% stopped but - retrospective review; ? groups comparable Drug Rx of SE Ideal agent characteristics: – – – – easy to administer prompt onset, long-acting 100% effective vs seizures no depression of cardio-resp function or mental status – no other adverse effects Drug Rx of SE Existing agents - adverse effects: – Benzos / Bbts - decrease LOC / respiration – Dilantin / (Fosphenytoin) - infusion rate-related hypotension / dysrhythmias – Dilantin / Bbts / (Fosphen) - slow onset d/t limited rate of administration Drug Rx of SE 1st - Benzodiazepines * Lorazepam, Diazepam 2nd - Phenytoin, Fosphenytoin 3rd - Phenobarbital Drug Rx - Refractory SE Anesthetic doses of: – Midazolam (0.2 mg/kg slow IV bolus) - >continuous IV infusion @ .4 - 6.0 mcg/kg/min OR .1 - 2.0 mg/kg/hr – Propofol (1-2 mg/kg) – Barbiturates (Thiopental, Phenobarbital, Pentobarbital) – Inhalational anesthetics (Isoflurane) GA can suppress immune system -->infection Non - IV Rx of SE e.g. out of hospital -- often in children – – – – Midazolam IM (or Intranasal) .15-.3 mg/kg Diazepam Rectally .5 mg/kg (to 20 mg) Lorazepam SL (Paraldehyde rectally) Lorazepam 1st agent to use Dose: Adults 4 -10 mg (.1 mg/kg) IV Peds .05 - .1 mg/kg (to 4 mg) IV less lipid soluble than Diazepam --> smaller volume of distribution / longer T1/2 – effects last 12 - 24 hr S/E: resp depression, hypotension, confusion, sedation (but less than diazepam) Diazepam Dose: Peds .1-1.0 (.2-.5) mg/kg IV » Adults 10 - 20 mg (.2 mg/kg) IV Duration of action: < 1 hr Lorazepam vs. Diazepam Duration of action Onset of action Sedation Lorazepam Diazepam *12-24 hr *< 1 hr 2-3 min 1-3 min + ++ Midazolam Dose: .2 mg/kg IV 5-10 mg IM 0.2 mg/kg Intranasal Dose for refractory SE - continuous IV infusion @ .1 - 2.0 mg/kg/hr - titrated Onset: IV 2 - 3 min / other routes 15 min Duration: 1 - 4 hr Phenytoin (Dilantin) still the standard 2nd IV Rx after Benzo dose: 18 - 20 mg/kg (better than “1 gram”) IV solution is highly alkaline - dissolved in propylene glycol, alcohol, and NaOH - pH is 12 -give in large vein, dilute N/S, flush rate: Š 50 mg / min (Peds: Š1 mg/kg/min) onset of action: 10 - 30 min duration of action: 12 - 24 hr Phenytoin continued S/E - (most avoided if slower administration) – hypotension – arrhythmias - (must monitor) – respiratory depression – venous irritation – extravasation -->tissue injury / necrosis – “purple glove syndrome”: progressive limb edema, discoloration and pain 2-12 hr post IV admin Fosphenytoin a prodrug of Phenytoin – it has no anticonvulsant action itself, but is rapidly converted to Phenytoin – Dosage: in “Phenytoin Equivalents” to attempt to avoid confusion – Molecular wt = 1.5 x Phenytoin ... so 1.5 mg Fosphen --> 1 mg Phenytoin – can safely give at 3x rate of Phenytoin, resulting in 2x amount of Phenytoin delivered Fosphenytoin Advantages over Phenytoin: – pH 8 (vs Phenytoin pH 12) – does not require solvent (Phenytoin is dissolved in propylene glycol) » can give IM when no IV access » IV: - less potential for irritation - can give faster - no risk of tissue necrosis if goes interstitial - does not precipitate in IV solutions – lower risk of hypotension and dysrhythmias Fosphenytoin Negative considerations: – COST Approx 20x that of Phenytoin – CONFUSION of ordering in “Phenytoin equivalents” » can give IV at rate of 150 PE/min, which delivers 100 mg/min of Phenytoin » 750 mg Fosphen = 500 mg PE - One UK hospital expresses orders in both units ie “500 mg PE (750 mg Fosphen)” Fosphenytoin confusion: – case report (Epilepsia 42(2): 288, 2001) - 25 yo female given infusion of Phenytoin (mistaken for Fosphenytoin) at 150 mg/min » bradycardia to 34 » BP dropped to 45/0 » asystole » oops. » resuscitated with CPR ( x 15 min), intubation, atropine, isoproterenol Fosphenytoin – NOTES both Fosphen (Cerebyx) and Dilantin are marketed by Parke-Davis Fosphen was developed to solve problems associated with parenteral Phenytoin, and eventually replace it P-D have stopped making IV Dilantin - but generic IV Phenytoin still available Fosphenytoin minor S/E similar to Phenytoin (since is converted to Phenytoin): – nystagmus, dizziness, headache, somnolence, ataxia; – MORE pruritus & paraesthesias, esp in groin area - responds to Benadryl Despite giving more rapidly, not shown to have more rapid onset of action Barbiturates in use since 1912 general CNS depressant activity – raise threshold of most neuronal pathways to direct and indirect stimulation – at high levels, slows EEG --> burst suppression and ultimately electrocortical silence – mechanism of action not clearly defined S/E: resp depression, hypotension Phenobarbital Dose: 20 mg/kg IV (range 10-40 mg/kg) -usu maximum 1 gm Maximum rate: 100 mg/min onset of action: 10 - 20 min duration of action: 1 - 3 days Phenobarbital IV Phenobarb in Refractory SE: – as effective as Diazepam plus Phenytoin, but S/E more pronounced – because of profound hypotension & respiratory depression, patient will likely need intubation & ventilation at this point; (and will need ICU admission and continuous EEG monitoring if SE persists) Pentobarbital Dose: 5 - 12 mg/kg Rate: 5 - 20 mg/min – once SE resolved -maintenance: 1-10 mg/kg/hr Thiopental Dose: 2-5 mg/kg IV rapid onset: 30 - 60 sec short duration: 20 - 30 min S/E: – CV depression, hypotension, arrhythmias – resp depression, apnea Thiopental Thiopental - negative aspects: – – – – accumulates in fatty tissues an active metabolite - Pentobarbital long recovery time after infusion hemodynamic instability Propofol Dose: 1-2 (3-5) mg/kg Rate: 5-10 mg/min (1-15 mg/kg/hr) Onset: 2-4 min Half-life: 30-60 min does not accumulate --> rapid recovery Mechanism: – stimulates GABA receptors (like Benzos/Bbts) – suppresses CNS metabolism Propofol study in rodent model of refractory SE (Ann Neurol 2001; 49: 260-63 M. Holtkamp) * showed effective resolution of refractory SE using Propofol at sub-anesthetic doses (50 mg/kg intraperitoneally) in 5 / 5 animals given that dose * Diazepam effective in 3 / 4 animals at similarly high dose Propofol Advantages over Barbiturates – less hypotension – more rapid onset of action – rapid elimination “Pro-convulsant effect” - is now thought to be myoclonus, unlikely a significant problem Paraldehyde an old agent, but has uses: – when no IV - rapid IM or PR absorption – effective vs ETOH withdrawal seizures / SE Dose: .1 - .15 ml/kg has fallen out of favor because: – – – – smells very bad - an aromatic aldehyde degrades easily, which increases toxicity decomposes plastic syringes & tubing < 2 min significant toxicity - other agents safer Possible new drugs for Status Lidocaine - some positive trials Valproate - IV form available »15-20 mg/kg IV. Not studied yet in SE Gabapentin / Vigabatrin / Lamotrigine Felbamate - blocks NMDA receptors Ketamine - blocks NMDA receptors Ketamine in SE blocks NMDA receptors - this may protect brain from effects of excitatory NT’s – may be neuroprotective as well as antiepileptic some animal studies have demonstrated control of refractory SE with Ketamine: Ketamine Controls Prolonged SE - DJBorris Epilepsy Research 42 (2000): 117-22 – more efffective than Phenobarb in LATE SE (>60 min); not as effective in EARLY SE Ketamine in SE has NOT been studied in SE in the Emergency setting Consensus Guidelines Rx of Status Ep. in Children by the Status Epilepticus Working Party Britain 2000 based on literature search of Ped SE papers in English ; >1100 found, though only 2 were pediatric RCT’s – they admit these are more practice-based than evidence-based Consensus Guidelines: if IV Access 1. Lorazepam 0.1 mg/kg (over 30-60 sec) 2. Lorazepam - repeat 3. Phenytoin 18 mg/kg (“over 20 min”) »OR Phenobarbital 20 mg/kg (“over 10 min”) if already on Phenytoin »AND Paraldehyde rectally 0.4 ml/kg in same volume olive oil 4. RSI - Thiopental induction 4 mg/kg Consensus Guidelines: if NO IV Access 1. Diazepam 0.5 mg/kg rectally 2. Paraldehyde 0.4 ml/kg rectally start intraosseous if still no IV then follow IV algorithm – 4. RSI using Thiopental – 3. Phenytoin / Phenobarb; plus Paraldehyde rectally Consensus Guidelines Suggestions for future: – compare rectal with buccal midazolam – compare IV Fosphenytoin with IV Phenytoin – for refractory SE, after algorithm, consider » midazolam infusion » inhalational anesthetic e.g. Isoflurane Take-Home points - Status better outcome if sz stopped earlier Lorazepam - best 1st line Rx Fosphenytoin - surpasses Phenytoin for SE, and for any patient with altered mental status who would otherwise need IV Phenytoin - hopefully more available soon Propofol - advantages over barbiturates for resistant SE