Burns - Texas Tech University Health Sciences Center
advertisement

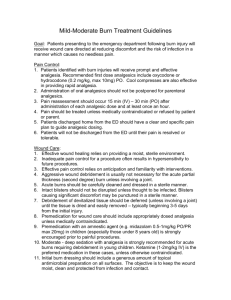
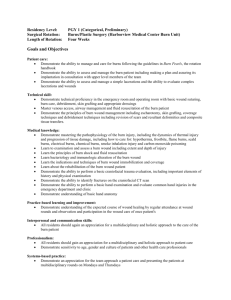
This PowerPoint file is a supplement to the video presentation. Some of the educational content of this program is not available solely through the PowerPoint file. Participants should use all materials to enhance the value of this continuing education program. EMS/Nursing 81212/ 39112 Burns: Part 2 Toni Galvan, MSN, RN, CCRN, CEN Charge Nurse II Medical Intensive Care Unit Covenant Health System Lubbock, Texas EMS/Nursing 81212/ 39112 Objectives 1. Identify risks to burn patients related to compartment syndromes. EMS/Nursing 81212/ 39112 Objectives 2. Recognize effective methods in wound care for burn patients. EMS/Nursing 81212/ 39112 Objectives 3. Recognize elements of a regimen for successful wound healing. Complications: Peripheral Ischemia rd Risk: usually 3 degree circumferential burns and electrical burns leading to compartment syndrome (edema and pressure in fascial compartment) Complications: Peripheral Ischemia Assess for: pain, pallor, pulselessness, paresthesia, paralysis, poikilothermia (6 Ps) Doppler pulses: palmar arch, finger webs Circumferential burn – checking pulses Treatment Compartment Syndrome Continue pulse check Elevate extremity to level of heart Consider escharotomy: cutting through eschar Escharotomy Locations Escharotomy Locations Also vertical cuts on lateral neck, avoiding great vessels and trachea What about pain? What about scars? Escharotomies improperly done→ 3rd degree burn in Caucasian child Inhalation Injury Inhale hot air, steam, smoke, carbon monoxide (CO) Above glottis: actual burn, compromise to airway Inhalation Injury Below glottis: toxic effects similar to acquired respiratory distress syndrome (ARDS) Inhalation Injury Suspect if: face and/or neck burns singed nose hairs flame burn in enclosed spaces carbonaceous sputum Inhalation Injury Suspect if: early edema of tongue burns of nasal or oral mucosa Inhalation Injury Early signs and symptoms hoarseness and drooling (#1) Inhalation Injury Early signs and symptoms altered ABGs (arterial blood gas), especially hemoglobin CO (HbCO) 2060% Inhalation Injury DO NOT use pulse oximetry (SpO2) to monitor O2 saturation Inhalation Injury Treatment: early intubation and ventilation with fractional inspired oxygen (FiO2) 1.0 and added pressure or high frequency ventilation (HFV) Wound Care Keep very clean: scrub Grafts only autograft, cultured epidermis, and isograft (identical twin) are permanent Wound Care Keep very clean: scrub Grafts others are temporary to encourage capillary neogenesis in wound bed and act as wound dressing Goals of Wound Care Close wound as soon as possible – preserves cosmetics (looks) and function Optimal closure – prevents infection Goals of Wound Care Early care of deep burns – encourages rapid granulation and preparation for grafting Medicate for pain prior to wound care Wound Assessment and Documentation Location Size, depth Color, texture, sensation Odor Wound Assessment and Documentation Exudate color, amount, quality Exposed bone, tendon, cartilage, subcutaneous tissue Wound Assessment and Documentation Surrounding tissue inflammation/infection Early Wound Care for Heat Burns Remove patient from site Remove clothing and jewelry, especially circumferential Early Wound Care for Heat Burns Cool wound with, ideally, cool sterile saline – use tap water or whatever else is available if necessary Early Wound Care for Heat Burns DO NOT apply topicals until after initial assessment and determination of minor/ moderate/major and depth of wounds Treatment for First Degree Keep clean: soap and tepid water Apply moisturizer such as ® Aquaphor , aloe vera gel Treatment for First Degree ® Use Tylenol for pain Key: prevention Treatment for Second Degree/Partial-thickness Débride blisters and loose (dead) skin Treatment for Second Degree/Partial-thickness Clean: scrub with surgical sponges (sterile) or very clean technique (clean washcloth, shower or clean washbasin, new mild soap) Treatment for Second Degree/Partial-thickness Dressings ® Biobrane for clean wounds without topical residues of any kind – replace every 2 to 3 days or as instructed Treatment for Second Degree/Partial-thickness Aquaphor®, if very shallow, for each cleaning Treatment for Second Degree/Partial-thickness Triple antibiotic ointment if inflammation NEVER use on cartilage cover with non-adherent dressing Topical Meds ® Aquaphor : water soluble moisturizer Aloe vera gel: herbal, water soluble moisturizer Topical Meds Triple antibiotic ointment: can be nephrotoxic if used for >20% TBSA [total body surface area (covered)] Topical Meds ® Sulfamylon (mafenide acetate) painful, can be nephrotoxic, cause metabolic acidosis Topical Meds ® Sulfamylon (mafenide acetate) used on deep burns, thick eschar, pseudomonas infection Topical Meds ® Silvadene (silver sulfadiazine) less painful and minimal systemic absorption softens eschar and retards bacterial growth Topical Meds ® Silvadene (silver sulfadiazine) can suppress white blood cells (WBCs) Nystatin: for yeast Topical Meds Furacin: used for resistant staph and strep infections Acticoat™ silver dressing antimicrobial keep moist with sterile water Topical Meds Furacin: used for resistant staph and strep infections Acticoat™ silver dressing wounds will be stained Topical Meds ® Aquacoat impregnated with Silvadene® and activated with sterile water sustained release Topical Meds Accuzyme™: dissolves eschar, dead tissue Bactroban®: effective against gram+ staph and strep Topical Meds Scarlet Red tincture of mercury used on donor sites and very shallow 2nd degree antimicrobial and stimulates granulation/ healing Topical Meds and Dressings Choice of topicals by type of wound and if infected Generally prescribed Topical Meds and Dressings Precise wound care instructions post-burn unit prescribed, taught to family or home health staff Questions: call BICU (burn intensive care unit) Grafts Allograft/homograft human cadaver used as temporary dressing to promote granulation Grafts Xenograft/heterograft pig skin used as temporary dressing to promote granulation Synthetic Grafts Biobrane®, SkinTemp™, Integra™, nylon, TransCyte®, XenoDerm Synthetic Grafts used as temporary dressing to promote healing or granulation also used on autograft donor sites Permanent Grafts Autograft self or cultured epidermis used for final repair Permanent Grafts Care pressure dressing for 3 days, undisturbed then, clean gently and cover with protective dressings until healed, then leave open to air Permanent Grafts Care observe closely for signs and symptoms of infection Graft Procedures Remove autograft with dermatome Apply as full-thickness or mesh Use full-thickness on face, hands, feet, genitalia unless lack of viable skin for grafts Meshed skin: stretches to cover more area and is used on trunk, limbs Mesh graft of hand Mesh graft with wound drain space Full-thickness graft of hand Cultured epithelial tissue after placement Post-graft Care Donor site care: Scarlet Red or Aquaphor® or other moisturizer and transparent dressings Care of Temporary Grafts Cadaver skin and pig skin change about every 3 days or if evidence of infection cover with pressure dressings often Care of Temporary Grafts Synthetic change every 3-14 days (manufacturer instructions) can be left open or covered Care of Temporary Grafts Synthetic most cannot be used on eschar, must débride first Support of Wound Healing ® Oxandrin promotes use of dietary protein anabolic steroid controlled drug Support of Wound Healing High-dose vitamins A and C: wound healing High-dose zinc: stress, wound healing General nutrition: highcalorie, high-protein diet Patient and Family Teaching Essential for recovery Properly done wound care hurts – patients and families have trouble scrubbing hard enough Patient and Family Teaching Absolute cleanliness essential First sign of infection: return to doctor Patient and Family Teaching Nutrition and ROM (range of motion) and general activity essential for recovery – no “couch potatoes” Patient and Family Teaching Use splints/pressure garments as prescribed – pressure garments need to be worn at all times for optimum effect Infection Leading cause of death in burns after first 72 hours Prevention: HANDWASHING Prevention: properly done wound care Signs and Symptoms of Infection Persistent true fever (lowgrade fever normal in burns) Signs and Symptoms of Infection Increasing wound exudate after 72 hours, especially pseudomonas or staph (early in healing, moderately thick, yellow exudate is expected) Signs and Symptoms of Infection Cellulitis of surrounding tissues: red, swollen, painful WBC changes Positive wound cultures Treatment of Infection Systemic antibiotics by culture results Appropriate topicals Treatment of Infection Often necessary to return to BICU for intravenous (IV) antibiotics and/or surgical débridement and regraft Expensive: best to prevent Special Situations Tar immediately cool with any liquid use petroleum jelly or mineral oil to remove continues to burn until removed Special Situations Friction burns (road rash): nd treat as superficial 2 degree Special Situations Eyelids, lips, and ears require special care ® no Neosporin on exposed cartilage ® use Neosporin on all others Special Situations Face: shave males daily Chemical burns: brush off dry chemicals immediately, remove clothing, shower or hose quickly Special Situations Chemical burns in eye: irrigate with tap water quickly, copiously Electrical burns: transport to burn unit for all Complication Keloids (scar hypertrophy): from lack of pressure during healing Complication Contractures Complication Contractures: from lack of physiologic positioning and lack of aggressive exercise therapy during healing Complication Myoglobinuria from electrical burns, large muscle burns large molecules damage renal tubules resulting in hematuria Complication Myoglobinuria can indicate rhabdomyolysis Electrical Burns Order current travels: nerves, blood vessels, muscle, bone Wound: entry and exit, invisible damage between Electrical Burns Complications: ventricular fibrillation, other dysrhythmias, respiratory tetany and arrest, falls, fractures Severity: length exposure, voltage, concomitant injuries Electrical Burns Treatment débride (often extensive) cardiac monitor treat dysrhythmias mechanical ventilator as needed Electrical Burns Entry wound Exit wound Chemical Burns Damage: strength, duration, volume, permeability, mode of action Most common: acids Chemical Burns Most troublesome: alkali because it adheres to tissue causing protein lysis and liquefaction Household chemicals: bleach and ammonia Chemical Burns Farm: organophosphates and other fertilizers and weed control chemicals Chemical Burn Initial Care Topical: (except sodium metal) remove agent and clothing, shower with tepid tap water Chemical Burn Initial Care Eyes: irrigate with tap water st (1 aid) or normal saline (do not use irrigation lenses) Chemical Burn Initial Care Inhalation (mustard gas, etc.): 100% O2 at high pressure/frequency Sodium metal explodes in air and H2O – remove surgically under oil Chemical burn: fell in vat of chemical Phases of Care Emergent: 24-72 hours Acute: days-months (until wounds closed) Rehabilitation: starts on admission/initial treatment and goes up to 2 years Immediate Care Priorities ABCs (airway, breathing, and circulation): intubate as needed Remove all clothing/jewelry Estimate size, depth Immediate Care Priorities Fluid resuscitation for burn shock Evaluate for late inhalation injury Immediate Care Priorities Peripheral circulation and escharotomy as needed Pain: morphine, incremental IV doses Wound care: débride, clean Immediate Care Priorities Tetanus history and treatment Continuing Care Wound care as discussed Keep clean Itch: lotion Continuing Care Pain over-the-counter, as Tylenol® or NSAID (nonsteroidal antiinflammatory drugs) or PO (oral) narcotics Continuing Care Pain take on schedule and as needed ROM, ambulation, exercise as appropriate Continuing Care Scars/keloid: use pressure garments, splints Sun protection healed burns always more sensitive avoid all sun 12-18 months Lifestyle Return to work when initial healing and energy level adequate – no sun exposure Nightmares and PTSD (posttraumatic stress disorder): treat – these are real Lifestyle Depression and fatigue part of healing some require treatment rest more talk about it family teaching/support Lifestyle Scars many are permanent body image disturbance some color change Rehabilitation Starts on admission/initial treatment Range of motion and activity Pressure garments and splints Rehabilitation Medical follow-up (burn clinic) Lifestyle adjustments Return to productivity How long to heal? Complete maturity: 1-3 years Some need further surgery to improve cosmetics during first year Initial closure: weeks to months for large deep burns; if infected, takes longer Other Complications of Burns Death Functional long-term disability Other Complications of Burns Financial and role stress patient family/significant others community Transport Contract with tertiary site Transport major and some moderate MD-MD and RN-RN contact as early as possible and update on dispatch Transport Choose method of transport: ground or air Stabilize for transport Stabilize for Transport Airway if in doubt, intubate always intubate anyone with possible inhalation injury Stabilize for Transport Fluids stable IV sites and initial fluid resuscitation started Foley catheter inserted Stabilize for Transport Wounds remove clothing and jewelry cover wounds loosely with dry, non-adherent dressings Stabilize for Transport Pain: narcotic coverage Family: instructions to find agency and NO SPEEDING Documentation for Transport Copy all lab/x-rays What was done for wounds Fluid resuscitation with times Next of kin/family location/contact Documentation for Transport Miscellaneous Summary Large burns are devastating for victim and family Most are preventable Mortality rate diminishing with proper early care Summary Long-term disability not necessary for most with proper care EMS/Nursing 81212/ 39112 Burns: Part 2 If you have any questions about the program you have just watched, you may call us at: (800) 424-4888 or fax (806) 743-2233. Direct your inquiries to Customer Service. Be sure to include the program number, title and speaker. EMS/Nursing 81212/ 39112 Release Date: 04/01/2012 The accreditation for this program can be found by signing in to www.ttuhsc.edu/health.edu EMS 81212 This continuing education activity is approved by the Continuing Education Coordinating Board for Emergency Medical Services for 1.5 advanced CEH. You have participated in a continuing education program that has received CECBEMS approval for continuing education credit. If you have any comments regarding the quality of this program and/or your satisfaction with it, please contact CECBEMS at: CECBEMS -12200 Ford Road, Suite 478 Dallas, TX 75234 Phone: 972-247-4442 lsibley@cecbems.com Nursing 39112 The Texas Tech University Health Sciences Center Continuing Nursing Education Program is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center's Commission on Accreditation. Provider approved by California Board of Registered Nursing, Provider #CEP11800, for the designated number of contact hours for each program. Provider approved by Florida Department of Health Board of Nursing, Provider #FBN2060. Provider approved by West Virginia Board of Examiners for Registered Professional Nurses, Provider #WV1998-0262RN. Iowa Board of Nursing approved provider #325. Accepted by the North Carolina Board of Nursing. Reminder to all PARTICIPANTS, certificates should be retained for a period of four (4) years. Health.edu reports Florida Continuing Education (Contact Hours) to CE Broker. This activity provides 1.5 contact hours. Nursing 39112 This activity is presented for educational purposes only. Participants are expected to utilize their own expertise and judgment while engaged in the practice of nursing. The content of the presentations is provided solely by presenters who have been selected for presentations because of recognized expertise in their field. Nursing 39112 DISCLOSURE TO PARTICIPANTS Requirements of successful course completion: •Complete the program via video presentation, PowerPoint slides, audio presentation, and/or manuscript. •Complete the course evaluation. •Complete the posttest with a score of 80% or greater. •Complete the time utilized in course completion including the posttest. Nursing 39112 Conflicts of Interest: Toni Galvan, MSN, RN, CCRN, CEN has disclosed that no financial interests, arrangements or affiliations with organization/s that could be perceived as a real or apparent conflict of interest in employment, leadership positions, research funding, paid consultants or member of an advisory board or review panel, speaker’s bureau, major stock or investment holder, or other remuneration. Commercial Support: There is no commercial support and/or relevant financial relationships related to this educational activity. Commercial support is defined as financial (or in-kind) contributions given by a commercial interest, which is used to pay all or part of the costs of a CNE activity. Relevant financial relationships are defined as financial relationships of any amount, occurring within the past 12 months, including financial relationships of a spouse or life partner that could create a conflict of interest. Nursing 39112 Non-endorsement of Products: Toni Galvan, MSN, RN, CCRN, CEN has disclosed that no significant relationships with commercial companies whose products or services are discussed in educational presentations. For speakers, significant relationships include receiving from a commercial company research grants, consultancies, honoraria and travel, or other benefits or having a self-managed equity interest in a company. Disclosure of a relationship is not intended to suggest or condone bias in any presentation, but is made to provide participants with information that might be of potential importance to their evaluation of a presentation. Off-label Use: Toni Galvan, MSN, RN, CCRN, CEN has disclosed that no products with off-label or unapproved uses are discussed within this activity. Nursing 39112 Individual programs are provided for a two (2) year period. Participants should check with their site coordinator, sign in to Health.edu’s internet site, http://www.ttuhsc.edu/health.edu or call Education Services at 1-800-424-4888 for information on the date through which this learning activity is provided. For questions or comments regarding accreditation, please call Education Services at 1-800-424-4888.To speak to a Customer Service representative, please call 1-800-424-4888. Institutional refund is available to subscribing organizations according to Health.edu’s tuition refund policy. See your site coordinator to view this program.