Nursing Assistant - Safe Environment
advertisement

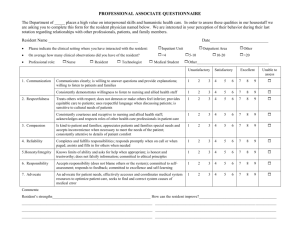
Nursing Assistant Safe Environment Role of CNA in Emergency, Disaster, & Fire Situations Be prepared – Know emergency codes (STAT) – Fire & disaster plans – Location of fire exits/extinguishers Remain calm Call for assistance, don’t act beyond level of knowledge Move residents in immediate danger Remain with resident Role (cont) Keep resident comfortable & calm Evacuate resident to safety according to plans Send family or visitors to the facility designated area Ways to help others remain calm Stay calm yourself, use a calm voice Project confidence Know & use facility emergency plans Stay with resident, keep them comfortable & quiet Move or direct families to the designated areas or safe places Common Emergency Codes Types – Fire – code red or doctor red – Cardiac arrest – code blue, code 99 – Resident safety issue – manpower or a special alarm sound – Disaster code – disaster level 3 Emergency Call System Telephone numbers – Numbers within the facility – EMS – licensed nurse dials 911 Remain call, don’t shout fire or arrest STAT – respond at once General rules for providing a safe environment Use good body mechanics Know policy & procedures regarding safety laws on use of equipment & handling hazardous materials (OSHA & MSDS) What are hazardous materials? Wipe up spills immediately, identify wet floors with signs Walk, never run in halls, watch at intersections Tag & report broken equipment General rules (cont) Report unsafe conditions Use 3-pronged plugs on electrical equipment Refuse to do any task you do not know how to do Watch linens & garbage for safety hazards (sharps) Report if sharps container is over half full In case of personal injury Report injury immediately to supervisor Fill out incident or accident report Seek medical help as necessary Resident safety is an important quality assurance issue General measures to provide safe environment Check wrist bands or name tags before performing any task Use side rails when appropriate Have resident use handrails or assistive devices when unstable Non-skid footwear when ambulatory Call signal within reach at all times & resident aware of how to use Lock wheels on bed/wheelchair/gurney Answer call lights promptly General measures (cont) Use night lights to help ensure good lighting & reduce obstacle hazards Keep be in lowest position except when working with the resident Check bed/chair alarms ensuring working condition 2 top safety issues FALLS (70% of all accidents) – Proper position in bed/wheelchair & readjust every 2 hours – Soft protective devices as ordered – SIDE RAILS – watch for arms/legs/tubing. Make sure they are locked in up position – Brakes on while transferring resident – Comfort items (water, call light, urinal) within easy reach Safety Issues Falls (cont) – Answer call lights promptly – Areas should have good lighting & be free of clutter – Foot latches on beds & foot supports of w/c out of way to prevent tripping or hitting legs – Wipe up spills promptly – Meet needs quickly (water, elimination) – Use appropriate assistive devices as directed by licensed nurse – Be aware of resident’s location at all times – More likely to occur when attention is elsewhere Safety issues Assistive devices used to reduce falls & maintain safe mobility – Assessed for need by licensed nurse, PT, or rehab team (imput from CNA) – Types of devices • Cane – single tip, tri tip, quad cane • Use on strong side • Check rubber tip & appropriate height Safety issues Assistive devices (cont) – Walker – provides stability & support • Pick-up, front-wheeled, four-wheeled • Check rubber tips & height • Give instruction on correct use – Wheelchair – provides mobility • Different types • Removable arm rests & foot rests • Brake locks on when transferring resident Safety issues BURNS – 2nd most common hazard – Types & causes • • • • Steam or water burns – bathing, hot drinks Flames – smoking Chemical – cleaners like peri-wash Thermal – heating pads, sunburn – Prevention of burns – best approach • • • • • • Check water temp, report if too hot Monitor smoking, hot drinks, & risk for spills Know how to use equipment like K-pads & hot packs Protect from sunburn with hat, sunscreen, brief exposure Know policy & procedure of fire response Follow directions on use of chemical cleaners Safety issues Intervention of burns (initial first aid) – First degree burns – • Ice & cold water only for discomfort – Never use butter, shortening, etc – Causes burn to be worse – Deeper or large burns – immediate attention • Notify licensed nurse immediately • Describe cause of burn if possible Who is at high risk for accidents? Fire Major causes – – – – – – Smoking is number one cause Sparks from faulty electrical equipment Heating systems Spontaneous ignition Improper disposal of trash 3 things needed to start a fire • Fuel • Flame • Oxygen Fire can cause both burns & suffocation Fire prevention Electrical – Report frayed electrical cords, smoke, or burning smells – Don’t use too many electrical devices on one wall socket – Use 3-pronged GROUNDED plugs Fire prevention Smoking – Empty waste paper into proper containers – Supervise residents who smoke if their condition is confusion, lethargic, or weak – Be sure materials in ashtrays are completely extinguished before throwing away. Always use ashtrays when smoking – Smoking allowed in designated areas only RACE – for fire emergencies R – Remove resident from fire & close the room door A – Activate the fire alarm system C – Contain the fire E – Extinguish if possible PASS for fire emergencies P – Pull extinguisher pin A – Aim S – Squeeze S – Sweep low Fire emergencies Make sure that residents are not placed by fire emergency doors – Swing shut automatically Know & follow facility’s specific policy & procedure Safety rules for Oxygen use Oxygen therapy – – – – – – Abbreviated as O2 Colorless, odorless, tasteless Essential for respiration Some residents need supplemental O2 Supplied in portable tanks or through wall outlets Increases the risk of fire because it supports combustion & is one of the 3 elements needed for fire Safety precautions for oxygen “No smoking, Oxygen in use” sign on door & over bed Smoking is NEVER allowed near oxygen by ANYONE! Keep tubing open & free of kinks Check electrical equipment use (electric razors, fans, radios) No flammable liquids (alcohol, nail polish remover, petroleum based – vaseline, chapstick) Watch for static when combing hair, using WOOL blankets, or nylon in clothing Types of oxygen equipment Green metal portable tanks – Under pressure & must be handled carefully to prevent dropping & possible explosion when in storage – Must be secured to wall – On movable stands & strapped in place Wall outlets – use wall mount flow meter & plastic tubing Types of oxygen equipment Portable tanks – Large ones covered with plastic casing & small ones that resident can carry or hang on assistive devices – Must be kept upright & not dropped Equipment used to deliver oxygen – Nasal cannula – Face mask – concentrators Nursing care for oxygen Dr’s order needed (considered med) Make sure resident wears mask or cannula – If oxygen needs to be turned off, MUST have an order – When not in use, needs to be turned off (very expensive & a fire hazard) Follow facility procedures for filling oxygen tanks, turning tanks off & on, set-up of oxygen Oxygen is very drying – Check nose & cleanse – Maintain water level in humidifier to reduce dryness Nursing care for oxygen Check for redness over ears & on face where tubing rests – report if present May turn tank on & off, but may NOT adjust oxygen to a lighter flow (med administration, not in your scope of practice) Postural supports Used to prevent resident from harming self or others Used to prevent – Falling out of bed/chair – Crawling over side rails or end of bed – Interfering with therapy by removing tubing or dressings – Hurting themselves or others Postural supports Types – Soft protective device – serves as a reminder to resident of safety issues (waist device) – Postural supports – devices to help to keep the resident in the correct postural position when up in a chair (posey vest) – Restraints – control behavior & are used only in extreme measures like limb devices. Side rails can be considered a restraint Infringe on resident’s rights to freedom of movement & may be considered “false imprisonment” if used inappropriately Alternative to device use Place resident where there is constant supervision Make sure comfort needs are met (water, toilet, reposition) so that there is a reduced risk of attempting to do unassisted & agitation is reduced Devices are used as a last resort & NEVER for convenience or as a punishment Types of protective devices Vest or jacket device – has opening in front, watch for choking & cutting into resident Wrist or ankle device – soft limb device restricts limb movement Hand mitt device – prevents scratching & removal of tubes & dressings Waist device – soft cloth or metal bars that remind the resident that they need assistance before walking or standing to reduce falls Pelvic support – keeps resident from sliding down in w/c, wide in front/narrow in back. Watch genitalia Regulations regarding postural supports Approach in calm manner to reduce anxiety & agitation during application Explain in non-threatening manner – “safety” & “soft protective” Use only on resident in bed or chair with wheels in case of emergency Place resident in good body alignment Pad bony prominences Regulations Use quick release bow-tie knots to secure device to bed frame or chair so that you can untie quickly in an emergency Tie securely, but allow two-finger slack for movement between support & skin Check circulation, sensation, & movement (CMS) every two hours Tie support to bed frame NOT side rails Remove support & reposition every 2 hours, do ROM to joint Regulations Offer fluids, bedpan, urinal on a frequent, regular basis. Have call light within reach Apply vest device with open area of vest in FRONT to prevent choking Document type of device, reason for applying, time on & off, CMS, effectiveness, & nursing care required Legal & Psychological implications of postural devices Legal – – Must have a dr’s order stating reason for use, type of device, & for how long – Must have informed consent – Cannot restrain unnecessarily or for staff convenience – Unnecessary restraint can equal false imprisonment Implications Psychological – Explain to resident & family reason for protective devices – Resident may struggle against devices – reassure & support resident & family Bioterrorism Possible terrorist acts – Biological • Bacteria or viruses • Toxins – Chemical – Explosions – Nuclear blast – Radiation Homeland security advisory system Green – low condition Blue – guarded condition Yellow – elevated condition Orange – high condition Red – severe condition