Barriers to Completing Advance Directives
advertisement
Advanced
Directives:
{
Le
ve
l
Si
xt
h
O
utl
in
e
Le
ve
l
Se
ve
nt
h
O
utl
in
e
Le
ve
l
Ei
gh
th
Thinking and Talking About the Hard Stuff ~
In 1900, average longevity in US was 49.2 years
In 2010, was 78 years.
Initial gain made through advent of sanitation,
childhood immunizations.
Since 1960, medical advances allowed lives to
be prolonged. Procedures/surgeries, antibiotics,
chemotherapy, heart/HTN medications, etc.
People live longer, die
differently
Death causes 1900
Click to edit the
outline text format
Second Outline
Level
Third Outline
Level
Infectious diarrhea
pneumonia
Fourth
Outline
Level
Fifth
Outline
Level
Sixth
Outline
Level
Sevent
h
31% were relatively quick
contagious dz, 14% lifestyle dz
Death causes 2004
56% are lingering deaths
2004
No contagious disease causes
in the top 3 causes
56% of top 3 causes mostly
lifestyle diseases
Sometimes cancer just happens
Often lifestyle encourages development
Lung, bladder, kidney, stomach, esophageal,
oral, lymphoma---smoking
Breast ---overweight, lack of exercise, high fat
diet, ETOH, HRT
Pancreas, stomach ---alcohol
Colon---low fiber, high fat diet
Is cancer a “lifestyle” disease?
Advances in technology:
•
Ventilators
Gastrostomy tubes
Dialysis
Implantable Cardiac Defibrillators
Ventricular Assist Devices
•
•
•
•
Enter….the machines
“The Dwindles“
The Dwindles --- a cascade of
events
Desk-exercise not a priority
Spent life watching football instead of playing football
Smoke, poor diet, become overweight or obese
Knees develop arthritis, ruptured back disk from wt
Now can’t exercise if want to
Become DM, HTN, COPD
Stroke –paralyzed on one side. Can barely walk. Need
spouse’s help
Too big to care for. Strain on family
Stratolounger or bed becomes your world
Everyone born has a “right to life,”
then what about a “right to die?”
Should any law upholding a person’s
right to life should inherently include
their right to die?
DO WE HAVE THE
“RIGHT TO DIE?”
Court Cases-it’s what started it all.
Karen Ann Quinlan -1975
When 21, overdose of ETOH and 2 Rx drugs
Stopped breathing >15 min
Persistent vegetative state, on ventilator
Parents wanted removal , hospital fought
Protracted court proceedings, tube removed
Lived for almost another decade
Stopping ventilators
Two significant outcomes of her case
development of formal ethics committees in
hospitals, nursing homes and hospices
and the development of advance health
directives
Nancy Cruzen-1990
After an automobile
accident left her in
a persistent vegetative
state, her family
petitioned in courts for
three years, as far as
the U.S. Supreme
Court (Cruzan v.
Director, Missouri
Department of Health), to
have her feeding
{
“Right to die”
Le
ve
l
Si
xt
h
O
utl
in
e
Le
ve
l
Se
ve
nt
h
O
utl
in
e
Le
ve
l
Ei
gh
th
The family's request was ultimately granted by
providing additional evidence. On December
15, 1990, the tube was removed and she died 12
days later.
The courts recognized for the first time a
constitutional right to refuse treatment in
extraordinary circumstances.
Stopping feeding tubes
The Cruzan decision spurred considerable
interest in "living wills" which clearly express
an individuals desire to discontinue treatment
or feeding in specified circumstances.
The Birth of the
Right to Die
Terry Schiavo-2005
Terri Schiavo collapsed in her home in
full cardiac arrest on February 25, 1990. She
suffered massive brain damage due to lack of
oxygen and eventually diagnosed as being in a
persistent vegetative state.
Normal CT scan---Terri’s CT scan
Legal battle between her husband and the
parents of Terri Schiavo that lasted from 1998 to
2005.
Lack of a living will caused a protracted series
of appeals to determine what Terri’s wishes
would have been re. life-prolonging
procedures.
Legal Battles Extraordinaire
Keeping Terri alive became a focal point for the
Right to Life movement
MULTIPLE appeals, motions, hearings, etc.
Florida legislature
Florida governor Bush
Florida and U.S. Supreme Court
Congressional Republicans
President Bush
Send in the ____
At issue was whether the husband had the
right to make decisions to . The highly
publicized and prolonged series of legal
challenges presented by the parents and by
state and federal legislative intervention
effected in total a seven-year delay before life
support finally was terminated.
What a mess!
the court finally found that Terri had made
reliable oral declarations that she would have
wanted the feeding tube removed, allowing her
husband’s decision to terminate life support
prevail.
The Patient Self-Determination Act requires
that healthcare institutions receiving Medicare
or Medicaid reimbursement provide patients
with written information about their legal
rights to participate in medical decisions by
completing an advance directive.
An important goal of the Patient SelfDetermination Act is to encourage patients to
indicate their preferences for end-of-life care
before the need arises, thus allowing healthcare
providers to honor individual choices, improve
the quality of dying and reduce stress for
families and caregivers
Patient self determination
act of 1991
Self-determination is derived from the
principle that an adult has the right to decide
what happens to his or her body. An advance
directive documents the wish of a person to
give directions about future medical care or to
designate another person to make medical
decisions if he or she loses decision-making
capacity.
The law also mandates that healthcare
providers document the presence or absence of
an advance directive in the patient’s medical
record.
What the Law
A patient’s right to make decisions in an
Intends
advance directive is protected by federal and
state law.
Who has Advanced
Directives?
Only 14% of Americans have a written advance directive
expressing their personal wishes for end-of-life care.
This low percentage has significant implications for the aging
U.S. population, as well as for younger adults who often don’t
think about the need for an advance directive until they are
confronted with a life-threatening terminal medical diagnosis.
Living wills and other advance directives aren't just for older
adults. Unexpected end-of-life situations can happen at any age,
so it's important for all adults to have advance directives.
Answer: everyone over age >=18.
Younger adults do not consider the need for
AD,
not considering death imminent. This age
group known for risky behavior. Yet, main
causes of death can lead to brain damage/death
and an inability to make AD decisions.
1.
Leading causes of death for ages 15-25:
Accidents, “unintentional injury”, MVA
Homicide
suicide
Who needs AD?
2.
3.
People over age 65 whose heart
stops outside the hospital setting
have about a 2 percent chance of
survival. Of those who survive,
half will end up permanently in a
nursing home. Only 1 percent will
return home .
Fully 50 percent of Medicare
funds are exhausted caring for
patients in the last 6 months of
life.
The NUMBERS
Healthy, robust 86 year old. Walked 6 miles a
day, played tennis 3x/wk
Hit by a car while jay walking.
Initial injuries-femur (thigh) and ribs fracture,
closed head injury, punctured lung.
On ventilator. Had a stroke, went into kidney
and liver failure. Developed pneumonia and
placed on antibiotics. Had a reaction to
antibiotics, turned bright red, and skin began to
slough. Doctors considered dialysis.
NO MPOA.
Family could not agree to appropriate
interventions.
3 months; much agony, and $1,000,000 later, he
finally died.
My friend’s father
ACUTE- sudden events that require immediate
care decisions
Massive stroke
Heart attack with/without arrest, heart failure
MVA
COPD exacerbation/pneumonia
Sepsis (massive infection)
Traumatic brain injury
Defining events I
CHRONIC---no sudden event, no clear line of
delineation as when to stop interventions
Dementia/Alzheimer’s Disease
“global geriatric decline/debility”—weight loss,
falls, frailty, loss of ability to performs
Activities of Daily Living (ADLs) “the
dwindles”
Cancer, neurologic diseases, autoimmune
diseases
Defining
II
Chronicevents
CHF, COPD, CAD
A vegetative state is a rare condition, caused
by brain damage, in which a person comes
out of a coma and is fully awake but they
have no sense of awareness.
14,000 people per year
Vegetative states:
let’s add to the confusion
a traumatic brain injury – caused by a severe
head injury such as that sustained during a car
accident or a fall from a great distance
non-traumatic brain injury – where the injury
to the brain is caused by a health condition
such as a stroke or Alzheimer's disease
Causes
40 % diagnosed with Minimally Conscious
State.
there is a condition called "locked-in
syndrome" where a person is fully aware but is
unable to move any of their muscles, so they
are unable to move or speak.
Aphasia, spasticity, blind, deaf, epileptic,
paralyzed, amnesic
Unlike persistent vegetative state, patients with
MCS have partial preservation of conscious
awareness. Squeeze hands, follow objects on
command. Consciousness often fluctuates.
Rare, but occasionally awaken (to some
degree).
Vegetative v.s. MCS
In a young person under the age of 20 who
experiences traumatic brain damage, the
chances of making a recovery are around 1 in 5.
A person over the age of 40, who is an
persistent vegetative state due to a nontraumatic brain damage, has an extremely
small chance of making a recovery.
People who do make a recovery are often likely
to have life-long physical and mental
disabilities resulting from the damage to their
brain.
“Recovery?”
Both conditions require a feeding tube.
If you were in a MCS,
what would you want?
How important to you is being independent
and self-sufficient?
What would make your life not worth living?
Would you want treatment to extend life in any
situation?
Would you want treatment only if a cure is
possible?
Do you have a goal in mind that influences
your decision about extending your life?
(wedding, graduation).
Would you want palliative care or hospice to
ease pain and discomfort if you were
terminally ill?
What treatments would you
want?
{
Resuscitation
Resuscitation.
Click to editRestarts
the
the
heart when
it has
outline
text format
stopped beating
Second
Outline
(cardiac
death).
Determine
Levelif and when
you would want to be
Third
resuscitated
by
Outline
cardiopulmonary
Level
resuscitation
(CPR) or
by a device that
Fourth
delivers an electric
Outline
shock to stimulate
the
Level
heart.
Fifth
Can lead to cardiac
assist devices (balloon
Outlin
pump) and
e
{
Interventions I
Fifth
Outlin
e Level
Ventilators
Sixth
Outlin
Mechanical
Click to edit the
e Level
ventilation.
Takes
over
outline text
format
your breathing ifSevent
you're
Second
Outline
h
unable
to do so.
Consider
if, when
and
Outlin
Level
for how long you
e Level
Third
wouldwant
tobe
Eighth
Outline
placed on a mechanical
Outlin
Level e Level
ventilator.
Fourth
Ninth Outline
LevelClickOutline
to edit
Master textLevel
styles
Fifth
Outlin
e
{
Nutrition/hydration
Nutritional
andthe
Click to edit
hydration
outline text format
assistance. Supplies the
Second
Outline
body
with nutrients
and fluids
Level
intravenously or via a
Third
tube in the
stomach.
Decide if,Outline
when and for
how longLevel
you would
want to be fed in this
Fourth
manner.
Outline
IV fluids-basic
hydration Level
Fifth
“TPN”-IV protein,
carbs, fats, fluidsOutlin
e
Gastrostomy tube-
{
Interventions II
Fifth
Outlin
e Level
Dialysis
Sixth
Outlin
Dialysis.
Click toRemoves
edit the
eblood
Level
waste
fromtext
your
outline
format
Sevent
and manages fluid
Second
Outline
h
levels
if your kidneys
no longer
Outlin
Levelfunction.
Determine if, when
and
e Level
long
Third
for how
you
Eighth
Outline
would want to receive
Outlin
Level e Level
this treatment.
Treatments 3x/wk for 4 Fourth
Ninth Outline
6 hrs
LevelClickOutline
to edit
Master textLevel
styles
Fifth
Outlin
e
Pericardial tap
Paracentisis
Thorocentesis
Surgery
? comfort versus treatment
Interventions III
Emergency care---do you wish to be
hospitalized for further interventions?
Antibiotics -– do you wish to be treated for a
pneumonia or sepsis (blood poisoning)?
Do you just wish to remain comfortable and in
your own home in your last days?
Is hospice or home-based Palliative Care a
better choice ?
Interventions IV
Your most
important asset
is a trusted MD
who can
provide you
with realistic
choices/outcom
e/expectations
MD role
Click to edit the
outline text format
Second Outline
Level
Third Outline
Level
Fourth
Outline
Level
Fifth
Outline
Level
Sixth
Outline
Level
Sevent
h
Can be treated, but not cured
Will get worse over time
Get pneumonia a lot
Repeat hospitalizations
Wearing oxygen
Debilitating, reducing quality of life
What’s it like to be intubated, air hungry?
Example: COPD
What are your
thoughts about dying?
Do you want to avoid
pain at all costs or do
you want to be
awake/alert?
What kind of quality of
life is acceptable?
What are your goals?
Wedding/graduation?
Click to edit the
outline text format
Second Outline
Level
Third Outline
Level
What are your goals?
Fourth
Outline
Level
Fifth
Outline
Level
Sixth
Outline
Level
Sevent
h
Let’s start with choosing
an MPOA.
First, what exactly DO
you want?
Medical or health care power of
attorney (MPOA). The medical
POA is a legal document that
designates an individual —
referred to as your health care
agent or proxy — to make
medical decisions for you in the
event that you're unable to do
so.
It is different from a power of
attorney authorizing someone to
make financial transactions for
you.
{
Le
ve
l
Si
xt
h
O
utl
in
e
Le
ve
l
Se
ve
nt
h
O
utl
in
e
Le
ve
l
Ei
gh
th
Medical power of attorney
(MPOA) aka “Healthcare Proxy”
Trust is the most important
element in choosing an MPOA .
Feel free to say what you want
and how you feel about End of
Life issues.
Prefer a committed, able MPOA
who knows what it is to be an
agent.
{
It’s not about what the MPOA
wants.
MPOA—your most
important decision
Le
ve
l
Si
xt
h
O
utl
in
e
Le
ve
l
Se
ve
nt
h
O
utl
in
e
Le
ve
l
Ei
gh
th
Choosing a person
to act as your
health care agent is
possibly the most
important part of
Choosing
MPOA You
youran
planning.
need to trust that
Your health care agent doesn't
necessarily have to be a family
member. You may want your
health care decision maker to be
different from the person you
choose to handle your financial
matters. It may be helpful, but
it's not necessary, if the person
lives in the same city or state as
you do.
{
Choosing
an
MPOA
Share your wishes with your
family.
Le
ve
l
Si
xt
h
O
utl
in
e
Le
ve
l
Se
ve
nt
h
O
utl
in
e
Le
ve
l
Ei
gh
th
to edit the
Who is an incapacitatedClick
adult?
outline text format
An adult “who is unable to effectively
Second Outline
receive or evaluate information
or both
Level
or make or communicate decisions to
Third Outline
such an extent that the individual
Level lacks
the ability to satisfy essential
Fourth
requirements for physical health,Outline
safety,
Level
or self-care, even with appropriate
and
reasonably available technological Fifth
Outline
assistance.
Level
Sixth
Who is an incapacitated adult?
Outline
Level
Sevent
h
Group of “interested
parties” get together and
choose one of the group to
be a Proxy Decision
Maker.
Medical Healthcare Proxy
form :
Click to edit the
outline text format
Second Outline
Level
Third Outline
Level
www.senioranswers.org
Uh-Oh! No MPOA!
Fourth
Outline
Level
Fifth
Outline
Level
Sixth
Outline
Level
Sevent
h
DNR
Do not resuscitate (DNR) order. This is a
request to not have cardiopulmonary
resuscitation (CPR) if your heart stops or if you
stop breathing. Advance directives do not have
to include a DNR order, and you don't have to
have an advance directive to have a DNR order.
Your doctor can put a DNR order in your
medical chart
It is a legal, binding physician order. Does not
expire.
File of Life or envelope
on your fridge
ID bracelet or necklace
Documentation on
your person?
Tattoo?
Click to edit the
outline text format
Second Outline
Level
Third Outline
Level
Notifying your DNR
status
Fourth
Outline
Level
Fifth
Outline
Level
Sixth
Outline
Level
Sevent
h
In hospital setting-is
honored as
documentation readily
available and can ID pt.
Validity of DNR and
identity of person need
to be confirmed ~any
?~CPR
Click to edit the
outline text format
Second Outline
Level
The reality of DNR
Third Outline
Level
Fourth
Outline
Level
Fifth
Outline
Level
Sixth
Outline
Level
Sevent
h
DNR
Advantages:
At home –paramedics often follow if
documentation readily available
Deficits:
Specific only to resuscitation efforts
In the field---rarely gets followed.
Living will. This written, legal document spells
out the types of medical treatments and lifesustaining measures you want and don't want,
such as mechanical breathing (respiration and
ventilation), tube feeding or resuscitation in the
event you are incapacitated.
Not a physician order, rather a directive.
A living will needs an MPOA to enact your
wishes
Living Wills
Advantages:
Short and sweet
Gives specific time parameters
Can be strictly interpreted but is mostly a guide
for MPOA
Deficits:
Not very detailed
No DNR
Almost never happens—MPOA steps in
Living Wills
Wish 1: The Person I Want to Make Care
Decisions for Me When I Can't
This section is an assignment of a health care agent
(also called proxy, surrogate, representative
or health care power of attorney). This person
makes medical decisions on your behalf if you are
unable to speak for yourself.
Wish 2: The Kind of Medical Treatment I Want
or Don't Want
This section is a living will—a definition of what life
support treatment means to you, and when you
would and would not want it.
5 wishes
Wish 3: How Comfortable I Want to Be
Wish 4: How I Want People to Treat Me
This section speaks to personal matters, such as
whether you would like to be at home, whether
you would like someone to pray at your
bedside, among others.
Wish 5: What I Want My Loved Ones to Know
This section deals with matters of forgiveness,
how you wish to be remembered and final
wishes regarding funeral or memorial plans.
5 Wishes
Advantages:
Comprehensive
Contains place for MPOA designation
Deficits
A bit long
As with Living Will—guide for MPOA
$5.00 ---agingwithdignity.org
5 Wishes
What do you want to know about your
condition ?
Strict adherence or interpretation?
Where to die?
Quality of life?
Treatment options
Spirituality
Organ donation
Body treatment after death
My Healthcare Decisions
Advantages:
Can personalize and add narrative
Comprehensive
Asks smart questions
Deficits
Still need to assign an MPOA separately
Does not contain a DNR
My Healthcare Decisions
Does not need an MPOA consult and to
enact.
It is a legal, binding physician order.
Covers resuscitation status
Medical interventions such as full,
limited, and comfort measures
Antibiotics
IV therapy
Tube feeding
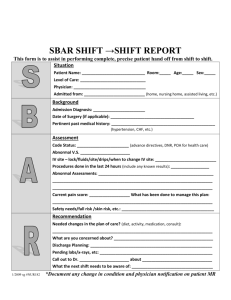
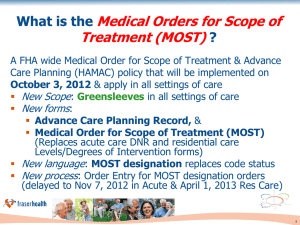
MOST FORM
Basically 4 parts
DNR
Level of medical interventions –level of airway
management
Antibiotics
Artificial nutrition
The MOST form
Advantages:
MD order
Comfort measures never optional
More comprehensive than DNR
Deficits:
Not flexible
MOST
All
Advanced
directives
documents
can be
changed or
rescinded at
any time.
Click to edit the
outline text format
Second Outline
Level
Change your mind?
Third Outline
Level
Fourth
Outline
Level
Fifth
Outline
Level
Sixth
Outline
Level
Sevent
h
Advanced Directives Documents
DNR
MD order/legally binding
Living Will
5 Wishes
Heathcare Decisions MOST
x
x
At discretion of MPOA
x
x
includes MPOA doc
x
x
need bracelet?
x
copy is valid?
x
x
x
x
x
x
x
Do you need a
A. DNR
B. Living Will
C. 5 wishes
D. MPOA
E. MOST
Multiple
F. All choice
of the questions
above ?
Most important—MPOA you trust!
Do you want something definitive –
DNR/MOST? (no MPOA needed)
Do you want resuscitation then decision by
your MPOA?
Most EOL decisions will be made
by your MPOA
What do you need?
Your MPOA chooses not to follow your wishes
Disagreements within family and between the
MPOA (MPOA has final decision)
The 23 year old who sees his grandfather die on
a ventilator and acts impulsively in completing
a DNR or MOST
Issues that might come up
Healthcare Affordability Act now allows for
one free visit with your primary care
physician to discuss AD.
Once you've filled out the forms, give copies
to your doctor, the person you've chosen as
your health care agent and your family
members. Keep another copy in a safe but
accessible place. You might also want to
keep a card in your wallet that says you
have a living will and where it can be found.
Talking with your doctor
Barriers to Completing Advance Directives
•Patient and provider reluctance
•Time constraints
•Assumptions about treatment preferences
•Denial and procrastination
•Unrealistic expectations
•Delaying until a crisis
•Discomfort with palliative care planning
•Lack of documentation of medical orders
•Cultural and health system barriers
•Lack of knowledge about the Patient Self-Determination Act and advance
directives among community members
Source: Butterworth AM. Reality check: 10 barriers to advance planning. Nurs
Pract. 2003;28(5):42-43
Barriers
1.Even when patients have advance directives,
they are often vague, incomplete, disregarded
by family members or unacknowledged by
caregivers.
2.When family members can’t agree on what
should be done.
3. Hospitals and physicians often pursue the
most aggressive treatment plan possible, even
when the patient is close to death.
4. Deciding to curtail treatment in critical care
settings poses unique problems.
5. Many patients and their families have had
little or no experience with critical care before
they face end-of-life care choices.
6. It may be difficult to convince some families
that the aim of withholding or withdrawing
treatment is to alleviate suffering. “Intervention
at all costs.”
Other obstacles
Through this type of advance directive, an
individual executes legal documents that
provide the power of attorney to others in the
case of an incapacitating medical condition.
The durable power of attorney allows an
individual to make bank transactions, sign
social security checks, apply for disability, or
simply write checks to pay the utility bill while
an individual is medically incapacitated.
Durable Power of
Attorney (DPOA)
A guardian is a person or persons appointed by
a court to assist with the personal affairs and
make decisions on behalf of a minor or an adult
who is incapacitated. A person under a
guardianship is called a ward.
Court ordered
A word about
Guardianship
My patient, Delores
No Advanced Directives for medical/financial
Small house in Longmont
Filthy—never cleaned, fridge science
experiment
Dogs --vet
Significant dementia
Drove –Kansas, Wyoming, Boulder
Gero-psych unit
Placement
Guardianship by son
A conservator is a person, or persons, appointed
by a court to manage finances and property for
an adult who is incapacitated, and whose assets
may be wasted or dissipated unless
management is provided. (Usually there is
dementia or emotional instability).
•
Charities
Scams
Unscrupulous family members
Poor buying choices
•
•
•
A word about
Conservatorship
Different than MPOA as this is after the fact and
is court-ordered.
More about
conservatorship
Finances and Welfare
POA
voluntary
welfare of person
Conservatorship
x
x
x
court ordered
financial
Guardianship
x
x
x
You can also specify in your advance directives any wishes
you have about donating your organs, eyes and tissues for
transplantation-sign up online in the Colorado Organ and
Tissue Donor Registry
at www.ColoradoDonorRegistry.org
Indicate your wishes on your driver’s license or
state ID when you apply for or renew it.
Let your MPOA and family know your wishes. Desire to
donate needs to be documented prior to death.
Organ donation
. If you wish to donate your body for scientific
study:
Colorado State Anatomical Board
P.O. Box 6511, MS 8501
Aurora, CO 80045
Phone:
303-724-2410
URL: http://www.ucdenver.edu/academics/coll
eges/medicalschool/departments/CellDevelop
mentalBiology/anatomicalboard/Aboutus/Page
s/default.aspx
WHOLE BODY
DONATION
Website Resources
“Put It in Writing” — uses a Q and A format to
help patients learn about types of advance
directives and their
importance. www.putitinwriting.org
Partnership for Caring — provides information
about end-of-life options and how to document
them. www.partnershipforcaring.org
Aging with Dignity — publishes Five Wishes, a
tool that helps patients consider their medical,
personal, emotional and spiritual needs in
planning end-of-life
choices.www.agingwithdignity.org/5wishes.ht
ml
MOST form –State of Coloradohttp://www.coloradoadvancedirectives.com/M
OST_Form_08.11.10.pdf
Website Resources
Click to edit the
outline text format
Second Outline
Level
Third Outline
Level
Fourth
Outline
Level
Fifth
Outline
Level
Sixth
Outline
Level
Sevent
h
Growing old is not for sissies.
What must we discover before
we die?
What do those at the end of
their lives have to teach us?
Why do some people find
meaning and die happy?
What does it mean to live a full
and meaningful life?
The 5 Secrets
Izzo asked 15,000 people to sent in names of
wise elders
1,000 responses received
Interviewed 235 ‘wise elders’ ages 59-105
This is what they said……
Be true to yourself –am I following my
heart? Am I focused on things that really
matter? Am I being the person I want to be?
Leave no regrets –constantly asking—“
When I get old and ready to die will I regret
the step I am about to make?’
Become love—love yourself, treat others w
kindness
The Wisdom
Live in the moment—every day,
every moment is a gift. Chose to
be in the moment.
Give more than you take---make
the world a better place. Leave a
legacy.
More questions, comments, or for a
great green chili recipe:
janicemichon@hotmail.com