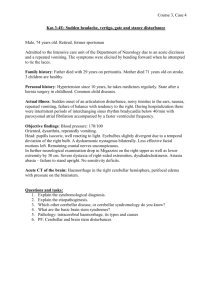
Cervical neurovascular dysfunction
advertisement

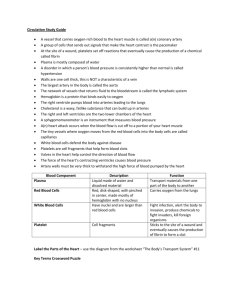
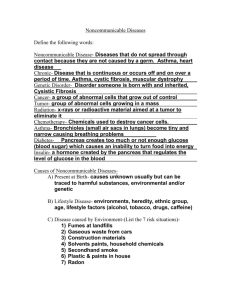
REVISION OF CEREBELLAR AND CEREBRAL DISORDERS & ARTERIAL DEFICIENCIES Caroline Peters CEREBELLUM 2 hemispheres (3 lobes) / 1 vermis 1. Coordination and correction of mvt via cerebellothalamic tract 2. Proprioception via ventral spinocerebellar tract 3. Muscle spindles in trunk and Lex (Clarke’s column) via dorsal spinocerebellar tract 4. Balance via vestibulocerebellar tract 5. Eye movements (same tract) CN III, IV, VI Signs of cerebellar dysfunction Ataxia - in postural co-ordination i.e. a stagger, falling Intention tremor - evident before or during movement, but not at rest Dysmetria - An inability to estimate distance correctly, e.g. on picking up an object, i.e. there is oscillation around the goal and undershoot or overshoot of the target Dysarthria - slow, slurred and explosive speech with pauses in the wrong places Rebound Phenomenon - An inability to break movement Dysdiadochokinesis - An inability to make rapid alternate movements Decomposition of Movement – movements become jerky and irregular A difficulty in performing complex actions involving simultaneous motion at more than one joint. Hypotonia - A decrease resistance to passive movement of limbs Hyporeflexia – pendular Difficulty in carrying out motor sequences that are usually automatic. Oculo-motor disorders – nystagmus (an inability to fix a gaze) Macrographia - Difficulty writing Test the cerebellum Observation Position of the limbs Head deviated to one side Look for tremor Head bobbing Truncal ataxia (vermis dysfunction) Shifting of the feet / wavering unsteady? Romberg’s Test – not a test of cerebellar dysfunction but a test of sensory ataxia Ask the patient to walk - Wide, staggering gait, resembles drunkenness = (B) cerebellar dysf Tandem Walking Test - It is the first function to be lost in alcoholic cerebellar cortical degeneration Head - Observe the eyes for nystagmus / head tilt Observe speech - Ask patient to say “la la la la la“ tests rapid movements of the tongue or “me me me me” tests rapid movements of lips Upper & lower Extremities - Check tone and reflexes Dysdiadochokinesis - Thigh-slapping test / Finger to Thumb Test Test finger–nose–finger - Touch the pad of your index finger with the pad of his or her index finger.+ Hoffmann’s sign Heel–Shin Test - The right heel starts on the top of the left knee and slides down the shin to the foot. Wallenberg syndrome = Lateral medullary ischaemia from occlusion of the vertebral artery (or PICA) nausea, vomiting and vertigo Ipsilateral features: Ataxia from cerebellar involvement. Horner's syndrome from damage to descending sympathetic fibres. Reduced corneal reflex from descending spinal tract damage. Nystagmus.Hypacusis.Dysarthria.Dysphagia.Paralysis of palate, pharynx, and vocal cord.Loss of taste in the posterior third of the tongue. Contralateral findings: Loss of pain and temperature sensation in the trunk and limbs (anterior spinothalamic tract).Tachycardia and dyspnoea (cranial nerve X).Palatal myoclonus (involuntary jerking of the soft palate, pharyngeal muscles and diaphragm). Cerebellar infarction Causes incoordination, clumsiness, intention tremor, ataxia, dysarthria, scanning speech. Early diagnosis is important, as swelling may cause brainstem compression BASAL GANGLIA = collection of nuclei connected to thalamus, cerebrum and brainstem (putamen, globus pallidus, caudate nuclei, subthalamic nuclei, substantia nigra) 1. Ordered 'background' movement 2. Suppression of movement 3. Initiate movement 4. Phasic movement control - e.g. walking/arm swing 5. 'Autopilot’ movement - e.g. swimming 6. Anti-gravity – esp. vestibulospinal 7. Muscle tone - esp. reticulospinal Signs of basal ganglia dysfunction NOT UMN LESION - Normal DOWNGOING plantar, No clonus, NOT 'clasp-knife' rigidity Movement Disorders - often unilaterally initially Involuntary movements Tremor e.g. at rest (Parkinsonian) Micrographia Difficult to get going – akinesia Reduced arm swing on walking phasic movement May affect posture / vestibulospinal Chorea - 'dancing' – continuous rapid, jerky movements < Huntingdon’s, damage to caudate/subthalamic/globus pallidus Athetosis - slow writhing/snakelike < putamen Hemiballismus - Violent, involuntary movement, ipsilateral and in proximal joints < subthalamic nucleus damage Rigidity - Cogwheel - hypertonia + tremor = intermittent resistance / Lead pipe - Sustained resistance Parkinsonism = progressive neurodegenerative disease, 2nd most common after Alzheimer’s Results from the degeneration of dopaminergic neurons in the substantia nigra of the basal ganglia in the midbrain Clinically the disease becomes evident when approximately 80% of the dopaminergic neurons are lost Parkinsons’s Common Symptoms Hypokinesia – motor activity Bradykinesia- slowness of movement Rigidity – lead pipe or cog-wheel Rest tremor Clinical Signs Coarse rest tremor Pill-rolling movements (between thumb and index finger) Cogwheel rigidity Slowness of movement Speech is typically monotonous, soft, faint Expressionless face Small writing - micrographia Shuffling parkinsonian gait – arm swing Other movement disorders Putamen = athetosis caudate, globus pallidus, subthalamic = chorea Subthalamic= hemiballismus (http://www.youtube.com/w atch?v=hqg2GTUq1k4) substantia nigra = Parkinson’s disease BRAINSTEM Midbrain/ Pons/ Medulla (CN III to XII) 1. Autonomic - not distinct anatomically, are associated with autonomic centres in the hypothalamus • Heart rate • Blood pressure • Ventilation • Coughing and vomiting reflex 2. Level of consciousness - and arousal 3. Pain modulation - and site of descending analgesic pathways 4. Habituation - Filters information so that not all input reaches the cortex 5. Extrapyramidal - neurons that influence the motor neurone pool of the spinal cord i.e. muscle tone, posture etc.. Anatomy – brief overview Vertebral arteries – branching off subclavian, ascending though transverse foramina of the 6th to 2nd vertebra, then sweeping laterally to enter trans foramen of C1 before going through foramen magnum to form the basilar artery Basilar artery divides into two post cerebral arteries at the upper pons (PICA) Joined by the carotid and basilar systems they form the circle of Willis at the base of the brain Important points to consider when assessing clinically are: The cerebellum is supplied by branches from the basilar artery (long circumferential, posterior cerebral, anterior inferior cerebellar and superior cerebellar arteries). The medulla is supplied by the posterior inferior cerebellar artery and by direct smaller branches from the vertebral arteries. The pons is supplied by small and large branches from the basilar artery. The midbrain and thalamus are supplied by penetrating arteries from the posterior cerebral arteries. The occipital cortex is perfused by the posterior cerebral artery. 1) Vascular dysfunction Atherosclerosis – most common, causing narrowing and occlusion of large arteries. Only causes vertebrobasilar ischaemia if BOTH vertebral arteries are stenosed at their origin. Embolic occlusion – fairly uncommon. Emboli can originate from subclavian artery or aortic arch Vertebral artery dissection (VAD) – usually in young people presenting with severe occipital headaches and pain in post nuchal region after head trauma Carotid artery dissection (CAD) – more common than VAD. Most common cause of stroke in middle-aged people, typically presenting with neck pain and Horner’s syndrome TIA’s Carotid artery TIA - 90%: Contralateral motor and sensory disturbance Ipsilateral visual disturbanc Monocular blindness - if the TIA is in the ophthalmic artery territory There may be a carotid artery bruit in the neck Vertebrobasilar Arterial Dysfunction / Disease - VAD’) 7% of TIA Vertigo Diplopia Dysarthria Weakness or sensory disturbance affecting one or both limbs Less commonly, impairment of vision, dysphagia Rarely, transient global amnesia, confusion, transient unconsciousness and hearing Lateral medullary ischaemia Result from occlusion of the posterior inferior cerebellar artery or partial occlusion of the basilar artery or vertebral artery S/SS due to infection of the lateral medulla and inferior surface of the cerebellum Cerebellar features: Ipsilateral limb ataxia Vertigo Nystagmus to the side of the lesion - due to damage to the vestibulo-ocular connections Brain stem features Sudden onset of dizziness and vomiting - due to the involvement of vestibular and vagal nuclei respectively Dysphagia and dysarthria - due to lesion to the nucleus ambiguus and vagal nuclei Ipsilateral Horner's syndrome Ipsilateral facial sensory loss - pain and temperature Ipsilateral pharyngeal and laryngeal paralysis - cranial IX and X palsies Contralateral sensory loss - pain and temperature of the limbs and trunk 2) Locked-in syndrome Caused by infarction of the upper ventral pons. Usually dramatic and sudden quadriplegia with preserved consciousness 3) Weber’s syndrome Ventral midbrain affected Ipsilateral mydriasis, cranial nerve III palsy and ptosis. Contralateral hemiplegia. Intracranial bleed (STROKE) Extradural/ Subdural/ Subarachnoid/ Intracerebral 1) Extradural – talk and die! = results from rupture of one of the meningeal arteries that run between dura and skull (middle meningeal artery is most common) Usual cause is skull fracture Effects develop rapidly, bleeding is arterial and at high pressure Commonly follows trauma to the temporal or temporo-parietal region Scalp oedema above the ear may be present Lucid interval - Concussion may be followed by temporary recovery of consciousness for minutes or hours before the onset of drowsiness and possibly coma – TALK & DIE Maybe ipsilateral, dilated pupil Bilateral CN III palsy as rising intracranial pressure > tentorial herniation There may be progressive contralateral hemiplegia 2) Subdural = result from rupture of cortical bridging veins. These connect the extradural venous system > the large intradural venous sinuses, blood fills the space between the dura mater and arachnoid mater. Acute subdural haemorrhage < severe brain injury following trauma Chronic subdural haemorrhage < traumatic or may arise spontaneously Effects develop gradually < bleeding is venous in origin and low pressure Fluctuating conscious level There may be a history of gradual onset of Headaches Memory loss Personality change Dementia, confusion Drowsiness 3) Subarachnoid = bleeding from intracranial vessels in the subarachnoid space Causes 80% due to "congenital" / berry aneurysm (40 to 50 YOA) 10% due to other aneurysms – e.g. arteriosclerotic, traumatic 5% due to arteriovenous malformations 5% due to bleeding disease Sudden severe headache ("my worst headache ever") Headaches in the preceding weeks in 25 to 50% Loss of consciousness or epileptic seizure occurs in 50% Bigger bleeds may cause nausea, vomiting and convulsions Focal signs, e.g. limb weakness, dysphasia may result from a haematoma Presence of a CN III palsy Papilloedema Plantar responses are usually extensor Back pain may arise from blood in the spinal theca 4) Intracerebral = is bleeding into the brain substance with the formation of a focal haematoma. Most commonly due to hypertension, also trauma May rupture through cortical surface > subarachnoid haemorrhage May rupture into ventricular system > intraventricular haemorrhage Cerebral lobes Frontal Lobe Paralysis / paresis Mood changes / Changes in social behavior / Changes in personality Difficulty with problem solving / abstract thoughts Inability to express language < Broca's Aphasia Parietal Lobe: Spatial neglect Agnosia – inability to recognize objects / speech / words etc.. Problems with reading, writing and drawing Mathematics (Dyscalculia) Stereognosis Graphesthesia Occipital Lobes: Most posterior, at the back of the head.- Functions: Defects in vision fields Difficulty with locating objects in environment Visual hallucinations / illusions Temporal Lobes Difficulty in understanding spoken words Short-term memory loss