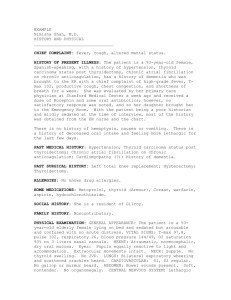
ppt - Tripod
advertisement

Thyroid Debate (Papillary Thyroid Cancer: Extent of Thyroidectomy) 30 Aug 2007 Surgery-OMMC JGGuerra, MD HCruz, MD Papillary Thyroid Cancer: Controversies in treatment • Surgical resection is the key to management of thyroid cancer, but determining the optimal surgical procedure for individual cases has been controversial. • A prospective, randomized study of total vs less than total thyroidectomy is impossible – due to the excellent outcome in the low-risk group – the requirement of long-term follow-up – large number of patients needed to show any statistical difference in long-term survival outcome. • Management protocols for WDTC are based on retrospective data on prognostic indicators (patient risk and tumor risk factors) • Clinicians rely on large patient cohort studies in which therapy has not been randomized, leading to some disagreement about management It is timely to discuss whether total thyroidectomy is a better treatment option compared to subtotal thyroidectomy for a 45F with 2 cm papillary thyroid cancer Premise Is total thyroidectomy a rational treatment of choice for a 45F with 2cm papillary thyroid cancer? YES Arguments 1. 30%-87.5% of papillary carcinomas involve opposite lobe (Hirabayashi, 1961, Russell, 1983) 2. 10%-20% develop recurrence in the contralateral lobe (Soh, 1996) 3. Lower recurrence rates, some studies show increased survival (Mazzaferri, 1991) 4. Facilitates earlier detection and tx for recurrent or metastatic carcinoma with RAI (Soh, 1996) 5. Residual WDTC has the potential to dedifferentiate to ATC Literature Review Databank: Total Thyroidectomy • Analysis of surgical procedures performed in over 1500 United States hospitals reveals that among 5584 patients with thyroid cancer the majority (77.4%) underwent total thyroidectomy regardless of tumor histology and stage (Mazzafferi) Recurrence rates with lobectomy • Performing lobectomy alone may result in a 5– 10% recurrence rate in the opposite thyroid lobe (4,1), a high tumor recurrence rate, and a high (11%) incidence of subsequent pulmonary metastases. Multicentricity • The fact that local recurrence signifies a substantial risk of subsequent tumour-related mortality is emphasized by several workers • Total thyroidectomy eliminates the multicentric microscopic foci present in up to 85% of papillary carcinomas6,12 as potential sites of local recurrence, or the anaplastic transformation that occurs in 1%3 • Patients undergoing lobectomy have a recurrence rate in the contralateral lobe of 5 to 25%, with a mean of 7%, and up to onehalf of these patients eventually die of thyroid cancer, some of whom were initially considered low risk.5 Cancer mortality rates with lobectomy • Hay et al. reported that patients treated for lowrisk papillary cancers [Age, Grade, Extent, Size (AGES) score 3.99] had no improvement in survival rates after undergoing more than lobectomy. • Later, they reported the results of a study designed to compare outcomes after unilateral or bilateral lobectomy for papillary cancer considered to be low risk by AMES criteria. • Although there were no significant differences in cancer-specific mortality or distant metastasis rates between the two groups, the 20-yr rates for local recurrence and nodal metastasis after unilateral lobectomy were 14% and 19%, respectively, significantly higher (P = 0.0001) than the 2% and 6% rates, respectively, seen after bilateral thyroid resection • Hay et al. (30) concluded that bilateral thyroid resection is the preferable initial surgical approach to patients with low-risk papillary cancer • Tollefsen et al reported a 5.7% local recurrence rate in the contralateral thyroid remnant, and 41% of these patients died. Management Options BENEFIT Total Thyroidectomy Subtotal Thyroidectomy Muticentri city RR RISK for Complication COST AVAILABILITY 1-3% RLN injury +++ / <1% +++ / Survival Rate + <5% ++ +++ 1015% + Summary • Retrospective data showed favorable result for total thyroidectomy in terms of – low recurrence rate in the ipsilateral lobe – prevention of development of cancer on the contralateral lobe – acceptable morbidity – facilitation of post operative treatment Thank You References 1. 2. 3. 4. Clark OH. Total thyroidectomy: the treatment of choice for patients with differentiated thyroid cancer. Ann Surg 1982; 196: 361—70 Hay ID, Grant CS, Taylor WF, McConahey WM. Ipsilateral lobectomy versus bilateral lobar resection in papillary thyroid carcinoma: a retrospective analysis of surgical outcome using a novel prognostic scoring system. Surgery 1987; 102: 1088—95. Grant CS, Hay ID, Gough IR, Bergitralb EL, Goellner JR, McConahey WM. Local recurrence in papillary thyroid carcinoma: is the extent of surgical resection important? Surgery 1988; 104: 954—62 Mazzaferri EL, Young RL. Papillary thyroid carcinoma: a 10-year follow-up report of the impact of treatment in 576 patients. Am J Med 1981; 70: 511—8. 5. McConahey WM, Hay ID, Woolner LB, van Heerden JA, Taylor WE. Papillary thyroid cancer treated at the Mayo Clinic, 1946 through 1970:initial manifestations, pathologic findings, therapy and outcome. Mayo Clin Proc 1986; 6: 978—96. 6. Rossi RL, Cady B, Silverman, ML, Wool MS, Homer TA. Current results of conservative surgery for differentiated thyroid carcinoma. World JSurg 1986; 10: 612—22. 7. Shah JP, Loree TR, Dharker D, Strong EW. Lobectomy versus total thyroidectomy for differentiated carcinoma of the thyroid: a marched-pair analysis. AmJSurg 1993; 166:331—5. 8. Tollefsen HR, Shah, JP, Huvos AG. Papillary carcinoma of the thyroid. Recurrence in the gland after initial surgical treatment. AmJSurg 1972;124: 468—72.