Health care reform:
Looking ahead to 2014
Presented by:
Joella Mullin
Managing Director, Carolinas
Wells Fargo Insurance Services USA, Inc.
September 13, 2011
Background
Patient Protection and Affordable Care Act (H.R. 3590) was
signed into law by President Obama on 3/23/10, and
companion bill, the Health Care and Education Reconciliation
Act (H.R. 4872), was signed into law on 3/30/10
– Together, these two bills constitute the new “Federal Health Care
Reform Law” (also commonly referred to as “ACA” or “PPACA”)
From employer’s perspective, ACA consists of four key
interrelated components
– Market reform affecting plan design or administration
– Individual responsibility provisions
– Employer responsibility provisions
– Revenue raisers and other provisions
In terms of effective dates, ACA rolls in on two major waves,
with various turbulence before and after
1
Status of judicial challenges
Individual mandate unconstitutional?
– 2-1 in federal circuit courts upholding constitutionality of individual
mandate
• Michigan: constitutional
6th Circuit agreed – June 29th
• Florida: unconstitutional and not severable (26 states have joined case)
11th Circuit agreed, but severable – Aug. 12th
• Virginia: unconstitutional but severable
4th Circuit hearing reversed and held constitutional – Sept. 8th
– U.S. Supreme Court has denied expedited review request
• Circuits split on constitutionality of individual mandate
• SC ruling not likely until summer of 2012 (or possibly after elections)
• “Swing” vote? “Punt” and say no standing?
• Argument: scope of commerce clause under U.S. Constitution and its
applicability to individual mandate
2
Status of legislative actions
Total repeal of ACA appears quite unlikely
– Insufficient votes to pass Senate or override a Presidential veto
– 2012 election outcomes impossible to predict (both presidential
and congressional races) – 60 Republican Senate seats?
Certain minor amendments have passed
– However, not to really core fundamental reform issues (e.g., repeal
of new Form 1099 reporting rule, repeal of free-choice voucher
rule, funding reduction to co-ops)
Attempts being made to slow implementation
– Some attempts to limit funding and personnel to hinder
implementation and enforcement of law
– Congressional hearings on certain aspects of ACA
– Some Republican-controlled state governments sending mixed
signals re: implementing state insurance exchanges
3
Status of regulatory actions
Regulatory agencies delaying or easing certain
implementation rules
− Six sets of implementation FAQs issued to date
− HHS waiver program from annual dollar limit phase-out for minimed and stand-alone HRA plans
− Delayed enforcement of non-grandfathered insured plan
discrimination (IRC § 105(h)-like) rules
− Revised claims procedures and external review rules (delayed
multiple times)
− Form W-2 reporting obligations delayed until 2012 (or 2013 if < 250
Forms W-2 issued in 2011)
− Automatic enrollment for large employers (>200 employees)
delayed until after guidance issued (likely not until 2013)
− Possible regulatory acceleration of ACA-approved increase in
permissible wellness program incentives from 20% to 30%
4
The first wave –
current status of
federal mandates
5
Federal mandates – key concepts
Grandfathered plans avoid certain mandates
To stay grandfathered
− Avoid the “Big 6” changes (measured relative to 3/23/10):
Elimination of benefits
Any increase in % cost-sharing requirement (e.g., coinsurance)
“Significant” increase in fixed-dollar cost-sharing requirement (e.g.,
deductibles, out-of-pocket limits)
“Significant” increase in co-pays
“Significant” reduction in % of employer contribution rate toward total
cost of coverage
Impose new or decreased annual dollar limits
− Plans can now change policies and/or carriers
But only after 11/15/10 and they still must avoid “Big 6” changes
− What else is permissible?
Everything other than a “Big 6” change, such as changes in Rx
formulary, and changes in eligibility rules
6
Federal mandates – key concepts
Changes applicable to all group health plans
−
−
−
−
−
−
−
−
−
−
No lifetime dollar limits on essential health benefits (2010/2011)
Phase-out of annual dollar limits on essential health benefits (2010/2011)
Phase-out of pre-existing condition limitations (2010/2011)
Prohibition on rescissions of coverage (2010/2011)
Extension of dependent coverage to adult children to age 26 (2010/2011)
Imposition of medical loss ratio requirements on insured plans (2011)
Uniform explanation of coverage distribution requirement (2013?)
Limitation on maximum service eligibility waiting periods (2014)
Reporting value of health coverage on employees’ Form W-2 (2012 or 2013)
Limits on deductibles and out-of-pocket maximums (2014)
Changes avoided by staying grandfathered
−
−
−
−
−
−
Application of IRC §105(h)-like nondiscrimination rules to insured plans (2012?)
Provision of preventive care services without cost-sharing (2010/2011)
Application of revised appeals and external review procedures (2010/2011)
Application of new access to certain health care provider rules (2010/2011)
Plan quality reporting obligation (2012/2013?)
Clinical trial participation rights (2014)
7
Nondiscrimination rule
Non-grandfathered insured health plans must satisfy
nondiscrimination rules “similar” to IRC § 105(h) rules already
applicable to self-insured plans
– Testing exclusions (e.g., < 3 years of service, < age 25 (going to 30?),
certain part-time and seasonal employees, etc.)
– HCIs = highest paid 25% nonexcludable employees, 5 highest paid officers,
and > 10% shareholders
– Benefits nondiscrimination (all benefits provided to HCIs provided to all)
– Eligibility nondiscrimination (boils down to ratio of “benefiting” to total
NHCIs divided by ratio of “benefiting” to total HCIs being at least > ≈ 40%)
Additional guidance anticipated in 2011, but perhaps as late as
2013
Regulators announced non-enforcement policy on 12/23/10 re:
excise tax penalties until set date after release of additional
guidance
8
New Form W-2 reporting obligations
Interim final guidance issued in IRS Notice 2011-28
– Effective for 2012 calendar year (voluntary reporting for 2011)
– Applies to all employers, except for “small “employers (issued < 250 Forms
W-2 for preceding year) and Native American tribal governments
Employer must report value following coverage
– Major medical benefits (insured or self-insured)
– Dental or vision benefits (insured or self-insured), if integrated with major
medical benefits
– Employer-paid fixed-dollar indemnity (hospital or critical illness) or diseasespecific benefits
– Medicare and TRICARE supplements and other similar supplemental
coverage benefits
– On-site medical clinic benefits
– Certain health FSA plans
Excluded coverage:
retiree plans, stand-alone dental or vision plans,
HRAs, HSAs, long term care, liability or accident only plans, most health FSAs
9
New Form W-2 reporting obligations
Reporting mechanics
– Forms W-2 must include the reportable cost of coverage for each employee
and be issued starting no later than January 31, 2013
– Employer can use one of four methods to calculate the value of coverage
(inclusive of both employer and employee costs)
COBRA applicable premium method (exclude 2%)
Premium charged method – available only to fully insured plans based on the
premium charged by carrier for each tier of coverage (e.g. single, two party or
family)
Modified COBRA premium method – only if the employer subsidizes the cost of
COBRA coverage or the cost of COBRA coverage is equal to the previous year’s
cost
Composite rate
– Employer must report coverage provided to an employee throughout the
year including mid-year changes in coverage
10
Summary of benefits and uniform glossary
Two documents
– 8-page “summary of benefits and coverage” (SBC)
• 4 double-sided pages – maximum 12-point font
– Uniform glossary of health coverage-related terms and medical terms
Distribute starting March 23, 2012
SBC to include
– Definitions, coverage details and exclusions, whether MEC and 60%
actuarial value
– Coverage examples
60-day notice only for mid-year plan changes – not at
renewal
11
Penalties for non-compliance with mandates
Excise taxes
– Federal group health plan mandates generally fall under Chapter
100 of the Internal Revenue Code
– In turn, failure to comply with Chapter 100 generally results in
nondeductible excise tax under IRC § 4980D on employers of $100
per day per person to whom the failure relates until violation is
corrected
In certain situations, minimum and maximum amounts may apply
ERISA remedies
– ERISA’s civil enforcement rules also may apply to violations of
federal group health plan mandates
12
Key pending guidance for first wave
mandates
Clarification of, and enforcement date for, various IRC §105(h)
nondiscrimination issues for insured plans
Clarification and effective date of automatic enrollment
requirement for large employers (>200 employees)
Specific services included within each category of “essential
health benefits”
13
The second wave –
2014
14
Fundamental paradigm shift
Employer-provided health care delivery system will be
restructured in 2014 due to following ACA provisions
– Individual mandates
– Two different types of employer “play or pay” mandates
– Health insurance exchanges
Change in employer approach to benefits
– Currently – day-to-day tactical compliance at HR level
• What do I have to do?
• When do I have to do it?
– 2014 – benefits as a strategic investment at C-suite level
• How will my business be affected financially, competitively, otherwise?
• How will my employees (and their families) be affected?
15
New benchmarks and new options
“Acceptable”
Health Insurance
All Employees >
30 hrs/week
“Affordable”
Employee
Contributions
“Fair”
Employee Access
< 400% of Federal
Poverty Line
“Minimum Essential
Coverage” and 60%
Cost Sharing Value
“Individual”
Tax Credits
< 9.5% of Household
Income on Self-Only
Coverage
What is the best way to allocate compensation dollars and manage
your employee benefit program in light of these new federal
standards affecting employer-provided health coverage?
16
Insurance exchanges
General overview
– Basically federally supervised, but state-operated, marketplaces where
health insurance policies meeting specific eligibility and benefits
requirements will be available for individuals and certain employers,
starting in 2014
– Each state must establish at least one exchange (federal government will
operate one if a state chooses not to establish its own)
– Initially only open to employers with < 100 employees (but a state may
lower threshold down to < 50 employees for years before 2016); beginning
in 2017, states may allow all employers of any size to participate
Five coverage tiers will be available
– Four (bronze, silver, gold, and platinum) will vary based on actuarial value
of covered benefits (60%, 70%, 80%, and 90%, respectively)
– One catastrophic tier for individuals up to age 30 in individual market
Coverage subject to modified community rating (no
individual medical underwriting)
– Rates can vary only based on (1) individual or family coverage; (2)
geographic area; (3) age (but only within 3:1 ratio band for adults); and
(4) tobacco use (but only within 1.5:1 ratio band)
17
Employer “play or pay” mandates
Planning Tip – Manage staffing and work hours carefully
• Penalties are based on actual full-time > 30 hours per week employees
• Minimize the number of full-time employees (but perhaps hire more part-time,
seasonal, and/or use leased employees for certain functions)
• Start considering changes in staffing policies now?
Planning Tip – “Do the math” on dropping coverage; address
strategy/philosophy/finance considerations for your business
• “Affordable” coverage may be easier than you think
• Current reasons for offering coverage will still apply, including overall
competitive pressures to attract and retain best possible (and healthiest)
workforce to maximize productivity
• Identify the “sweet spot” in terms of the level and allocation of employer
subsidies to find optimal balance between tax subsidies available for employerprovided coverage and for new Exchange coverage
• Sample strategy: Offer “minimum value” plan that is “affordable” and then
offer supplemental benefits that are “excepted benefits” to selected groups of
employees to let them buy lower cost-sharing features
18
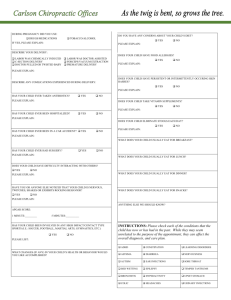
Impact Analysis – Current Plan (projected
to 12/31/2013)
Home
Set-up
HCR Review Key Concepts Impact Analysis Provisions About CHROME
Employer Perspective
Group
Premium
$5,580,622
Premium
Tax Impact
($2,120,636)
FICA Tax
Impact
($619,959)
ER Total
$2,840,025
Employee Perspective
Group
Premium
$4,458,913
Premium
Tax Impact
($1,203,364)
FICA Tax
Impact
($267,787)
EE Total
$2,987,762
Key Considerations:
– Current Costs Trended at 130%
– Salaries Adjusted by 109%
19
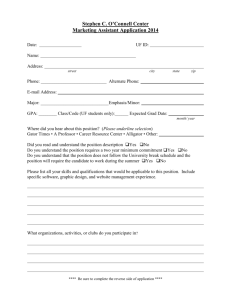
Bottom line summary of HCR Impact Analyzer
Home
Set-up
HCR Review Key Concepts Impact Analysis Provisions About CHROME
2014
No HCR
2014
Maintain
2014
Terminate
2014
ISS
Employer
Perspective
ER Total
$2,840,025
ER Total
$3,403,309
$563,284
ER Total
$5,702,518
$2,882,493
ER Total
$2,271,708
($1,131,601)
Employee
Perspective
EE Total
$2,987,762
EE Total
$2,619,928
($367,384)
EE Total
$4,074,572
$1,086,810
EE Total
$2,572,602
($47,326)
23% increase in employees with coverage
Comparison
to 2014
Maintain
Source: Wells Fargo Insurance Services Health Care Reform Impact Analyzer (powered by CHROME)
20
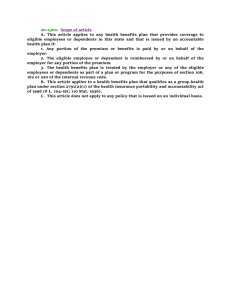
Action plan – Financial perspective
2012
Current
Plan
Optimized
Plan
2013
2014
ER Total
$2,754,824
ER Total
$2,840,025
ER Total
$3,403,309
ER Total
$2,617,083
($137,741)
ER Total
$2,407,716
($432,309)
ER Total
$2,271,708
($1,131,601)
For ABC Company, HCR Impact Analyzer points to an employer-specific
three-year plan that potentially reduces the employee benefit budget
by 18%, and that would be financially optimized in post-2014
environment
21
Questions and answers
The material is provided for informational purposes only based on our understanding of applicable guidance in effect at the time of
publication, and should not be construed as ERISA, tax, or legal advice. Customers and other interested parties must consult and
rely solely upon their own independent advisors regarding their particular situation and the concepts presented here. Although
care has been taken in preparing and presenting this material accurately (based on the laws and regulations, and judicial and
administrative interpretations thereof, as of the date set forth above), Wells Fargo Insurance Services USA, Inc. disclaims any
express or implied warranty as to the accuracy of any material contained herein and any liability with respect to it, and any
responsibility to update this material for subsequent developments.
To comply with IRS regulations, we are required to notify you that any advice contained in this material that concerns federal tax
issues was not intended or written to be used, and cannot be used, for the purpose of (i) avoiding tax-related penalties under the
Internal Revenue Code, or (ii) promoting, marketing, or recommending to another party any matters addressed herein.
© 2011 Wells Fargo Insurance Services. All rights reserved