Welcome to:
Self-Funding, Doing it Right
TX Course #98737
Two Hours CE Credit
Housekeeping:
1.
Please put your phones on silent or buzz.
2.
Please sign in and print legibly
3.
Presentation – There will be a 10 minute
break at the 50 – 55 minute mark.
4.
Please feel free to ask questions for
discussion during the presentation.
5.
Quote/Actions & Quiz Questions
6.
Please complete an Evaluation Survey
Introduction to Self-Funding
o
o
o
o
o
o
o
o
Self-Funding: What is it?
Self-Funding in the Marketplace Today
Fully Insured Model vs. Self Funded Model
The Mechanics of Self-Funding
Self-Funding Scenarios
The Pros and Cons of Self-Funding
PPACA: Impact on Self-Funding
Prospecting and Retention
DISCLAIMER
This presentation is for educational purposes
only. It does not constitute legal advice, nor
does it constitute advice about any particular
set of facts or issues. If you have questions
about a particular set of facts or issues,
consider
independently
consulting
an
attorney or other professional.
© TRIFLEX Corporation, all rights reserved
Pop Quiz:
1. Self-funded health plans are almost always
governed by:
a. ERISA
b. The IRS
c. The state insurance commissioner
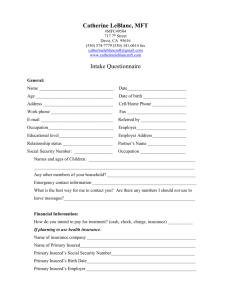
What is Self-Funding?
When an employer group wants to offer health benefits to their employees
but does not want to pay an insurance company. Instead they take the place
of the insurance company and “self insure.”
Two levels of Self-Funding
1. Fully Self Funded
• Group retains all the risk – they do not purchase stop loss
• Usually reserved for “jumbo” cases
• Examples: Microsoft, Walmart, General Motors
2. Partially Self Funded
• Employer purchases insurance policy to take part of the risk
• On a smaller scale a HDHP with an HRA is an example
• Traditional self funded plans purchase stop loss coverage.
Self-Funding in the Marketplace Today
The numbers of employees in self funded medical plans has increased from
44% in 1999 to 60% in 2012.
Self-Funding in the Marketplace Today
Increase in % of Covered Workers Participating by Size:
• 3 - 199 Workers
13% to 15%
• 200 - 999 Workers
51% to 52%
• 1,000 - 4,999 Workers 62% to 78%
• 5,000 + Workers
62% to 93%
Quote/Action
"In the middle of every difficulty comes
opportunity.”
Albert Einstein
Your action is to take one of the challenges you
are currently facing and look for the opportunity
it presents you.
Pop Quiz:
2. Using Disease Management or Wellness
Programs to help control claims exposure are
commonly referred to as:
a. Price Fixing Strategies
b. Cost Containment Strategies
c. Cost Shifting Strategies
Fully Insured Model vs. Self Funded Model
Fully Insured
Self Funded
Employers pay a monthly, pre-determined amount to Employers reserve a monthly, pre-determined
the insurance company.
amount in an interest bearing account.
The insurance company accepts all of the risk
associated with medical claim costs by its enrolled
members.
The employer accepts all of the risk associated with
medical claims costs by its enrolled members.
In an effort to reduce their risk, insurance companies
utilize tools to help minimize medical claims:
- Pre-determined Plan Designs
- Capitation/Network Re-pricing of Claims
- Managed Care
- Large Case Management
- Reinsurance (pooling point)
In an effort to reduce their risk, employers and their
brokers utilize tools to help minimize medical claims:
- Customized Plan Designs
- Network Re-pricing of Claims
- Managed Care through UR/UM
- Large Case Management
- Stop Loss Insurance
The insurance company receives the excess profit
when a group experiences good health and lower
than expected utilization.
The employer retains the excess profit when a group
experiences good health and lower than expected
utilization.
Mechanics: Benefit Design
Plan Document and Summary Plan Description (SPD)
In a self funded health plan, the employer, with the assistance
of their broker, creates, defines and establishes a benefit plan
for its employees.
For groups that are currently fully insured the new plans
are normally modeled after their current fully insured
plans.
Self funded plans are governed by ERISA (Federal law) and
are not subject to State mandates.
Groups have great flexibility in plan design
Who are the Players
1. The Plan Sponsor
2. Consulting Services
3. Legal Services
4. Actuarial Services
5. Accounting and Auditing Services
6. Stop-Loss Insurer
7. Third Parties Providing Administration Services
8. Third Parties Providing Specialized Plan Admin. Services
9. Provider Networks
Mechanics: Paying Claims
Self-insured employers can either administer the
claims in-house, or subcontract this service to a third
party administrator (TPA). TPAs can also help
employers set up their self-insured group health plans
and coordinate stop-loss insurance coverage, provider
network contracts and utilization review services.
Third Party Administrators (TPA)
An Important Distinction: Bundled ASO vs. Unbundled
Independent TPA
Mechanics: Paying Claims
TPAs provide many services to the employer
including:
1. Claim and premium administration
2. Reporting
3. Plan Document Creation
4. Stop Loss Integration
5. Cost Containment Features/Vendors (in house or
sub-contracted)
6. PPO Access
7. COBRA/HIPAA administration
Quote/Action
"The pessimist complains about the wind; the
optimist expects it to change; the realist adjusts
the sails."
Writer: William Arthur Ward
Your action is to think of a problem or challenge
you're facing. Are you approaching it in a
pessimistic, optimistic or realistic frame of mind?
Pop Quiz:
3. The availability of competitive stop-loss
coverage is one of the most critical
components in determining an employer’s
willingness to self-fund.
a. True
b. False
Mechanics: PPO Networks for Medical Claims
Physician Networks (PPO)
Self funded health plans will typically “lease” a PPO network in order to
provide their employees access to physician and hospitals, as well as reduce
the risk to employer’s claim fund by taking advantage of established PPO
network discounts.
PPO Network
Service Type
Charge
Allowable
% Off Billed
PPO A
Outpatient Hospital
$1,614,407
$607,264
63.4%
PPO B
Outpatient Hospital
$1,614,407
$757,724
53.1%
PPO C
Outpatient Hospital
$1,614,407
$957,724
40.7%
Referenced
Outpatient Hospital
$1,614,407
$386,021
76.1%
Items to consider:
• Robust and easily accessible to its members
• Discount structure and payment timeline
• TPA integration
• Accurately priced by the stop loss carriers
Mechanics: PPO Network for Rx Claims
Pharmacy Benefit Management (PBM)
A PBM is essentially an Rx TPA married to a Rx PPO network.
• Provide access to most major pharmacies
• Negotiate discounts on a employer’s behalf
• Manage formularies on behalf of employer (provide
recommendations)
• Many offer mail order and specialty drug programs
Examples: Express Scripts (Medco), CVS Caremark, OptumRx,
Med Impact, Restat
Most TPAs contract with numerous PBMs and are willing to
integrate the Rx claims information in their monthly reporting
and stop loss filing.
Cost saving opportunities: Rebates and Plan Transparency
Mechanics: Cost Containment
Employers can also add numerous features to help manage
both the frequency and severity of claims. These programs are
typically called cost containment.
1.
2.
3.
4.
Disease Management
Utilization Review and Management
Case Management
Bill Audit and Review Services
5. Out of Network negotiation
6. Patient Advocacy
7. Tele-Doc Services
8. Specialty Care Vendors: Dialysis, Hemophilia, etc.
9. Wellness Programs
TPAs and PPO networks will typically provide some of these features.
Mechanics: Stop Loss Insurance
Since the employer is accepting the financial responsibility for
the medical claims there are two main concerns.
1. Large Claimants
2. Over Utilization
Stop Loss insurance provides protection against both scenarios.
1. Specific stop loss coverage covers catastrophic claims
2. Aggregate stop loss coverage covers against “over
utilization” by providing a maximum out of pocket for the
employer’s collective claims.
The availability of competitive stop loss coverage is one of the
most critical components in determining an employer’s ability
to self fund.
Mechanics: Stop Loss Insurance
Specific Stop Loss (Individual)
1. Employer is responsible for all claims on every member until the
deductible is met.
2. Carriers can provide various deductible options to suit a group’s
risk tolerance.
3. The higher the deductible the lower the price for the insurance.
4. Occasionally, specific individuals will be subject to a higher
deductible known as a laser.
Aggregate Stop Loss (Group)
1. Claim maximum (aggregate attachment point) is normally set
25% higher than expected claims (25% corridor)
2. Aggregate can be difficult to secure due to lack of claims data
3. Aggregate coverage is cheap (“sleep insurance”), historically a
group has a 2% chance of hitting their maximum.
Mechanics: Specific Stop Loss Coverage
Specific Stop Loss Insurance (Individual)
Specific stop loss coverage provides protection from
catastrophic losses on each individual insured under the plan.
Example: An employer group with 250 employees selects a
$75,000 specific deductible. Employee John Smith has a heart
attack and the total claims incurred during his hospital stay
totaled $195,000. The employer is responsible for the first
$75,000 in medical claims incurred by John Smith. The stop
loss carrier then reimburses the employer for the $120,000 that
exceeded the specific deductible.
$75,000
Specific Stop Loss Claim Accumulation – ABC Group
100% Stop Loss Carrier’s Responsibility
$75,000-
100% ABC Group’s Responsibility (up to stop loss deductible)
$3,000-
20% Patient Responsibility
80% ABC Group Responsibility
(This is known as coinsurance, where the patient and health plan co-insure
the risk.)
$500Individual Deductible & Copayments (Patient Responsibility)
Frequency & Severity of Claim Utilization
Individual Claim Range
% of Claimants
$0 to $999
80%
$1,000 to $4,999
14%
$5,000 to $9,999
3%
$10,000 to $24,999
2%
$25,000 to $59,999
1%
$60,000 or more
<1%
Total
100%
Mechanics: Aggregate Stop Loss Coverage
Aggregate Stop Loss Insurance (Group)
Aggregate Stop Loss Insurance provides a second layer of protection for self
funded health plans intended to limit the plan’s maximum financial
exposure. The aggregate “deductible” is determined by the insurance
company and is regularly set at 125% of the expected claims for the group.
Example: A stop loss carrier evaluates a 250 EE company’s data and
develops an expected claims attachment point of $2M. They then adjust it
by 25% to arrive at a maximum claims attachment point of $2.5M.
Items to consider:
• Aggregate coverage can be difficult to secure due to a lack of claims
data.
• Aggregate coverage is not always purchased since medical claim costs
rarely exceed 125% of expected claims.
Mechanics: Specific & Aggregate Stop Loss Insurance
Aggregate Attachment Point:
Maximum Claims per Group
(125% of Expected)
$2,500,000
$2,000,000
Expected Claims (100%)
Specific Deductible:
Maximum Claims per Individual
$75,000
John Smith
Quote/Action
"To acquire knowledge, one must study; but to
acquire wisdom, one must observe."
Writer: Marilyn vos Savant
Your action for to observe yourself as if you were
a third party watching you.
Pop Quiz:
4. Stop loss protection for each individual
covered under the health plan is referred to
as:
a. Specific Stop Loss
b. Aggregate Stop Loss
c. Cost Shifting Strategies
30
Mechanics: Stop Loss Contract Options
Standard Stop Loss Contract Options
Since all claims are not received and paid within the Plan Year,
stop loss is sold with various “contracts” offering coverage for
claims incurred prior to the effective date (run-in) and claims
that are paid after the policy year is over (run-out).
Two important terms:
1. Incurred (first number)
• Incurred date refers to the date the member receives care.
• This number designates the number of months qualified claims
can be incurred.
2. Paid (second number)
• Paid date refers to the date the claim is paid by the
administrator.
• This number designates the number of months a qualified claim
can be paid.
Typical turn around time from incurred to paid is 6-10 weeks.
Mechanics: Stop Loss Contract Options – 12/12
12/12
Claims must be incurred and paid in the same 12 month
period.
1/1/2014
12/31/2014
|-------------------------------------------------------------------|
INCURRED
|-------------------------------------------------------------------|
PAID
A 12/12 contract has no Run-In or Run-Out protection.
Sometimes sold with a Terminal Liability Option (TLO).
This contract can be used to help a group transition to
self funding.
Mechanics: Stop Loss Contract Options – 12/15
12/15
Claims must be incurred within 12 months and paid within 3
months following the end of the coverage period.
1/1/2014 12/31/2014
|-----------------------------------------------------|
INCURRED
|-----------------------------------------------------|-----------------|
PAID
3/31/2015
This type of coverage is called Run-Out.
It is also available in contracts on a 12/18 and 12/24
basis.
Fully insured policies are on an incurred basis and
typically offer a 12/24 or greater.
Mechanics: Stop Loss Contract Options – 15/12
15/12
Claims must be incurred within 15 months and paid
in the 12 month coverage period.
|-----------------|------------------------------------------------|
10/1/2013 1/1/2014
INCURRED
12/31/2014
|-----------------------------------------------|
PAID
This type of coverage is called Run-In.
It is also available in contracts on an 18/12,
24/12, and paid basis.
Self-Funding: A Fully Insured Prospect
A prospective client currently offers (3) health plans to its
employees: HMO, Low PPO and High PPO. All plans are
currently fully insured through a major insurance
company. The CEO and CFO of the organization believe
that the insurance company is making money on an
annual, consistent basis off of their workforce’s good
claims’ utilization and costs. They also desire the cash flow
benefits and plan design control that self-funding offers.
The broker and the client work to secure claims data,
enrollment information, plan designs, etc. so that the stop
loss carriers will have enough information to make an
appropriate evaluation of the risk. After working with
multiple stop loss markets, the group receives their stop
loss quote(s) and now have the ability to determine total
cost scenarios including potential claims liability, stop loss
premium and plan administration.
Real Life Scenario: A Fully Insured Prospect
Maximum Liability
Risk Corridor
Expected Claims
$2,950,000
$2,750,000
$450,000
$1,800,000
Stop Loss
$400,000
Ancillary Vendors
$35,000
PPO Access Fees
$65,000
Plan Administration
$200,000
Fully Insured
Premium
Self-Funding: Disadvantages & Potential
Exposures
1. Securing competitive stop loss – group size,
location, available claims data
2. Potential claim liability – claims can come in
above expected
3. Not building claim reserves – claim reserve
underfunded
4. Looting claim reserve for other expenses - can
lead to insolvency
5. Over-generous employers – exceptions are not
covered by stop loss
6. HIPAA Compliance (“hands-on”)
Self-Funding: Advantages
1. Control of the plan design
2. Ancillary service flexibility
3. Collection of health plan data
4. Lower administrative costs
5. Cash flow benefits
6. The ability to build reserves
7. Elimination of carrier profit margin
8. Reduced premium tax
9. Avoidance of Health Insurance Industry tax
Quote/Action
"You always pass failure on your way to success."
Actor: Mickey Rooney
Your action is to think of three failures that were
stepping stones to success.
Pop Quiz:
5. Self-funded health plans are not subject to
the Health Insurance Industry Tax
a. True
b. False
Real Life Scenario: 200 Employee Company
A 200 EE Company was partially self funded through
Principal Financial Group on a minimum premium plan.
Late in 2010 Principal decided to exit the health insurance
market and offered a renewal using UMR (UHC) and BP, Inc.
as the stop loss carrier.
Broker, TPA and the Stop-loss provided stop loss quotes from
6 carriers utilizing HealthComp and the Blue Cross network.
Through an unbundled approach we were able to drop the
group’s maximum liability from $2,698,000 with Principal to
$2,092,000.
Since that time the group has grown but the PEPM costs
have remained steady. They are now entering their fourth
year being unbundled.
200 Employee Company – Unbundling
$1,400.00
$1,200.00
$1,000.00
$800.00
$600.00
$400.00
$200.00
$0.00
10-11
11-12
Unbundled Anthem
12-13
13-14
14-15
Principal Financial
In 2011 Principal Financial decided to get out of the medical business.
Moving to an unbundled self funded plan with HealthComp and
Anthem, the employer was able to reduce their PEPM maximum costs
from $1,128 to $908.
Employer’s overall PEPM trend over the last four years is 0.7%.
XYZ Corporation – Comparison of Administration Costs
XYZ Corporation
Proposed 2014-15 Admin Cost
$400,000
$350,000
$300,000
$250,000
$200,000
$150,000
$100,000
$50,000
$0
UHC - Fully Insured
HealthComp - Self-Funded
ABC Group – Building Reserves
$4,000,000
$3,500,000
$3,000,000
$2,500,000
$2,000,000
$1,500,000
$1,000,000
$500,000
$0
08-09
Attachment Point
09-10
Expected Claims
10-11
Actual Claims
11-12
12-13
Cumulative Claim Reserve
Over a 5 year period ABC Group’s reserve grew to almost $1.2M.
Over a 5 year period ABC Group’s claims came in at 91.2% of expected.
For all 5 years the actual paid claims came in under the expected
claims.
ABC Group’s effective trend was only 7.7% on claims per year.
XYZ Corporation – Building Reserves
$1,400,000
$1,200,000
$1,000,000
$800,000
$600,000
$400,000
$200,000
$0
-$200,000
08-09
Attachment Point
09-10
Expected Claims
10-11
Actual Claims
11-12
12-13
Cumulative Claim Reserve
Over a 5 year period XYZ Corporation’s reserve grew to $215K.
Over a 5 year period XYZ Corporation’s claims came in at 94.3% of
expected.
During the 2011-12 plan year, XYZ Corporation’s claims exceeded the
aggregate attachment point by $9,336.
XYZ Corporation’s effective trend was 12.3% on claims per year.
Quote/Action
"It is not because things are difficult that we do
not dare; it is because we do not dare that they
are difficult."
Philosopher: Seneca
Your action is to do something daring!
Pop Quiz:
6. Administrative Costs associated with a selfFunded Plan are more costly than those
within a fully insured arrangement?
a. True
b. False
PPACA: How It Affects Self-Funding?
Interest is mounting because..
It historically has been even before PPACA. In 1999, 44% of
all employees were covered in a self funded environment.
Today, that number has grown to 60%.
PPACA requires employers with 50 or more employees to
pay or play. This may leave employers looking for health
benefits and self-funding is one of the more long term, cost
effective approaches.
If Massachusetts tells us anything…
The % of employees in self-insured plans with 50 or
more employees rose from 54.6 in 2005-2006 to 67.2%
in 2010-2011.
Better strategic position to adjust benefits to control
increased provider costs.
Fully insured premiums expected to jump to accommodate
new provisions as a result of PPACA.
PPACA: How It Affects Self-Funding?
Interest is mounting continued..
Other considerations:
Limited exposure to MLR rules
Guarantee issue rule, not applicable to stop loss
carriers
Stop loss premiums will not likely be subject to
all the ACA fees
Some additional advantageso
o
o
o
“Essential Health Benefits”
Avoidance of Health Insurance Tax (HIT)
Most premium taxes
State mandated benefits
PPACA: How it affects Self-Funding?
PCORI Fee & Transitional Reinsurance Fees will apply to fully insured
and self funded health plans, however self funded health plans are
exempt from both the Risk Adjustment Fee & Health Insurance Industry
Tax due to ERISA law.
What do the fees equal in savings for the self funded client versus fully insured?
Group Size:
250 Employees
Annual Premium:
$2,750,000
Estimated Renewal Trend:
5%
1/1/2014
1/1/2015
1/1/2016
1/1/2017
Renewal Premium
$2,887,500
$3,031,875
$3,183,469
$3,342,642
Estimated HIT Fees
$66,412
$98,536
$103,463
$133,706
2.3%
3.25%
3.25%
4.0%
HIT %
*For illustrative purposes only. Fee Estimates taken from the Oliver Wyman Study.
Reduced Premium and ACA Taxes
Fully Insured
Annual Premium Premium Tax
Self Funded
Self Funded
Health Ins.
Industry Tax
Total
Premium Tax
Savings
$1,000,000
$25,000
$23,000
$48,000
$5,000
$43,000
$2,000,000
$50,000
$46,000
$96,000
$10,000
$86,000
$4,000,000
$100,000
$92,000
$192,000
$20,000
$172,000
$6,000,000
$150,000
$138,000
$288,000
$30,000
$258,000
$8,000,000
$200,000
$184,000
$384,000
$40,000
$344,000
$10,000,000
$250,000
$230,000
$480,000
$50,000
$430,000
$40,000,000
$1,000,000
$920,000
$1,920,000
$200,000
$1,720,000
Note: Self funded premium tax assumes stop loss premium is 20% of fully insured premium.
Prospecting and Retention
Talk to both your current groups and prospective
groups about self funding.
1. If a group is fully insured offer to do a viability
study to evaluate the competitiveness of selffunding. Request the following:
Current & Proposed Plan Designs
Census: DOB, ZIP, Coverage Type/Tier
2-3 Years Rate History (Renewal if available)
2-3 Years Paid Claims Experience
2-3 Years Large Claim Experience
Prospecting and Retention
2. If a prospect is currently self funded, offer
to do an audit of their self funded plan:
Review the Plan Document and Stop Loss
policy for gaps
Review eligibility language
Review plan exclusions
Analyze claim trends
Review high dollar individuals for cost
containment options
Please take out a business card:
Q – if you want to get QuoteAction
W – if you want to be on our webinar list
C – if you have a case or specific problem to
discuss
Please Complete the
Evaluation
Don Cooper
Founder – TriFlex Corporation
don@triflexcorp.com
469-518-5000
© TRIFLEX Corporation, all rights reserved