Use of PDMP to Improve Patient Care and Outcomes – O'Kane
advertisement

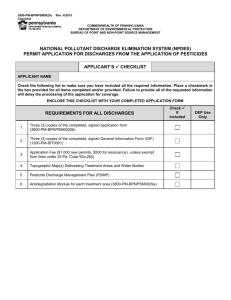
Use of Prescription Drug Monitoring Programs to Improve Patient Care and Outcomes Nicole O’Kane, PharmD Clinical Director Acumentra Health May 30, 2015 Disclosure Statement I have no relevant, real or apparent personal or professional financial relationships with proprietary entities that produce health care goods and services. 2 Agenda 1. Background 2. Who uses the Oregon PDMP? 3. When and how do Oregon prescribers use the PDMP? 3 Acumentra Health • • Portland-based nonprofit consulting firm, dedicated to improving quality, safety, and effectiveness of health care Collaborate with practitioners in all care settings, and with purchasers, communitybased organizations, professional associations, policy makers, and consumers www.acumentra.org 4 Oregon Prescription Drug Monitoring Program (PDMP) • • • • Goal to improve health and public safety Pharmacies submit data weekly Includes data for all controlled substance prescriptions dispensed to Oregon residents Oregon-licensed providers, pharmacists, and their staff can get authorization to access the web-based information to manage patient treatments 5 A Socio-Ecological Model for Behavior 6 Background • PDMPs increasingly used for public health: reduce drug abuse, improve patient safety • Many clinicians who prescribe controlled drugs do not use PDMPs • Little is known about clinician responses to PDMP information 7 Oregon Pain Guidance: Five-Step Approach with Chronic Complex Non-Cancer Pain 1. 2. 3. 4. 5. Practice assessment Patient assessment Non-opioid treatments Patient reassessment Follow-up visits 8 Use of Prescription Monitoring Programs to Improve Patient Care and Outcomes • 5-year grant (2012‒2017) to study effectiveness of the Oregon Prescription Drug Monitoring Program as a clinical decision tool for prescribers of controlled substance medications Supported by the National Institutes of Health, National Institute for Drug Abuse through Grant # 1 R01 DA031208-01A1, and by the National Center for Research Resources and the National Center for Advancing Translational Sciences, through grant UL1RR024140 9 Research Partnership • Acumentra Health • Oregon Health Authority • Principal investigator Richard A. Deyo, MD, MPH, Oregon Health & Sciences University 10 Study Aims AIM 1: Determine the prevalence and characteristics of PDMP users and non-users AIM 2: Determine how providers use PDMP data; formulate recommendations for clinical guidelines AIM 3: Determine whether use of PDMP improves patient outcomes and reduces apparent diversion/abuse 11 5000 Cumulative Number of System Accounts 4500 Cumulative System Accounts 4000 3500 3000 2500 Delegates MD / DO NP / CNS-PP / PA DDS/DMD RPh 2000 1500 1000 500 0 *Delegates were granted access starting in Q1 2014 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 2011 2012 2012 2012 2012 2013 2013 2013 2013 2014 2014 2014 2014 Calendar Quarter 1600 New System Accounts Number of New System Accounts 1400 1200 1000 Delegates MD/DO NP / CNS-PP / PA DDS/DMD RPh 800 600 400 *Delegates were granted access starting in Q1 2014 200 0 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 2011 2012 2012 2012 2012 2013 2013 2013 2013 2014 2014 2014 2014 Calendar Quarter 120000 Total Queries by Discipline Total Number of System Queries 100000 80000 Delegates MD (PA, DO) NP / CNS-PP DDS/DMD RPh 60000 40000 *Delegates were granted access starting in Q1 2014 20000 0 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 2012 2012 2012 2012 2013 2013 2013 2013 2014 2014 2014 2014 Calendar Quarter Number of Users Submitting Queries 5000 Number of Users Submitting Queries Delegates 4500 MD (PA, DO) 4000 NP / CNS-PP DDS/DMD In 2012 - 2013, unique users were counted monthly (and summed quarterly) 3500 3000 RPh In 2014, unique users were counted quarterly 2500 2000 1500 1000 * Delegates were granted access starting in Q1 2014 500 0 Q3 2012 Q4 2012 Q1 2013 Q2 2013 Q3 2013 Q4 2013 Calendar Quarter Q1 2014 Q2 2014 Q3 2014 Q4 2014 2014 Oregon PDMP Annual Report • Only 42% of prescribers who write prescriptions for scheduled drugs have a PDMP account • Of the 4,000 most frequent prescribers of scheduled drugs, only 66% have a PDMP account 16 How Providers Use PDMP • Surveyed a sample of all Oregon clinicians with DEA license • Randomly selected 650 frequent users (>1 query per month) • Of 358 frequent users who returned a survey, 212 agreed to a follow-up interview • Follow-up telephone interviews (n=33) 17 Interview Participants 18 Survey Results: Topics for Learning 1. Workflow 2. Communication 3. Decision-Making 19 Workflow Topics • When do providers check PDMP? Routine versus triggered by “red flag” or suspicion New Rx/patient versus existing patient 20 Results: Workflow • Inconsistent use of routine PDMP checks Some emergency and procedural specialists check routinely when controlled substance is requested; others rely on red flags such as patient behavior Many PCPs check routinely with new patients; for ongoing monitoring with existing patients, some rely on red flags 21 Quotes: Routine vs. Triggered Checks “If somebody immediately starts negotiating their pain medicine or telling me they’ve lost a prescription and/or they’re new to town ― and usually they would say several of those things ― that’s clearly a red flag. But it wouldn’t even take something that overt. If they’re hinting at…they’re low on their medication, and it’s the weekend and they haven’t been able to get in with their doctor, that’s all it usually takes to prompt me to consider or just go ahead and use the Prescription Drug Monitoring Program.” – Emergency Room Physician 22 Quotes: Routine vs. Triggered Checks “I started trying to be less discriminating. If pain is the issue and if I think pain medications are going to be a question, I’ve tried to start doing it almost across the board with those people before I walk into the room. I’m not going to try to pick and choose so much, I’m going to try to do it on most if not all of the people I’m seeing.” – Emergency Room Physician 23 Quotes: New vs. Existing Patients “The new patient that's coming in asking for opiates is going to get at least checked immediately. With existing patients, it will depend on the situation. If I see them frequently wanting medications, maybe after the first or second time, I'll check them. It really depends on what they're asking for. It depends on the feel that I’m getting from the patient. I don’t have a thing I do for every patient.” – Primary Care Clinician 24 Communication Topics • • • Ways in which providers discuss worrisome reports with patients Policies or guidelines that influence checking the PDMP and/or prescribing Ways in which providers discuss PDMP information to assess patient medication compliance and ongoing care 25 Quotes: Ways Providers Discuss Worrisome Reports with Patients • Openly discussing and sharing PDMP results with the patient “For me, it’s a chance to be hopefully less judgmental…and an opportunity to broach the topic. And in an objective, non-judgmental way, to say, ‘Look at this: you’re 20 years old and I see you’ve gotten 160 Vicodin over the last month.’” – Emergency Room Physician 26 Quotes: Ways Providers Discuss Worrisome Reports with Patients • Withholding PDMP results and keeping them a secret “It’s a cat and mouse thing. I keep it secret as much as possible because it’s better used if it’s kept quiet. I can catch the patient unaware…It’s much better for me to have information and I can discover things that are happening. You have to be a bit of a detective.” – Primary Care Physician 27 Quotes: Ways Providers Discuss Worrisome Reports with Patients • Avoid discussing PDMP results with the patient “I never confront them with the evidence from the PDMP. I write it up in the chart, so the chart indicates 18 prescriptions for controlled substances, from six providers over the last year…I’ll flag his chart as drug seeking and that will be his number one diagnosis.” – Primary Care Physician 28 Quotes: Policies or Guidelines That Influence Checking the PDMP and/or Prescribing • Discussing PDMP as part of agency policy or guideline “I tell them that as part of our clinic policy, I need to log in and see if they’re getting these prescriptions from another prescriber. It also helps me to tell them about the policy, the contract that we will have them sign if they start getting them long-term from us.” ‒ Primary Care Clinician 29 Quotes: PDMP Information Communicated as a Tool to Assess Patient Medication Usage • Discussing PDMP results routinely as part of the visit “I communicate much of the time that, ‘It looks like you’ve been filling your Ambien about two weeks late, so it looks like you haven’t been using it every night. What have you been doing to help yourself sleep on the nights that you don’t take it?’” ‒ Psychiatrist 30 Decision-Making Topics • Prescribing decisions in light of worrisome PDMP profile New/episodic patients Existing patients • Referrals Emergency/procedural specialist referral to PCP Referral to behavioral health provider • Discharge from care 31 Results: Prescribing and New Patients • Clinicians generally won’t prescribe for new patient with worrisome profile Some PCPs/clinics had policies against prescribing at first visit or until specific conditions met • Clinicians will prescribe for verifiable acute condition (e.g., broken bone) regardless Emergency and procedural specialists generally won’t prescribe for chronic pain conditions unless authorized by PCP 32 Quotes: New Patients “I just say, ‘I see you’ve gotten multiple scripts filled from multiple providers. I just need to look into this some more, and I’ll see you back in X amount of time, hopefully when I’ve gotten the records, and we can figure out what else we’re going to do for your anxiety or pain management.’” – Primary Care Clinician 33 Quotes: New Patients “I’ll bring the PDMP report back with me and I’ll say, ‘I want to get clear on the information we discussed. You told me you take a Vicodin once in a while, but I have access to your prescription history and when I looked it up, I see you’re getting a regular prescription for this many from Dr. Soand-So, and that’s more than once in a while. So I want you to know before we do treatment, I will not be able to prescribe you any narcotics in addition to what you're already getting.’” – Dentist 34 Survey Results: Prescribing and Existing Patients • Some clinicians discontinue ongoing Rx automatically at worrisome profile Violation of medication agreement • For some, depends on patient circumstances If continue Rx: revisit medication agreement, more frequent monitoring, shorten refill/visit schedule, behavioral health visit • If discontinue Rx: some taper, others do not 35 Quotes: Existing Patients “If they’ve gone to other prescribers, I’ve found it’s most commonly dentists and they don’t think of it as the same thing…I am aware of the kind of mistakes that people make, but when somebody has been to an ER three times in the last month and hasn’t told me, and got prescriptions every time, I simply say, ‘That’s a violation and I can no longer prescribe for you.’” – Primary Care Clinician 36 Quotes: Existing Patients “It depends on their history and the risk of addiction and abuse. We do a risk evaluation when they first come in, so they’re either a mild, moderate, or highrisk patient. If they’re a high-risk patient and something happens, then it’s a lot more severe what I do. If they’re a moderate or low-risk patient, chances are I might not be as controlling. I might just say ‘Okay, you did this ― now we’re reiterating that this is our policy. You can’t do this again.’ Then I’ll watch their drug monitoring program a lot closer and maybe do urine drug screens more frequently.” – Primary Care Clinician 37 Survey Results: Referral and Discharge • • Some emergency and procedural specialists refer patient to primary prescriber/PCP, or may contact PCP to ask about prescribing PCPs and clinicians who provide ongoing prescribing had varied responses Some may discharge if worrisome report; others will not Most offer referrals and/or alternatives 38 Quotes: Referral to PCP/Pain Specialist “If I feel like they have a legitimate reason for wanting more, sometimes I will call their medical doctor or whoever’s been prescribing all the other pain medicine, and talk to them to see if they feel comfortable with me giving the patient more, or ask them if the patient has a legitimate reason for being out.” – Dentist 39 Quotes: Referral to PCP/Pain Specialist “We are not going to manage medications, narcotics at least, for long periods of time. So when I get into situations like that, I would rather refer them to somebody that is better suited to handle a longer-term situation. Or if I think that they’re going to be a problem, somebody that needs to be monitored a little more closely with urine drug screens and things like that.” – Surgical Specialist 40 Quotes: Discharge “Usually the people I choose to discharge from my clinic are the ones who have been getting narcotics multiple other places and haven’t been honest with me.” – Primary Care Clinician “You have to be a really bad person to get discharged from our practice…I think as clinicians, a lot of times we hide behind the Hippocratic Oath or behind this side that we don't want to hurt anybody. Well, we already got all those patients on these medications. It's best that you work with them to turn the ship.” – Primary Care Clinician 41 Conclusions: Workflow • Routine use of PDMP vs. triggered by red flags Some emergency and procedural specialists do not check routinely Some PCPs check routinely only with new patients; for ongoing monitoring, rely on red flags • Need for guidance: What policies or guidelines support optimal use of PDMP? 42 Conclusions: Communication • Some discuss PDMP results openly; • others hold back PDMP results to unearth patient dishonesty Need for guidance: What works best in engaging patient? What should be the role of episodic providers in discussing concerns with patient? 43 Conclusions: Decision-Making • Clinicians are not likely to prescribe for • • new patients with worrisome profile Decisions related to existing patients are varied Need for guidance: For existing patients, when to taper, discontinue, or continue prescription? What is the optimal care related to discharge in response to a worrisome profile? 44 Recommended Next Steps 1. Understand when it is optimal for providers to access PDMP 2. Understand how the various ways of communicating PDMP results may affect provider-patient relationship and ongoing patient engagement 3. Understand how clinic policies or guidelines may affect provider actions 45 Contact Information Nicole O’Kane, PharmD Acumentra Health nokane@acumentra.org Project Funding: National Institute on Drug Abuse, 1R01DA031208-01A1 For more information, please visit: http://www.acumentra.org/PDMP/ 46