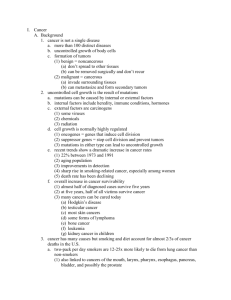
Slackers Reproductive Pathology Fact Stack - U
advertisement
Reproductive Pathology Fact Stack Mike Ori Disclaimer • Faculty has not reviewed or vetted the information contained herein. • If you think this material is any way accurate, you are mistaken. • Celebrity voices are impersonated • Which hormone is responsible for endometrial proliferation and which for increased gland development? • Estrogen is proliferative • Progesterone is responsible for gland maturation • Define dysfunctional uterine bleeding • Bleeding between menstrual cycles caused by abnormalities in the cycle or by systemic disease and not by organic abnormalities. • I.E. Hormone imbalances caused by PCOS, liver disease, etc • Define abnormal uterine bleeding • The occurrence of bleeding at times other than the expected menses. Describe the structure of the endometrium • An epithelium composed of stroma and glands with a relatively constant stratum basalis and a variable stratum functionalis. The latter undergoes cyclic growth, maturation, and degeneration in response to estrogen and progesterone. • Define endometriosis • The presence of endometrial glands or stroma outside the uterine cavity. • Define adenomyosis • Endometrial tissue within the myometrium at a depth of 2+mm from the stratum basalis. • What are the common sx of endometriosis • • • • Dysmenorrhea Menstral irregularities Recurrent pelvic pain Infertility (30-40%) • What are the three theories of regarding the genesis of endometriosis • Menstrual regurgitation • Blood/lymphatic dissemination • Metaplasia • What is the most common organism for suppurative salpingitis • Neisseria Gonorrhea • Distinguish primary fallopian tube adenocarcinoma from secondary (ovarian origin). • Must have a dominant tubal mass involving the lumen of the tube that originates from tubal epithelium. • Define gestational trophoblastic disease • A variety of tumors and tumor-like conditions characterized by proliferation of pregnancyassociated trophoblastic tissue of increasing malignant potential. • Describe hydatidiform moles • Pathologic cystic swelling of the chorionic villi with variable degrees of associated trophoblastic proliferation. Resulting in high levels of HCG, large for gestational age uterus, and passage of small grape-like structures. The distribution is bimodal with peaks in teens and then forties. • Describe the three benign subclasses of moles • Complete – swelling of all or almost all villi with diffuse trophoblastic hyperplasia. These result from the fertilization of an empty ovum by two sperm (2x1n) or by a single 2n sperm. All genetic material is of paternal origin. There is absent or limited vascularization of the villi. • Partial – The fusion of a 1n ovum and 1x2n or 2x1n sperm resulting in a 3n fertilization. The fetus may be viable for weeks and thus fetal parts and an amniotic sac may be present. Both normal appearing and hydropic villi will be seen. HCG level are high but are less than with complete mole. • Invasive – invasion of the myometrium by hydropic villi. Responds well to chemotherapy. • Describe choriocarcinoma • A malignant neoplasm of the chorionic epithelium characterized by a large, bulky, soft, fleshy, yellow-white mass with areas of hemorrhage and necrosis that does not develop chorionic villi. – 50% arise from previous GTD – 25% from normal pregnancy – 25% follow abortion • List the benign ovarian cysts • Follicular cysts – serous > 2cm • Luteal cysts – Lined by layers of granulosa cells conveying bright golden yellow color. Usually regress spontaneously • Cystic follicles – serous < 2cm • List the sx associated with ovarian cancer • • • • • • Pelvic or abdominal pain Pelvic and abdominal swelling Vague but persistent GI issues Unexplained changes in bowel habits Urinary urge and increased frequency Ongoing unusual fatigue • Rank the incidence and prognosis for ovarian, endometrial, and cervical cancer from most common to least common and from most serious to least • Incidence (most common -> least common) – Endometrial > ovarian > cervical • Prognosis (worst -> best) – Ovarian > cervical > endometrial • Which blood test can you use to confirm ovarian cancer • There is no confirmatory blood test. CA-125 is used as a tracking test to monitor progression of the disease. • What are the risk factors for ovarian cancer? • Family hx (Ovarian, colon, prostate (?), breast) • Increasing age • Undesired infertility • What explains the prognostic difference between endometrial and ovarian cancer? • Endometrial cancer presents in post menopausal women with vaginal bleeding – an obvious sign. In contrast, ovarian cancer presents with vague signs that require clinical experience and judgment to recognize as part of a larger syndrome. Hence, ovarian cancer presents at a more advanced stage. • Which cancers is the pap smear diagnostic for? • The pap smear is not diagnostic for any cancer. It is a screening test. Any positive indicator must be followed by culposcopy and biopsy. • What is the average age of a patient diagnosed with breast cancer. What is the male:female ratio • 64 years • 1:100 M:F • Describe the structure of the lactating human breast and the importance of this structure for the development of cancer • Secretory lobules filled with alveoli lined with epithelial and surmounted by myoepithelium. Components are separated by connective tissue stroma and adipose tissue. Lobules connect to the nipple via ducts. Cancers typically arise in the ductal > lobular epithelium • Describe the clinical presentation of breast disease in broad terms • • • • Pain Palpable mass Nipple discharge Mammographic screenin abnormality • Describe acute mastitis • Painful erythematous breast with fever in lactating women. If not lactating suspect inflammatory carcinoma. • Describe periductal mastitis • Painful often recurrent sub-areolar mass in both women and men that is associated with smoking (90%) • Describe fibroadenomas • Well circumscribed, rubbery, freely movable mass that waxes and wanes in response to the menstrual cycle and that typically occurs in women < 30 years of age. • Stromal tumor • Describe phyllodes tumor • Small to large bulbous protrusions with Leaf life slits in an overgrown stroma that typiclly presents in the 50’s. Must be excised with wide margins. • Stromal tumor • Describe fibrocystic changes to the breast • Increased nodularity (lumpy bumpy) of the breast in women in their 30’s and 40’s. It presents without a dominant mass but it often becomes tender premenstrually. • Cysts, fibrosis, adenosis • Up to 60% of cadavers have histologic evidence • Differentiate proliferative breast disease with and without atypia from atypical lobular hyperplasia and estimate the cancer risk of each • Proliferative – Without atypia • Moderate to florid epithelial hyperplasia, adenosis, papilloma, fibroadenoma with complex features • Cancer risk 1.2-2x – Atypia • 4-5x cancer risk for both • Ductal – Resembles DCIS but is quantitatively or qualitatively insufficient • Lobular – Similar to LCIS but affects fewer than 50% of the acini in a lobule. – Always incidental finding • Which breast cancers are found in males? • Pretty much ductal as men should lack lobules. • What is the ratio of ductal to lobular carcinoma in situ. • 80:20 ductal:lobular • Describe the cardinal feature of carcinoma in situ • Lack of invasion past the epithelium’s basement membrane. 45555555 (cat) • What is the risk for invasive carcinoma with DCIS and LCIS and is the risk bilateral? • Both DCIS and LCIS carry a 25-35% risk of invasive carcinoma over 20 years • LCIS indicates bilateral and multicentric risk of 20-40% • What is the lifetime risk of breast cancer for a 90 year-old and what are the general risk factors • 1 in 8 risk (12%) • Risk factors – Age – Increased reproductive life span (menarche – menopause) – Age at primiparity. Older conveys increased risk – Race (caucasian > black > asian > hispanic) – First degree relative with breast cancer – Prior hx of atypical hyperplasia in the breast • List the invasive carcinomas, their frequency as a percentage of all breast cancer, and their clinical appearance Type Frequency Clinical Infiltrating ductal – no specific type 80% Palpable mass with irregular borders and gritty feel. mammographic density. Tubules, nests, cords, sheets of cells Lobular 10% Mass or mammographic density. Cells in single file diffusely infiltrating Medullary 2% See notes. BRCA1 association Mucinous 1-6% Mucin. BRCA1 association Tubular 10% See notes Invasive papillary 1% See notes Inflammatory Clinical morphology. • What are the major and minor prognostic factors for breast cancer. • Major – Invasive v in situ – Metastasis • Lymph node – Inflammatory carcinoma • Distant – Tumor size – Locally advanced • Minor – – – – – – – Histologic subtype Tumor grade ER/PR status Her2/Neu status Lymphovasular invasion (nodal mets = major) Proliferation rate DNA content • What are the zones of the prostate and how do they relate to BPH and cancer? • Peripheral – adenocarinoma • Transitional - BPH • Central • Describe the age correlation with prostate disease • Both BPH and prostatic adenocarcinoma increase with age. The incidence of adenocarcinoma is as high as 70% at age 70 but most are indolent. BPH incidence is as high as 90% at age 70. • Describe the clinical, gross, and microscopic findings for BPH. • Clinical – Dysuria, nocturia, urinary obstruction, hydronephrosis, cystitis, pyelonephritis. • Gross – Enlarged prostate with nodular appearance • Microscopic – Increase glandular and stromal components with a nodular appearance. • Describe the gross, microscopic, and clinical manifestations of prostate adenocarcinoma. • Gross – Yellow-white, gritty, firm growths in the peripheral zone. • Microscopic – Proliferation of small glands that lack the branching and papillary infolding of normal glands. • Clinical – Frequently silent until bone pain presents from mets to spine. May present as masses on digital rectal exam. • What stains differentiate adenocarcinoma from BPH. • Adenocarcinoma glands typically lacks the basal cells whereas BPH glands will stain positive for basal cells. • Describe prostatic intra-epithelial neoplasia. • High grade PIN is considered a precursor for prostate cancer. The overall structure is preserved and the glands stain positive for basal cells but the epithelial cells are neoplastic. • Describe the staging system for prostate adenocarcinoma • Modified TMN • T – 1 – Confined to prostate but found incidentally – 2 – Confined to prostate but found as a result of clinical suspicion – 3 – invading the capsule – 4 – direct invasion of nearby organs • M and N as normal • Describe the gleason system • Adds together the two most common morphologies seen on prostate biopsy to yield a score of 2 – 10. Scores above 7 predicts a worse prognosis. • Describe the utility of PSA • Prostate specific antigen (serine protease) can be used as a marker for prostate adenocarcinoma. It may be falsely elevated for a number of conditions such as trauma, recent ejaculation, prostatitis, and BPH. Levels above 10 ng/mL warrant further investigation. Serial PSA tests are useful to detect changes that may be indicative of cancer. Not all prostate cancers elaborate PSA. • List the fibrotic structural diseases of the penis • Peyronies – chronic fibrosis of the subtunical sheath • Phimosis – Narrowed prepuce that prevents retraction of the foreskin • Paraphimosis – results when phimotic foreskin is forcibly retracted and then cannot return. • What disease is the character of Bert from Mary Poppins at higher risk for? • Scrotal cancer independent of HPV infection. Describe Bowen disease, erythroplasia of Queyrat, and bowenoid papulosis and the relative cancer risk of each. • Bowen and Queyrat histologically appear as carcinoma in situ of the skin of the penis. Lead to invasive squamous cell carcinoma in 10% of cases. Association with HPV 16. – White plaque = Bowen – Red = Queyrat • Bowenoid papulosis present as multiple pigmented papules that histologically resemble bowen but that are not associated with invasive cancer. • To which lymph nodes do cancers of the penis/scrotum, testes, and prostate spread • Prostate – Obturator early then para-aortic later • Penis/scrotum – Inguinal then iliac • Testis – Retroperitoneal (below diaphragm) • What is the clinical significance of cryptorchidism • Left untreated it will result in testicular atrophy leading to infertility if bilateral. • Increases cancer risk 5-10 times if untreated • What are the causes of testicular atrophy • • • • • • Klinefelters Cryptorchidism Radiation Drugs Malnutrition Prolonged exposure to female hormones • What is the likely etiology of Hank and Dean Venture’s testicular torsion? See the PSA on youtube. • http://www.youtube.com/watch?v=BHKMCrD aHRY • Failure of the terminal portion of the gubernaculum to anchor the tunica albuginea to the scrotum. The so-called bell clapper malformation • What is the most common type of testicular tumor and which chromosomal abnormality is it associated with? • 95% are germ cell • 90% of germ cell tumors are associated with isochromosome of short arm of chromosome 12 • Categorize germ cell tumors of the testis. Describe their incidence, spread, and usual treatment. • Seminatous – Peaks in 30’s (seminoma) and 60’s (spermocytic) – Spread via lymphatics – Radiosensitive • Non-seminatous – Peaks in teens to twenties – Spread via both hematagenous and lymphatic routes. – Surgery and chemo • Describe the staging system for testicular cancer • Stage I – Confined to testis, epididymis, spermatic cord • Stage II – Mets to retroperitoneal (sub diaphragm) lymph nodes • Stage III – Distant mets • Describe the seminatous germ cell tumors • Seminoma – – – – – – Peak age in 30’s Placental alkaline phosphatase positive. C-kit (CD-117) positive Uniform population of cells with clear to eosinophilic cytoplasm Lymphocytic invasion in fibrous stroma Similar to ovarian dysgermioma • Spermatocytic seminoma – Peaks in 60’s – Composed of three cell types • Morphology variation in tumor – Non-cohesive cells in scant or edematous stroma – Immunohistochemical stains negative – Rarely mets • Differentiate the non-seminatous germ cell tumors • Embryonal – Large cells with abundant clear to basophilic cytoplasms. – Peak incidence at 30 – CD30 positive • Yolk sac (endodermal) – Schiller-duvall bodies • capillary surrounded by tumor cells – Alpha fetoprotein positive – Median age 16-17 months • Choriocarcinoma – – – – • Invading trophoblast cells Beta HCG positive Median age 25-30 Poor prognosis – in contrast to placental forms Teratoma – Mature are benign in 1-2 year olds – All are malignant in post-pubertal • Differentiate testicular stromal tumors • Leydig – – – – – – • Elaborate testosterone Most common in adults from 20’s-50’s Painless enlargement of testis 10% have malignant potential May cause precocious puberty Usually benign Sertoli – Vimentin and inhibin (variably) positive – Usually benign • Gonadoblastoma – Mixed gonadal dysgenesis (45,X/46, XY mosaicism) – Undergoes malignant transformation to seminoma • Testicular Lymphoma – – – – Difficult to determine if primary or secondary Stains positive for B cell markers CD 19,20 Most common testicular neoplasm over age 60 12% 5-year survival • List the categories of ovarian tumors, their frequency, their age range, and their malignant potential Type Proportion Age Malignancy Epithelial 70% Adult->elder 85-90% Germ Cell 15% Young women 3-5% Stromal 10% Any 2-5% Metastatic 5% Any 100% • List the types of epithelial ovarian tumors • • • • Serous Mucinous Endometriod Clear Cell • Describe in broad terms serous tumors of the ovary. What is their incidence and malignant potential. • Cystic neoplasm of the ovary filled with serous fluid and lined by tall columnar ciliated epithelium • Often bilateral • 30% of ovarian tumors • 75% benign -> borderline • 25% malignant • Note there appear to be conflicts in the notes about percentages as 40% of all malignant ovarian tumors are serous cystadenocarcinomas but only 8% would be by the numbers above. • List and describe the types of serous tumors • Serous Cystadenoma – Benign – From one to a few smooth walled cysts with no epithelial stratification • Borderline (low malignant potential) – – – – Increasing complexity and papillary projections into the cyst cavity. Up to 4-5 epithelial cell layers No stromal invasion Psammoma bodies common • Serous cystadenocarcinoma – – – – Most common malignancy of the ovary (40%) Increasingly solid, papillary, and irregular. Invasion of stroma Psammoma bodies • Describe in broad terms mucinous tumors of the ovary • Multiple cysts lined by mucinous columnar epithelium • 25% of all ovarian tumors • Occur in middle adult life • Typically unilateral • List and describe the mucinous tumors of the ovary • Pseudomyxoma Peritonei – Clinical finding – Implant on peritoneal surface leading to mucinous ascites – Arise from tumors of the ovary or more commonly (?) appendix or other GI tract organs. • Mucinous Cystadenoma – Benign – Tall columnar epithelium with apical mucin – Large cysts filled with sticky fluid • Borderline/low malignant potential – Increased papillary structures and gland complexity. – Up to several layers of epithelium – No invasion of stroma • Mucinous cystadenocarcinoma – 5% of all ovarian cancers – 20% bilateral • remember most other mucinous tumors are unilateral – May be metastatic implant from remote source – Increased stratification and atypia • Describe endometriod carcinoma of the ovary • 40% bilateral • 40% 5 year survival • Grossly resembles endometrial adenocarcinoma • Associated with – Uterine endometriod carcinoma – Endometriosis – Clear cell adenocarcinoma of the ovary • Describe clear cell adenocarcinoma of the ovary • Not associated with DES • Very aggressive • Clear cells • List and differentiate the germ cell tumors of the ovary • Dysgermioma – Similar to testicular seminoma – Good prognosis – Occurs in young adults • Teratoma – Mature are benign in females – Immature are malignant (??) – Mature AKA dermoid cysts • Endodermal sinus tumor (yolk sac tumor) – Elaborates alpha fetoprotein – Schiller duval bodies • Choriocarcinomas (Non-placental origin type) – Less responsive to therapy than placental variety – Usually occur in mixed germ cell tumors • Differentiate the stromal tumors of the ovary • Granulosa-theca cell tumor – – – – – – Older women (2/3 post menopausal) Call-exner bodies Coffee bean nuclei Usually benign Recurrent Elaborates estrogens • Precocious puberty • Endometrial hyperplasia • Theca-fibroma – 90% unilateral – Meigs syndrome • Tumor, ascites, pleural effusion • Sertoli-leydig – Elaborates androgens – Occurs in teens and twenties • Describe CIN, VAIN, VIN • These refer to intra-epithelial neoplasia of the cervix, vagina, and vulva • Very strong associated with HPV 16 and 18 • Leads to squamous cell carcinomas of the affected organ • Cervix is most commonly affected • Describe the staging of cervical adenocarcinoma • Stage 0 – CIN III • Stage I – Confined to cervix • Stage II – Extension beyond cervix • Stage III – Extension to pelvic wall or lower 1/3 of vagina • Stage IV – Extension to nearby organs or distant mets • Differentiate leukoplakia, lichen sclerosis, and lichen simplex chronicus, and malignant melanoma of the vulva • Leukoplakia – Clinical term – Caused by a variety of benign, premalignant, and malignant lesions • May signal premalignancy – Plaque like mucosal thickening • Lichen sclerosis – – – – – • Parchment like pale gray skin Atrophy of the dermis Band like lymphocytic invasion of the dermis Possibly autoimmune Not premalignant but oddly associated with vulvar carcinoma Lichen simplex chronicus – Acanthosis of the squamous epithelium – Hyperkeratosis – Not premalignant • Melanoma – Rare – Peak age 50’s and 60’s • Differentiate pagets disease of the breast and vulva • Histologically similar • Breast has 40% association with underlying invasive ductal carcinoma • Vulvar pagets is rarely associated with underlying carcinoma • Differentiate adenocarcinoma of the vagina from embryonal rhabdomyosarcoma of the vagina • Clear cell adenocarcinoma – Associated with DES use – Most tumors in upper 1/3 of vagina – Women in teens • Embryonal rhabdomyosarcoma – AKA sarcoma botryoides – Presents in infancy and early childhood – Grape like structures composed of malignant rhabdomyocytes. – Often protrudes into the vagina or out the intraoitus • Describe the etiology and appearance of endometrial hyperplasia • Arises from excess estrogen stimulation as a result of – estrogen elaborating tumors – unopposed exogenous estrogens – HPG axis issues – PCOS • Excess growth of endometrial tissue • List the classifications of endometrial hyperplasia and their likely progression to cancer. • What is the new terminology replacing the older classification scheme Without atypia Atypia Simple 1% 3% Complex < 8% 29% •Old scheme •Four types as above •New scheme •Endometrial intra-epithelial neoplasia • List the types and etiology of endometrial cancer, their age of onset, and the prognosis • Type I – Endometriod – Endometrial hyperplasia – PTEN and MSI gene changes – 50-60’s, less aggressive, good if early • Type II – – – – – – Serous Clear cell Carcinosarcoma P53 gene changes Resting endometrium 60’s-70’s, more aggressive, poor • Describe the grading system for edometrial carcinoma • FIGO (Histologic) – Grade 1 < 5% solid – Grade 2 6-50% solid – Grade 3 >50% solid • Nuclear grading – Grade 1 – not too messed up (minimal atypia) – Grade 2 – somewhat messed up (intermediate) – Grade 3 – really messed up (marked atypia) • Describe carcinosarcoma and list its rapper name • Endometrial adenocarcinoma accompanied by malignant stroma often resulting in a grossly large mass that extends beyond the uterus. • Rapper name: trip-M – Mixed mullerian malignancy • Differentiate leiomyoma from leiomyosarcoma • Leimyoma – – – – – Benign smooth muscle tumor Well circumscribed Up to 25% of women Multiple lesions common Estrogen responsive • Regresses post menopause • Leiomyosarcoma – – – – Malignant smooth muscle tumor Peak incidence 40’s-60’s Bulky mass commonly with hemorrhage and necrosis 40% 5 year survival