The Study Coordinator's Role in Investigator originated studies
advertisement
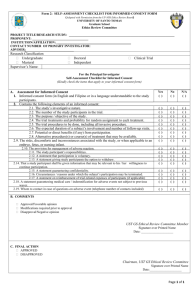
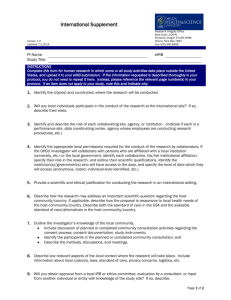
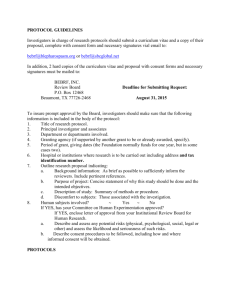
The Study Coordinator’s Role in Investigatororiginated Studies Diane Davies RN Manager, Clinical Research Unit Helen Diller Family Comprehensive Cancer Center Consultant: CTSI and QIU Let’s talk about you, the study coordinator …… •Educated, motivated and you like and care about people!!!! •As a study coordinator you often become attached to the patients and want what is best for the patients and their families!!!! Skills you bring to the position: •Verbal Communication •Written Communication •Information Technology Skills •Problem Solving •Organizational Skills •Teamwork with Peers Skills you will acquire as a Study Coordinator: •Ethical Conduct-Maintaining Data Integrity, GCP Guidelines •Drug/Device/Biologics Development •Clinical Care in a Medical Center Setting •Clinical Trial Budgets & Financial Management •Medical and Scientific Terminology •Regulations and Guidelines applicable to Clinical Research •Data Management •Leadership •Teamwork among Medical Professionals Objectives Define an investigator-originated study Define your role in the 3 stages of a study I. Pre-study (study set up period) II. Study Conduct Period III. Data Analysis and Closeout An investigator-originated study is defined as… •A study that is the PI’s original or collaborative idea. •The PI owns the data •These studies are often sponsored by the NIH or other agencies that grant money for scientific ideas. Other Funding •At UCSF investigators can also use gift or departmental funds to finance a study •Drug manufacturers can also finance this type of study. –These studies are usually called Investigator Sponsored Trials or IST’s –The manufacturer will supply the drug/device and may pay per patient enrolled Investigator-originated studies include: •Therapeutic (intended to cure or prolong a life) •Symptom management •Prevention •Early detection/diagnostic •Correlative – Imaging/ tissue/ blood •Population-based studies: •Epidemiology/Surveys/Observational •Quality-of-life The Principal Investigator is responsible for: •The entire conduct of the study •Protocol design •Funding and approvals from contracts and grants •Human subject approvals •Data collection and analysis •Publication of results The investigator must assure the welfare of all subjects enrolled: •Subject management: recruitment practices, HIPAA policies informed consent process •Adverse event identification and reporting: Any serious adverse event must be reported to the UCSF CHR and if your investigator holds an IND or IDE that event must be reported to the FDA through MedWatch reporting program The Investigator and the Study Coordinator SC are hired to “coordinate” the study, you are not “responsible” for the study….. this can be a fine line between you and the PI Developing a rapport with your PI: – Use the Delegation of Responsibilities Log to start your conversation with the PI – The Log is found on the QUI website – Ask your PI about their vision of the study • Will this lead to further studies • Will this device or drug provide new information • Do they have plans for an abstract or publication/ timeline The important role of the SC • Human Subject Protection – Ensuring that the study and consent have current CHR approval – The most current consent is used, the consent process has occurred and all patients questions have been answered. – Subject safety, the protocol is followed and all serious adverse events are identified and reported Examples of SC responsibilities • CHR applications, renewals and reporting of SAE / protocol violation • Scheduling subject visits/ collection of biological samples • Interviewing subjects / Collection of questionnaires • Abstracting study data into database or Case Report Forms • Data Integrity • Liaison with Medical Center • Study Budgets you should know about……. Regulations for Human Subjects Office of Health and Human Services & Office for Human Research Protections (OHRP) http://www.hhs.gov/ohrp Food and Drug Administration http://www.FDA.gov Code of Federal Regulations 21 CFR parts 11, 50, 54, 56, 312, 314, 812, 814 45 CFR part 46 The organization that is responsible for providing the infrastructure at UCSF for clinical research is the Human Research Protection Program ( HRPP) Committee on Human Research (CHR) applications and renewals Quality Improvement Unit (QIU) post approval reporting The CTSI Clinical & Translational Research Institute http://ctsi.ucsf.edu/ Find Consultation Services Search Research Cores at UCSF Use Clinical Research Center CTSI Consulting Services • • • • • • Biostatistics Study Design and Implementation Data Management Ethics Health Policy Bioinformatics Data Analysis CTSI Consulting Services • Regulatory Knowledge (RKS) Consultation – Regulatory requirements (including FDA and IRB) – Interactions with regulatory authorities – Regulatory strategies across the spectrum of preclinical to late phase clinical research • http://ctsi.ucsf.edu/research/rks-consult-preview Drugs/Biologics and Devices A investigator who files an IND or IDE application must comply with: i. Code of Federal Regulations (CFR) title 21 – 312 (FDA regulations) ii. International Conference on Harmonization (ICH) topic E6, Guidelines for Good Clinical Practice (GCP’s) If you need advice contact CTSI- RKS Clinical Research Centers Inpatient and Out-patient locations • • • • • • • • San Francisco General Hospital Moffitt Hospital Mount Zion Hospital Moffitt Pediatrics Hospital Tenderloin Center CHORI Children's Hospital Adults Kaiser Oakland Research Unit Veterans Affairs Medical Center CTSI- Clinical Research Centers Services • • • • • • Nursing Services Bionutrition Services Body Composition & Exercise Laboratories Sample Processing Newborn Intensive Care Neurodevelopmental Evaluation Prestudy •What is the objective of the study? •Who is the target population? •What are the risks to the subject? •How and where is the research conducted? •What are your resources? Prestudy •CHR application •IND/IDE application •See your MSO regarding: •study budget •your role with Grants and Contracts •space and work supplies See the Clinic Manager and Administrative Nurse for both outpatient and inpatients care areas orientation Recruitment plan The grant application will define the study population and target accrual Tips: Where is the study population located, recruitment methods, in person/by letter /by phone or advertisement Take a look at the study events and determine the enrollment plan Make sure your study is registered at Clinical trials.gov after you receive CHR approval Pre-study data collection preparation The data collection needs to support the study objectives How are you going to gather the data? How are you going to record and store the data? Work with the statistician and PI on the data collection methods What is source documentation ? • The original recording of data, such as the B/P on a VS sheet, a RN/MD note, clinic note, medication record or infusion records / surgical dictation • Any signed notes by care providers • Test (lab or image reports) downloaded from STOR • ER record • Telephone notes Pre Study • Subject visits– Layout an enrollment schedule – the visit schedule can snowball and resources will not be available • PI/MD time • Clinic schedule/OR schedule • Interviewers availability Set up a pt. calendar to inform patients of the visits and location of appointment ( Maps/printed directions / parking lots Source documentation you may need to develop • Inclusion/ Exclusion checklist • Drug compliance diaries or symptom diaries (make sure the subject signs the diary as you collect it) • Log to collect adverse events • Log to collect concomitant meds • Log documenting the collection of blood or tissue samples What is an Adverse Event • Any change in the subject health, a new symptom, an accident or new diagnosis after the subject has received a drug or device or during a medical procedure • These are documented on all device or drug trials while subjects on study • They are classified by grade 1-5, or mild, moderate or severe and death. Relationship to the experimental drug or device must be included Questionnaires • When using a validated questionnaire you do not need source documentation – FACT – QOL – Depression Scales Make sure the form has the subject identifier and date of completion- some forms require a signature Case Report Forms (CRF’s) • CRF’s is the paper or electronic form that collect the data needed for study analysis • Paper vs. Electronic data base – Use unique identifiers (initials and study number) – If data is missing indicate by UNK – Code entries/ do not use text • PE Normal = 1 abnormal= 2 not done =3 Your Primary Role in Data Collection is to Maintain Data Integrity •Complete and accurate accumulation of information as specified in the study protocol •Followed by the accurate transfer of this information (data) to the data collection method •It is preferable to use electronic data entry, set –up in secure relational database versus paper forms or an Excel file Regulatory Files • Set-up and Maintain Regulatory Binder or File – IRB required on-study documentation • • • • • • • Initial approval and approved consent Protocol modification Single Subject exceptions Informed consent modifications Annual renewals Onsite serious adverse events Official Communication with the CHR Enrollment and Screening Logs •Create a log to track all potential subjects •Screening logs (initials and dates/ keep copies of the consents) •Enrollment logs: •Name, DOB ,contact information •Date of consent •Demographics (reporting to granting agencies) •Dates of treatment / evaluation or 1st questionnaire Are you ready? Must have full CHR approval including recruitment materials !!! Grant and contracts must have full authorization and final signatures !!! Is the study is registered on Clinical Trials.gov ? Is the Fund/ DPA set up with a ZZ account ? Do you know how to link study subjects on IDX ? Screening and Enrollment Document clearly: Consent procedure •Determining eligibility – •time frame of testing is often very important •use a checklist •Obtain signatures of the PI/ NP or other supervisor •Collect supporting documentation •Review with PI and obtain signoff •Inform the patient of the next steps, who informs the subject that they can participate in the study ?? Give study calendar to the subject with projected dates and set up the next appt. •Randomization –who will inform the patient if the study is not double blind The subject has been enrolled: What are my next steps? Ensure protocol interventions are carried out in a safe and timely manner per protocol guidelines: i. Procedures ii. Laboratory/radiology tests iii. Study drug administration Study Implementation and Documentation • Documentation specific to protocol – Note should start with protocol number – Investigator or staff should clearly document informed consent process and any re-consenting – Investigator / RN should document dosing and dose modifications. – Investigator should document relationship of adverse events to study participation, management of event, and when it resolved Study Implementation • Data Collection – Abstract data from a variety of sources to complete CRF – Obtain medical reports; forms for off-site offices – Create and maintain source documents/shadow charts – Enter information on the CRF database/paper Study Implementation • Maintain study drug supply/devices – Shipping receipts, dispensing log • Document communications with “Medical Science Liaison (MSL)” regarding study conduct • Maintain worksheets for investigator/division to track on-study activities, costs, and scheduling Study conduct • Scheduling subject visits and exam- this can be very time consuming • Keep up with the subject data collection • Use study chart (shadow file) to have medical records at your desk • Do not forget to set aside time for data entry, double check or have someone audit your data • Review the data with the PI, find out when a presentation or abstract is planned Study Conduct • Keep your subject log up to date, track all study visits • Review the billing charges to your study • Liason with your dept finance personnel • Enter the date off study or completion of study • If long term follow up of subjects is required create a method to track the next contact –(use an electronic calendar or excel spreadsheet with calculations The PI and SC relationship Keep your PI and other investigator informed of any changes and updates – Meetings 1:1 – Weekly e-mail – Team meeting Ask your PI how s/he wants to be informed. What s/he needs to know about immediately, or at the end of the day or in a weekly meeting. The study has ended, what now ?? • • • • All subject follow-up has ended All data is collected Has the pharmacy been notified All data is entered into a data base and the data base is “lock” • If you are not going to be contacting a subject or reviewing medical records the study may be “retired at CHR” • Notify the CHR using the study close-out report Data Analysis • Discuss your role with the PI • Organize the study charts and regulatory files • Make sure the PI has the electronic data and there is data back-up • Remind the PI to acknowledge the CTSI on publication • You may want to send subjects a thank you for their participation and results of the study. Research Protocol Coordination Pre-Activation Protocol Design and Feasibility Prepare Regulatory Documents Staff Education Initiation Meetings Treatment/ Activate Team Recruitment Patient/Family Education Informed Consent Adverse Event Collection On-going Data Collection Tumor Response Assessment Protocol Modifications Off-Study Follow-up Eligibility Report to IRB Begin Data Collection Dose Modifications Off-Study Follow-up Budget Study Close-Out Report to Sponsor/IRB Report Back To Sponsor Update Patient and Team Seven Ethical Principles* 1. 2. 3. 4. 5. 6. 7. Social or scientific value Scientific validity Fair subject selection Favorable risk-benefit ratio Independent review Informed consent Respect for subjects *“What Makes Clinical Research Ethical,” Emanuel. More Training • Collaborative Institutional Training Initiative – “CITI” required by the CHR for all key personnel • Clinical Trials Networks Best Practices • Medical Center Annual Safety Training • Safe Shipping and Biohazards • Blood-borne Pathogens • Vaccinations and TB testing- Occupational Health – see your HR dept • Research Billing (FOT-519) • IDX, STOR, U-CARE Study tools from the QUI Below is a collection of tools to assist in the conduct and management of clinical research: • Delegation of Authority Documentation Log • Screening / Enrollment / Withdrawal Log • Regulatory File Checklist • Drug or Biologic Dispensing / Accountability log • Device Dispensing / Accountability Log – Example: Study Events Tracking Form – Example: Tracking System for Deadlines and Reporting Learn more about your job • Organizations – ACRP http://www.acrpnet.org – SOCRA http://www.socra.org • Contact Beverly Fein at bfein@cc.ucsf.edu for local chapter info – Research Practitioner http://www.researchpractice.com These sites have information for subjects about participation in clinical trials • http://www.fda.gov • http://www.cancer.gov/clinical_trials • http://www.centerwatch.com