What do we need to know?
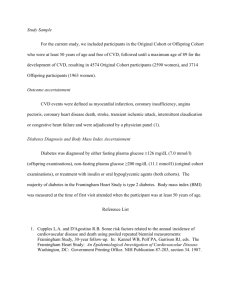
advertisement
Myths Facts Men are more likely to have heart disease Heart disease is the #1 killer of men and women; 50,000 more women than men die of heart disease every year Cancer is a bigger threat than heart disease Nearly twice as many US women die from heart disease and stroke than from all cancers combined Doctors are aware of women’s risk for heart disease and act accordingly Undertreatment and underdiagnosis of heart disease in women contributes to excess mortality in women “… The community has viewed women’s health almost with a ‘bikini’ approach, looking essentially at the breast and reproductive system, and almost ignoring the rest of the woman as part of women’s health ….” Nanette Wenger, MD Chief of Cardiology, Grady Hospital Professor of Medicine, Emory University Atlanta, Georgia 2.5 million women per year in the US are hospitalized with cardiovascular disease (CVD) Deaths from CVD = 500,000/yr Leading cause of death in US women: CAD 1990: US Congress directed the National Institutes of Health that women be included in clinical trials and that gender differences be evaluated 1 in 5 women has some form of CVD 38% of women who have a heart attack die within 1 year 40% of coronary events in women are fatal › Most occur without prior warning Deaths in Thousands American Heart Association. 2002 Heart and Stroke Statistical Update. 2001 Typical in both sexes Pain, pressure, squeezing, or stabbing pain in the chest Pain radiating to neck, shoulder, back, arm, or jaw Pounding heart, change in rhythm Difficulty breathing Heartburn, nausea, vomiting, abdominal pain Cold sweats or clammy skin Dizziness Typical in women Milder symptoms (without chest pain) Sudden onset of weakness, shortness of breath, fatigue, body aches, or overall feeling of illness (without chest pain) Unusual feeling or mild discomfort in the back, chest, arm, neck, or jaw (without chest pain) Percent of Population 90 80 70 60 50 40 30 20 10 0 79.00 70.7 Males Females 65.2 65.20 51.0 48.10 34.2 28.90 10.4 5.5 4.60 4.20 20-24 25-34 17.4 13.60 35-44 45-54 Ages 55-64 65-74 75+ American Heart Association. 2002 Heart and Stroke Statistical Update. 2001 More than35,000 women under the age of 65 die annually in the US from CVD 72% of young women (ages 25-40) still consider cancer to be the greatest threat to women’s health Some women know about the risks of heart disease but do not hear it from their own doctors and do not “personalize” it Robinson A. Circulation. 2001 65% of women recognize that symptoms may be “atypical” but do not know classic symptoms Most women learn about coronary artery disease (CAD) from magazines and the Web—not from their own physicians! 1 Perceived health threats Leading causes of death in women 55% 2 46% 40% 24% 22% ci de n ts 3% Ac eu m on i PD Pn C O ce r C an C AD ta ck rt H ea di rt at se as e r H ea Br ea st ca nc e ce r C an 4% a 4% 2% 1. Gallup survey. 1995 2. American Heart Association. Heart & Stroke Facts. 1996 Statistical Supplement US Vital Statistics, 1990 Traditional Paradigm: Menopaus e Minimal or no CVD Risk Increasing Risk of CVD Alternative Paradigm: Increasing Risk of CVD Menopaus e Decades of time The reality: Being premenopausal probably High Blood Pressure, does not protect youSmoking, from cardiovascular Age, Heredity Cholesterol, disease and you should Diabetes, beElevated vigilant at all ages … Inactivity, Obesity Critical to reproductive function in men & women Most produced by ovaries Some arises from fat, liver, breasts, adrenals Complex physiologic effects Secondary prevention › 1998: HERS 4 years of treatment with conjugated estrogen plus medroxyprogesterone acetate No reduction in the risk of MI and coronary death in women with established CAD HERS trial. JAMA. 1998. Secondary prevention › 3/2000: Estrogen Replacement and Atherosclerosis trial (ERA) 309 postmenopausal women with CAD Placebo vs conjugated estrogen (.625 mg/day) vs conjugated estrogen (.625 mg/day) with medroxyprogesterone acetate (2.5 mg/day) Angiographic analysis of the diameter of the coronary arteries at the start of the study and 3 years later ERA trial results at follow-up angiography › The progression of coronary atherosclerosis was unchanged in the women randomized to either of the estrogen groups ERA trial. J Am Coll Cardiol. 2001 16,608 Postmenopausal women aged 5079 with an intact uterus Estrogen + Progesterone Placebo Hormonal replacement associated with: •Increased heart disease (29% ↑) •Increased stroke (41% ↑) •Increased blood clots •Increased breast cancer (26% ↑) •Reduced colon cancer •Reduced hip fracture Study stopped after mean followup of 5.6 years RCOG UPDATE (11 June 2013): The British Menopause Society (BMS) and Women’s Health Concern recently published a literature review In summary, their key recommendations are: The decision whether to use HRT should be made by each woman having been given sufficient information by her healthcare professional, including information about complementary therapies and lifestyle and dietary changes. HRT dosage, regimen and duration should be individualised, with an annual evaluation of the pros and cons Arbitrary limits should not be placed on the duration of usage of HRT; if symptoms persist, the benefits of hormone therapy usually outweigh the risks. HRT prescribed before the age of 60 has a favourable benefit/risk profile. It is imperative that women with Premature Ovarian Insufficiency (POI) are encouraged to use HRT at least until the average age of the menopause. If HRT is to be used in women over 60 years of age, lower doses should be started, preferably with a transdermal route of administration. 60 50 40 Mortality Rate per 1,000 30 Women with Diabetes 20 Women without Diabetes 10 0 0-3 4-7 8 - 11 12 - 15 16 - 19 20 - 23 Duration of Follow-up (yrs) Sources: Krolewski 1991, National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) 2002. 33 65% of diabetics die from heart disease or stroke 4.2 million American women have diabetes › Diabetes increases CAD risk 3-fold to 7-fold in women vs 2- fold to 3-fold in men › Diabetes doubles the risk of second heart attack in women but not in men American Heart Association Centers for Disease Control and Prevention Manson JE, et al. Prevention of Myocardial Infarction. 1996 Framingham Heart Study › Women with diabetes mellitus had relative risk of 5.4% for CAD vs women without diabetes › Men with diabetes had relative risk of 2.4% Nurses’ Health Study › Relative risk of 6.3% for total cardiovascular (CV) mortality › Even if women had diabetes for <4 years, their risk of CAD was significantly elevated Kannel W. Am Heart J. 1987 Manson J, et al. Arch Intern Med. 1991 Abdominal obesity › Men › Women Triglycerides HDL cholesterol › Women › Men Blood pressure Fasting glucose >88 cm (>40 in) >80 cm (>35 in) (TG) >150 mg/dL <50 mg/dL <40 mg/dL >130/>85 mm Hg >100 mg/dL National Heart, Lung, and Blood Institute Framingham Heart Study Relative Risk (x-fold) 2.5 2.2 Women Men 2 1.85 1.8 1.45 1.4 1.5 1.2 1 1 0.55 0.65 2.15 1.3 1.25 1.25 300 350 400 1 0.8 0.75 100 150 0.5 0 50 200 250 Castelli WP. Can J Cardiol. 1988 Single most preventable cause of death in US Smoking by women causes 150% more deaths from heart disease than lung cancer Women who smoke are 2-6 times more likely to suffer a heart attack Nurses’ Health Study: Even a few cigarettes a day correlated with a greater risk of CVD or fatal MI About one-quarter of all women smoke; prevalence greatest among postmenopausal women 39 Younger women who smoke probably cancel out any premenopausal protection Women who take oral contraceptives and smoke are more likely to have an MI or stroke than those who take the pill but don’t smoke Puts a woman at greater risk for CVD and poorer outcomes Depression also may increase risk or defer her from seeking medical help Consider screening women with CAD for depression and refer for treatment as needed 41 Lack of exercise is a proven risk factor for heart disease › A lack of regular physical exercise is a growing epidemic all over the world. “We seem to eat much more than what we burn” Heart disease is twice as likely to develop in inactive people than in those who are more active Physical activity helps maintain weight, blood pressure, and diabetes Women should exercise to increase heart rate for 20-30 minutes a day, 3-5 times per week Women are underrepresented in cardiovascular (CV) trials › Evidence-based CV medicine biased toward men Food and Drug Administration/National Institutes of Health mandate: 50% enrollment of women Women need to be empowered to enroll in clinical trials for heart disease › Breast-cancer awareness is a good example Coronary MVD is heart disease that affects the heart's tiny arteries. This disease is also called cardiac syndrome X or nonobstructive CHD. In coronary MVD, the walls of the heart's tiny arteries are damaged or diseased. Women are more likely than men to have coronary MVD. Many researchers think that a drop in estrogen levels during menopause combined with other heart disease risk factors causes coronary MVD. Although death rates from heart disease have dropped in the last 30 years, they haven't dropped as much in women as in men. This may be the result of coronary MVD. Stress Rest Thrombolysis – equally effective – Cerebral hemorrhage risk is more Low rates of coronary angiography in women Under referral for revascularization procedures CABG - > operative mortality 1.9 % v/s 4.6% Restenosis after PTCA, or CABG occlusion rates are more for women - ? Smaller lumen sizes Women have higher hospital readmission rates for unstable angina, reinfarction, heart failure, ventricular tachycardia, and ventricular fibrillation. Main goals: Reduce risk and restore functional capacity 51 parameter Changes at various times (weeks) 5 12 20 24 32 38 HR ↑ ↑↑↑ ↑↑↑ ↑↑↑ ↑↑↑↑ ↑↑↑↑ SBP ↔ ↓ ↓ ↔ ↑ ↑↑ DBP ↔ ↓ ↓↓ ↓ ↔ ↑↑ ↑↑↑↑↑ ↑↑↑↑↑↑ ↑↑↑↑↑↑ ↑↑↑↑↑ SV ↑ ↑↑↑↑↑ CO ↑↑ ↑↑↑↑↑↑ ↑↑↑↑↑↑↑ ↑↑↑↑↑↑↑ ↑↑↑↑↑↑↑ ↑↑↑↑↑↑↑ SVR ↓↓ ↓↓↓↓↓ ↓↓↓↓↓↓ ↓↓↓↓↓↓ ↓↓↓↓↓↓ ↓↓↓↓↓ LV EF ↑ ↑↑ ↑↑ ↑↑ ↑ ↑ ↑ ≤ 5%; ↑↑ 6-10%; ↑↑↑ 11-15%; ↑↑↑↑ 16-20%; ↑↑↑↑↑ 21-30%; ↑↑↑↑↑↑ > 30%, ↑↑↑↑↑↑↑ > 40%. Plasma volume ↑ 50% (20100%). “Physiologic anemia of pregnancy”. Estrogen-mediated stimulation of the RAS. Role of other hormones › deoxycorticosterone, prostaglandins, estrogen, prolactin, placental lactogen, GH, ACTH, ANP From Pitkin RM, Nutritional support in obstetrics and gynecology. Clin Obstet Gynecol 1976;19:489 CVD Mortality per 100,000 Women HTN – Hypertension GDM – Gestational Diabetes PCOS – Polycystic Ovary Syndrome Source: Adapted from “CVD Prevention and the Primary Care Partnership”, Deborah Ehrenthal, MD, FACP 55 Anxiety, pain, uterine contraction. Oxygen consumption ↑ threefold. ↑ CO during labor (↑ SV and ↑ HR). ↑ SBP & DBP (especially 2nd stage) Those changes are influenced by the form of anesthesia and analgesia. Increase in venous return (relief of caval compression) Blood shifting “auto-transfusion” (from the contracting uterus to the systemic circulation) Increase in effective blood volume Blood loss during delivery Substantial increase in LV filling pressure, SV and CO Clinical deterioration • HR and CO return to pre-labor values within 1 hour. MAP and SV within 24 hours. • Hemodynamic adaptation persists post partum and return to pre-pregnancy values within 12-24 weeks after delivery. Before conception History Exercise capacity Current or past evidence of HF Associated arrhythmias Physical exam Cardiac Hemodynamics Severity of heart disease, PA pressures Echo, MRI. Exercise testing Useful if the history is inadequate to allow assessment of functional capacity During pregnancy Evaluate once each trimester and whenever there is change in symptoms Multidisciplinary approach, Fetal Echo During Labor & Delivery Multidisciplinary approach (Obstetrician, Cardiologist, Anesthesiologist) Tailor management to specific needs Reimold, S. C. et al. N Engl J Med 2003;349:52-59 Pulmonary HTN and Eisenmenger’s syndrome. Symptomatic obstructive cardiac lesions: › AS, PS, uncorrected coarctation of the aorta. Marfan’s Syndrome with dilated aortic root. Systemic ventricular dysfunction (LVEF < 40%). Severe cyanotic heart disease. Patients with prosthetic valves. Significant uncorrected CHD. Lesion Maternal death rate (%) • Severe Pulmonary Hypertension 50 • Severe obstructive lesions: AS,PS, HOCM, Coarctation. 17 • Systemic Ventricular Dysfunction, NYHA class III or IV 7 The prevalence of clinically significant maternal heart disease is low (<1%)1. Its presence increases the risk of adverse maternal, fetal, and neonatal outcomes2. 1. 2. Siu SC, Sermer M, Colman JM, et al. Prospective multicenter study of pregnancy outcomes in women with heart disease. Circulation 2001;104:515-521. Siu SC, Colman JM, Sorensen S, et al. Adverse neonatal and cardiac outcomes are more common in pregnant women with cardiac disease. Circulation 2002;105:2179-2184. Preeclampsia (pre-e-KLAMP-se-ah) is a condition that develops during pregnancy. The two main signs of preeclampsia are a rise in blood pressure and excess protein in the urine. These signs usually occur during the second half of pregnancy and go away after delivery. However, your risk of developing high blood pressure later in life increases after having preeclampsia. Preeclampsia also is linked to an increased lifetime risk of heart disease, including CHD, heart attack, and heart failure. (Likewise, having heart disease risk factors, such as diabetes or obesity, increases your risk for preeclampsia.) If you had preeclampsia during pregnancy, you're twice as likely to develop heart disease as women who haven't had the condition. You're also more likely to develop heart disease earlier in life. Severe AS is poorly tolerated. › AVA < 0.7 cm2, Mean PG > 50 mmHg. › Mortality up to 17%. Symptomatic patients or Mean gradient > 50 mmHg → Delay conception until after surgical or interventional correction. Consider balloon valvuloplasty, Ross procedure, tissue valve (no need for anticoagulation). Symptomatic patients before end of 1st trimester Terminate pregnancy. Β-Blockade, Bed rest. Palliative aortic balloon valvuloplasty or AVR. Early Delivery. Reimold, S. C. et al. N Engl J Med 2003;349:52-59 Hameed A, et al. The effects of valvular heart disease on maternal and fetal outcome of pregnancy. J Am Coll Cardiol 2001;37:893-9. Warfarin Heparin Crosses the placenta. ↑early abortion, prematurity, and embryopathy when used in 1st trimester (6th–12th weeks). CNS & Eye abnormalities (2nd & 3rd trimester). Bleeding in the fetus (especially at delivery) › Should be stopped before delivery. Does not cross the placenta No teratogenicity No fetal bleeding Twice daily SC injection Risk of osteoporosis › › <2% symptomatic fractures. but 30% decrease in bone density. Risk for thrombocytopenia ↑↑ Risk of thrombosis Antibiotic prophylaxis at the time of delivery is not recommended for patients expected to have uncomplicated vaginal delivery or cesarian section, unless clinically overt infection is present 1,2 Patients at high risk for endocarditis may receive antibiotics at the discretion of their physician2: › Those with prosthetic heart valves. › Previous IE. 1 Sugrue D, Troy P, McDonald D. Antibiotic prophylaxis against infective endocarditis after normal delivery -- is it necessary? Br Heart J 1980;44:499-502. 2 Dajani AS, Taubert KA, Wilson W, et al. Prevention of bacterial endocarditis: recommendations by the American Heart Association. JAMA Most women with heart disease can have a pregnancy proper care. Pre-pregnancy evaluation mandatory. High-risk cases benefit from combined high-risk OB and cardiac care in the same center.