AQuA_ERPP_Practical_Steps_for_Getting_Started
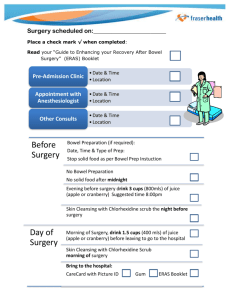
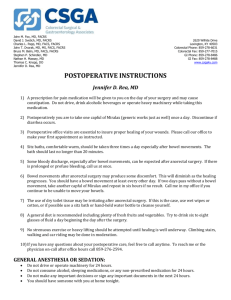
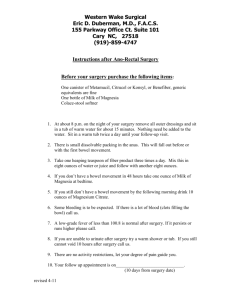
advertisement
Practical Steps for Getting Started Wendy Lewis Programme Manager © 2012 AQuA This session: • Discuss the key elements of your local implementation plan • Practical activities to get you started • Based on the Implementation Guide • Access to advice, guidance and support © 2012 AQuA 2 Implementation Plan 1. Stakeholder analysis 2. Stakeholder engagement 3. Engaging with Commissioners 4. Team working 5. Understanding your current service 6. Understanding the risks 7. Understanding the investment required 8. Maintaining momentum 9. Testing and making changes to your pathway 10.Sustaining the change Implementation Plan 1. Stakeholder analysis 2. Stakeholder engagement 3. Engaging with Commissioners 4. Team working 5. Understanding your current service 6. Understanding the risks 7. Understanding the investment required 8. Maintaining momentum 9. Testing and making changes to your pathway 10. Sustaining the change Stakeholder Analysis High Influence Satisfy Manage •Opinion formers Key Stakeholders need to be fully engaged through full communication & consultation •Keep satisfied •Review regularly Inform / Monitor Little / No Influence Not crucial to the process but useful to keep informed Little / No Interest Involve •Voices that need to be heard •Need to be proactive High interest Stakeholder Analysis – Activity On the blank map provided start your stakeholder analysis by identifying your stakeholders with high influence and high interest that you need to actively manage High Influence Satisfy Manage •Opinion formers Key Stakeholders need to be fully engaged through full communication & consultation •Keep satisfied •Review regularly Little / No Influence Inform / Monitor Involve Not crucial to the process but useful to keep informed •Voices that need to be heard Little/No Interest •Need to be proactive High interest Identifying the team Implementation requires a number of factors: • Changing clinical interventions • Changing care systems and processes • Creating a team to work across the patient pathway • Both require technical and behavioural change management • Lets start with thinking about who to engage and how to structure the project team Essential Roles Sponsors: •authority to sanction change (organisational alignment / benefit) Change Agents •facilitate change, require knowledge, skills and credibility Champions •respected opinion leaders who positively promote work •lead by example Optimal Project Leadership CEO or Executive Sponsor Project Lead / Manager Project Leadership Clinical Leads Information Support Ham 2001 (Report for NHS MA) ©NHS Institute for Innovation and Improvement 2006 Identifying the Team - Activity • Consider who will take the roles of: – Sponsor? – Change Agent? – Champion? • Who will take the essential project roles: – Project Lead / Manager? – Clinical Lead? • Who will provide information management support? Understanding your current service Referral from Primary Care • Optimising pre operative haemoglobin levels • Managing pre existing co morbidities e.g. diabetes PreOperative •Admission on day •Optimised Fluid Hydration •CHO Loading •Reduced starvation •No / reduced oral bowel preparation ( bowel surgery) •Planned mobilisation •Rapid hydration & nourishment •Appropriate IV therapy •No wound drains •No NG (bowel surgery) •Catheters removed early •Regular oral analgesia •Paracetamol and NSAIDS •Avoidance of systemic opiate-based analgesia where possible or administered topically Admission •Optimised health / medical condition •Informed decision making •Pre operative health & risk assessment •PT information and expectation managed •DX planning (EDD) •Pre-operative therapy instruction as appropriate •Minimally invasive surgery •Use of transverse incisions (abdominal) •No NG tube (bowel surgery) •Use of regional / LA with sedation •Epidural management (inc thoracic) •Optimised fluid management Individualised goal directed fluid therapy IntraOperative PostOperative •DX when criteria met •Therapy support (stoma, physio) •24hr telephone follow up Follow Up Understanding your current service- Activity Referral from Primary Care On the • Optimising pre operative haemoglobin levels • Managing pre existing co morbidities e.g. diabetes map provided: Pre- •Admission on day •Optimised Fluid Hydration •CHO Loading •Reduced starvation •No / reduced oral bowel preparation ( bowel surgery) •Planned mobilisation •Rapid hydration & nourishment •Appropriate IV therapy •No wound drains •No NG (bowel surgery) •Catheters removed early •Regular oral analgesia •Paracetamol and NSAIDS •Avoidance of systemic opiate-based analgesia where possible or administered topically • Mark the Operative interventions you already have in place You should also consider when, where and how they are provided and whether Admission there is further opportunity for/ improvement •Optimised health medical condition •Informed decision making •Pre operative health & risk assessment •PT information and expectation managed •DX planning (EDD) •Pre-operative therapy instruction as appropriate •Minimally invasive surgery •Use of transverse incisions (abdominal) •No NG tube (bowel surgery) •Use of regional / LA with sedation •Epidural management (inc thoracic) •Optimised fluid management Individualised goal directed fluid therapy Intrayou Operative need to • Identify the interventions establish and start to consider the sequence for Postimplementation Operative •DX when criteria met •Therapy support (stoma, physio) •24hr telephone follow up Follow Up Understanding and improving systems and processes Patient Pathway Undertake mapping and tracking Increasing level of detail Measuring and understanding the baseline Measurement Aspect Improvement Accountability Research Aim Improvement of care Comparison, choice, reassurance, spur for change New knowledge Methods: Tests are observable No test; merely evaluate current performance Test blinded or controlled tests Bias Accept consistent bias Measure and adjust to reduce bias Design to eliminate bias Sample Size “Just enough” data, small sequential samples Obtain 100% of available, relevant data “Just in case” data Flexibility of No hypothesis Fixed hypothesis Hypothesis Hypothesis flexible, changes as learning takes place Testing Strategy Sequential tests No tests One large test Determining if a Change is an Improvement Run charts or control charts No change focus Hypothesis, statistical tests (t-test, F-test, chi square), p-vlaues Confidentiality of the Data Data used only by those involved with improvement Data available for public consumption and review Research subjects’ identities protected Test Observability Measures for improvement • Outcome – Length of stay – Patient experience • Balancing – Re-operations – Readmissions – Complications • Process – ER pathway interventions Benefits Realisation Using Measures for improvement - Activity Look at the list of programme measures: •How will you make your baseline measurement? •How will measure on an on going basis? •How you will use the measures to drive improvements? Steps for Improvement - Right first time and every time • First step - Reduce defects such as avoidable infections • Second Step – Reduce waste (cost) such as losing and repeating a blood test • Third Step – Enhancements or new features such as a new treatment or cure Invest in Quality Improvement - the Sand Cone Model Ferdows and De Meyer 1990 Model for improvement What are we trying to accomplish? How will we know that a change is an improvement? What changes can we make that will result in the improvements that we seek ? Copyright IHI 2000 Act Plan Study Do aims measures change principles & ideas testing ideas before implementing changes Using multiple tests of change D S A T A A D A P D S P A Changes that result in improvement S D P A P Hunches theories ideas S D Need to start small!! Managing improvement low Test on a very small scale Agreement amongst the key players Just do it JDI high high Certainty that the change will work low MeasuringChanging the impact of the tests of change process Journey Time (hours) 25 Changed Process 20 Second Process Change 15 Third Process Fourth Change Process Change 10 5 0 Jan Apr Jul Oct Jan Apr Month Jul Oct Jan Apr Jul What will be your first test of change? Remember the importance of a quick win as well as a plan for sustainability Critical Factors for Sustainability ©NHS Institute for Innovation and Improvement 2006 Making it Happen • Will • Ideas • Execution IHI Framework for Leadership for Improvement 2008 Advice guidance and support • Literature and toolkits • AQuA ER Network • Websites - AQuA Portal • Who in your local organisation can help?