Olecranon Bursitis
advertisement

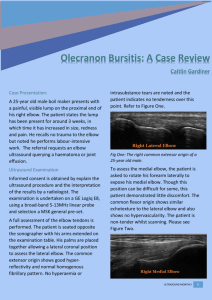
Musculoskeletal Medicine for Medical Students Olecranon bursitis Author: Joseph Bernstein Version: 8 Date: 06-Apr2014 11:37 Table of Contents . 1 Description 3 . 2 Structure and function 4 . 3 Patient presentation 5 . 4 Clinical Evidence 6 . 5 Epidemiology 7 . 6 Differential diagnosis 8 . 7 Red flags 9 . 8 Treatment options and outcomes 10 . 9 Risk factors and prevention 11 . 10 Miscellany 12 . 11 Key Terms 13 . 12 Skills 14 1 Description Olecranon bursitis is a condition in which the soft tissue overlying the olecranon at the elbow is inflamed. Inflammation of the olecranon bursa can be the result of direct trauma, repetitive use, or inflammatory conditions such as gout or rheumatoid arthritis. Occasionally, the fluid in the olecranon bursae can become infected – a condition that requires surgical drainage. Often, however, the olecranon bursitis runs an innocent course. CLINICAL PHOTO of Olecranon bursitis Version 8 3 Olecranon bursitis 2 Structure and function The body places bursae (the plural of "bursa") in those areas where the normal structures must glide (e.g. the skin overlying the olecranon) to facilitate that gliding by reducing friction. The word “bursa” literally means “sack”, however, it is best to think of these “sacks” as plastic bags (similar to those used to hold trash or groceries, say), in their compressed, unused state. That is, a healthy bursa is like a plastic bag before it is filled: namely, a structure with two layers of material, closely opposed; layers that glide smoothly against each other. Only when they are filled (with bursal fluid or groceries in bursae and plastic bags respectively) do they become “sack-like”. That is, whereas the inner surfaces of bursae can become filled with fluid (and hence earning their container-connoting name), in the natural state they are empty. If the bursa is filled with fluid, but is not inflamed or infected, sometimes the fluid can be resorbed over time. However, if it does not resorb itself, the fluid can become infected. Bursitis is the clinical entity in which the bursa becomes inflamed and fluid-filled. This inflammation can be caused by direct trauma, repetitive use, prolonged pressure and systemic inflammatory conditions (such as gout or rheumatoid arthritis). Bursitis can be caused by infection directly, e.g. insect bite or puncture wound. At times, fluid collecting for other reasons can become secondarily infected. Version 8 4 Olecranon bursitis 3 Patient presentation The hallmark of olecranon bursitis is a mass at the elbow over the olecranon. Tenderness, redness and warmth are classic signs, but may be absent. At times the mass is not at all painful, unless pressure is applied. Olecranon bursitis can be caused by conditions such as rheumatoid arthritis or gout, and therefore the presentation may be colored by co-existing symptoms of those conditions (for example, arthrosis within the elbow itself). Patients on dialysis seem to be at particular risk for olecranon bursitis (for reasons that are not entirely clear). At times there is a history of direct trauma to the elbow; sometimes there is a history of repetitive use; and at other times there is no antecedent history at all. Even in cases where the bursa is not painful, hyper flexing the elbow can produce pain, as this motion tends to increase the pressure within the bursa. Along those lines, bursitis may impede full range of motion. Version 8 5 Olecranon bursitis 4 Clinical Evidence Fluid from olecranon bursitis can be drained and sent for culture. Culture is the definitive test; gram staining may be negative in many cases that ultimately turn out to be infectious. X-rays may show an olecranon spur. There may be calcification within the bursa itself. An MRI can demonstrate the fluid collection but is rarely indicated. MRI of Olecranon bursitis Version 8 6 Olecranon bursitis 5 Epidemiology The precise prevalence of olecranon bursitis is not known. It is a common condition, and therefore high (if not first) on the differential diagnosis list of painless masses on the elbow. Approximately 20-25% of cases of known septic bursitis turn out to be infectious. Approximately 5-10% of patients on dialysis may have this condition. Version 8 7 Olecranon bursitis 6 Differential diagnosis There are two levels of diagnostic thinking required: first, “is this mass bursitis?” And second, “if this is bursitis, what has caused it?” (Along those lines, the question “is this bursa infected or prone to be?” should be kept to the forefront.) A mass overlying the elbow in the setting of normal radiographs (or radiographs showing only calcification within the bursa) can be considered bursitis until proven otherwise. The causes of bursitis usually can be deduced from the history. As noted, increased redness, warmth, and tenderness (especially in a patient with an imperfect immune system) should prompt an infection work-up. Version 8 8 Olecranon bursitis 7 Red flags Bursal fluid can serve as a culture medium and easily become infected. Approximately 25% of cases of olecranon bursitis will turn out to be infectious. Septic bursitis is heralded by more redness and warmth, and is much more likely to be painful. Patients on dialysis should be suspected of having septic bursitis. Septic bursitis can be diagnosed definitively with an aspiration and culture. A cell count of the aspirate can be a useful clinical guide for initiating empiric treatment. CLINICAL PHOTO showing aspiration of olecranon bursitis Version 8 9 Olecranon bursitis 8 Treatment options and outcomes The first line treatment of aseptic bursitis includes rest, compression (with ace wrap), ice and NSAIDs. Also, ensuring that any underlying process that may be responsible (e.g. gout) is well controlled is a wise step. Minimizing the gliding across the bursa may help control the bursitis, but in general the elbow is apt to get stiff when immobilized; as such, prolonged immobilization should be avoided. Typically, immobilization with ace wrap will provide enough compression but will not immobilize the elbow completely. If the first line treatment is not successful, needle aspiration (with the addition of a steroid) can be helpful. Aspiration can be diagnostic as well as therapeutic. If sepsis is considered, aspiration should be performed and antibiotics started. If the infection does not clear after the first aspiration and antibiotics, surgical drainage may be needed. Treatment of bursitis tends to be effective, yet recurrence is common. That is often the case because the inciting cause remains present, e.g. a worker continues to put pressure on the elbow, or the gout flares again. In general, however, long-term impairment is rare. Version 8 10 Olecranon bursitis 9 Risk factors and prevention People whose occupations require resting on the elbows – for example carpet installation or gardening – are best served with elbow pads. Dialysis and immune compromise in general are risk factors for infectious bursitis that cannot be prevented per se. Vigilance to make sure that infections are detected early is best. Version 8 11 Olecranon bursitis 10 Miscellany The "bible" remedy used for ganglion cysts (smashing the mass with a heavy book) is a poor choice for olecranon bursits. If nothing else, a heavy blow may damage the skin and increase the chance of infection. The word bursa is similar to the word “bursar”, the official at a university who collects the tuition – and carries it away in money sacks. The simple English word “purse” has a similar root. Version 8 12 Olecranon bursitis 11 Key Terms Bursa; bursitis; aspiration Version 8 13 Olecranon bursitis 12 Skills Recognize bursitis and associated “red flags”; aspirate bursa under sterile conditions Version 8 14 Olecranon bursitis