Everyone Wants To Go To Heaven…. But Nobody Wants to Die
advertisement

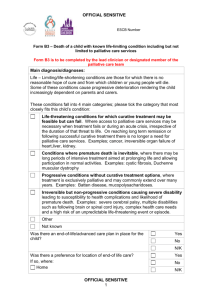
Everyone Wants To Go To Heaven…. But Nobody Wants to Die Jean Gordon RN, MSN, CHPN Director of Education, QA/PI Hospice of East Texas Objectives Identify evolving trends in end of life care, with a focus on palliative care . Differentiate between hospice and palliative care programs. Dr. Atul Gawande – a surgeon and staff member of Brigham and Women’s Hospital and the Dana Farber Cancer Institute in Boston “Letting Go”, The New Yorker, August, 2, 2010 Our medical system is excellent at trying to stave off death with chemotherapy, intensive care, and surgery. But, ultimately, death comes, and no one is good at knowing when to stop. “In the past few decades, medical science has created a new difficulty for mankind: how to die, due to the seemingly unstoppable momentum of medical treatment.” Do you want everything done? What the patient/family hears Resuscitation Ventilator Surgery, transplants…. Cure Return to normal life What the physician/nurse means We’ll try CPR, if you insist. Evolving Realities Life expectancy has increased Increased prevalence of chronic disease Increased comorbidities and frailty with advancing age adding to complexity Death is considered by many -to be “optional” 25% of all Medicare spending is for 5% of patients who are in their final year of life; and most of that money goes for care in their last couple of months…. which is of little apparent benefit. Atul Gawande MD, The New Yorker, August, 2, 2010 Finley, E. & Casarett, D. (2009). Making Difficult Discussions Easier: Using Prognosis to Facilitate Transitions to Hospice. CA Cancer J Clin What Do Patients Want?? Realistic prognostic information Straightforward communication Time and ability to ask questions Sensitivity, empathy, & “expertise” Assurance of non-abandonment Appropriate transition to palliative care Challenges Difficulty with patients and/or families accepting that effective treatment is no longer available Or… that patient has fewer than 6 months to live. Certain people have the skills to cope well and go gently into the night, while many never come to terms with the fact that they are dying. Some understand that death is imminent but aren’t emotionally accepting of it and fight to stay alive at any cost. Casarett, D. & Quill, T. (2007). “I'm Not Ready for Hospice": Strategies for Timely and Effective Hospice Discussions. Annals of Internal Medicine. 146 (6). “What should medicine do when it can’t save your life?” “Modern medicine is good at staving off death with aggressive interventions and bad at knowing when to focus, instead, on improving the days that terminal patients have left.” Atul Gawande MD, The New Yorker, August, 2, 2010 “How can we build a health-care system that will actually help dying patients achieve what’s most important to them at the end of their lives.” Atul Gawande MD, The New Yorker, August, 2, 2010 Restoring the Balance Palliative Care Life Prolonging Care Trends in End of Life Care Greater emphasis on ‘reasonable’ care through: 1. New legislation 2. ‘AND’ orders 3. Palliative care teams/services The Palliative Care Information Act bill (S. 4498 Duane/ A. 7617 Gottfried), has passed both houses of the NY State legislature and is awaiting signature by New York’s Governor David Paterson. If signed, the bill “requires physicians to discuss all end of life options.” http://www.examiner.com/x-59793-NY-Healthy-LivingExaminer~y2010m7d30-NY-Governor-considers-law-to-promptdiscussions-about-end-of-life-decisions?cid=email-this-article The health reform bill that passed April, 2010 included a Medicare pilot project to allow 12 communities across the country to offer both curative treatment and hospice services to terminal patients to evaluate whether physicians would refer earlier and patients would accept hospice earlier. Supportive Versus Palliative Care: What's in a Name? Palliative Care as a term was seen as more distressing to providers, patients, and families than Supportive Care and perceived as synonymous with hospice and with giving up hope. Treatment implies that something active will be done and that there is still hope, whereas care is viewed as less active and devoid of hope. Fadul N, Elsayem A, Palmer JL, et al. (2009). Supportive versus palliative care: what's in a name? A survey of medical oncologists and midlevel providers at a comprehensive cancer center. Cancer. Supportive Versus Palliative Care: What's in a Name? Many use the phrase "the patient has been taken off treatment" when chemotherapy has been discontinued, despite the fact that opioids are being titrated, medications are given for symptom management, and family needs are being addressed. This is the provision of supportive or palliative treatment. Fadul N, Elsayem A, Palmer JL, et al. (2009). Supportive versus palliative care: what's in a name? A survey of medical oncologists and midlevel providers at a comprehensive cancer center. Cancer. Supportive Versus Palliative Care: What's in a Name? When patients are given a choice between pursuing non-evidence based, unproven lifeprolonging interventions (frequently called treatments), or receiving only Palliative Care, they might opt for treatment only because they view any treatment as preferable to care. Fadul N, Elsayem A, Palmer JL, et al. (2009). Supportive versus palliative care: what's in a name? A survey of medical oncologists and midlevel providers at a comprehensive cancer center. Cancer. Supportive Versus Palliative Care: What's in a Name? Physicians & patients are more responsive to “hospice treatment” rather than end of life care. Fadul N, Elsayem A, Palmer JL, et al. (2009). Supportive versus palliative care: what's in a name? A survey of medical oncologists and midlevel providers at a comprehensive cancer center. Cancer. A.N.D. (Allow Natural Death) “If your heart stops, we are going to let you die peacefully.” “We will give you medicines to help make your breathing more comfortable.” These phrases truthfully communicate the care that clinicians have and prevents the patient/caregiver from feeling that ‘care has been withdrawn’ A.N.D. orders vs D.N.R. orders Perceptions can be everything Positive Supportive Non-abandonment Empathy Palliative Care an approach to care that improves quality of life of patients and their families facing life-threatening illness, through prevention, assessment, and treatment of pain and other physical, psychological, and spiritual problems. (WHO, 1982) Palliative Care: Supports the patient and family’s goals for the future, during whatever time they have remaining as well as their hopes for peace and dignity throughout the course of illness, the dying process, and death. Prevents and relieves suffering and promotes the best possible quality of life American Academy of Hospice and Palliative Medicine How do you attend to the thoughts and concerns of the dying when medicine has made it almost impossible to be sure who the dying even are? Is someone with terminal cancer, dementia, or incurable congestive heart failure dying, exactly? Atul Gawande MD, The New Yorker, August, 2, 2010 Prognosis Can Be Difficult to Predict Life Shortening Illness Actively Dying 120 CANCER 80 CHF 60 DEMENTIA 40 COPD 20 12 /1 10 /1 8/ 1 6/ 1 4/ 1 2/ 1 0 1/ 1 Function 100 Potential Goals of Care Cure of disease Avoidance of premature death Maintenance or improvement in function Prolong life Relief of suffering Quality of life Staying in control A good death Support for families and loved ones Palliative Care’s Place in the Course of Illness Diagnosis of Serious Illness Palliative Care Medicare Hospice Benefit DEATH Palliative Care Focuses on the patient and family preferences, not just on the patient’s disease process. Seriously ill people often feel as though they are lost among many specialists focused on body organs. > 5800 hospitals in the US – 2009 Over 1300 hospitals have palliative care programs. Palliative Care Services reduce hospital cost and length of stay; reduce utilization of critical care beds; improve care of patients near end of life; optimize symptom management. What Is Hospice? A program for patients who have a limited prognosis or life expectancy – Usually, 6 months or less Goals: Relief of pain and other symptoms Psycho-social support Benefit covered by medicare, medicaid, and most insurance companies at no cost to the patient. Hospice provides: Regular visits by nurse, hospice aide, & social worker to allow family to care for patient at home Volunteers, clergy – as desired Medications to manage pain and symptoms related to the terminal diagnosis Supplies, medical equipment, 24 hour RN and physician availability Hospice does not = morphine drip, or giving up Dr. Atul Gawande – surgeon and staff member of Brigham and Women’s Hospital and the Dana Farber Cancer Institute in Boston “Letting Go”, The New Yorker, August, 2, 2010 “Like many people, I had believed that hospice care hastens death, because patients forgo hospital treatments and are allowed high-dose narcotics to combat pain.” Hospice But studies suggest otherwise. A study of 4,493 Medicare patients with either terminal cancer or congestive heart failure, found no difference in survival time between hospice and non-hospice patients with breast cancer, prostate cancer, and colon cancer. Atul Gawande MD, The New Yorker, August, 2, 2010 Hospice Curiously, hospice care seemed to extend survival for some patients; those with pancreatic cancer gained an average of three weeks, those with lung cancer gained six weeks, & those with congestive heart failure gained three months. Atul Gawande MD, The New Yorker, August, 2, 2010 Hospice care goes where the patient is – home, assisted living, nursing home, inpatient unit 80% of hospice care takes place in the home An RN case manager is assigned to each patient to coordinate care and follow the patient’s and family’s goals for end of life. Hospice Care Provides: Patient & family control over decisions about care Anticipation of disease progression and preparation for patient decline Short term inpatient care for crises or respite Option for patient to die at home & be pronounced by an RN (without calling 911) Grief counseling for 1 year following patient’s death Conditions for Hospice Eligibility Under Medicare Order for certification of terminal illness and admission to hospice by patient’s attending physician and Hospice Medical Director Patient chooses hospice benefits rather than standard Medicare* Patient chooses palliation as goal, rather than cure Under Medicare, DNR status cannot be used as a requirement for admission *Patient may choose to revoke Hospice Care and revert to Cure-Oriented Care at any time Diseases with Coverage Guidelines indications of terminality Liver disease Renal disease ALS disease (Amyotrophic Lateral Sclerosis; Lou Gehrig's Disease ) HIV disease Heart disease Alzheimers & dementia Pulmonary disease Stroke and/or coma Adult failure to thrive Neurologic disorders Medicare requires recertification every 60 days to assess and document continued appropriateness for the hospice benefit. Benefits of Hospice Care Interdisciplinary, collaborative Cost-effective Extremely high patient and family satisfaction Improves quality of life Patients can revoke to pursue treatment or testing and then readmit, if desired Comparing Hospice vs. Palliative Care Hospice Services Patient population Patients with life-limiting illness; 6 months or less Sites of care • Home, NF, Assisted living, hospital, hospice inpatient unit Hospital-Based Palliative Care Services Patients at any stage of advanced or life-limiting illness; May continue with curative treatments Hospital; • outpatient or NF services varies by program - no home care services Comparing Hospice vs. Palliative Care Hospice Services Pain & symptom management, psychosocial, volunteer, spiritual, bereavement support Coordinated care delivered by IDT (physician, nurse, SW, clergy, aide, volunteer, pharmacist, therapist) Hospital-Based Palliative Care Service Pain & symptom management Services vary by program from a single MD to NP, SW, nurse, clergy, psychologist, counselors, therapy Comparing Hospice vs. Palliative Care Hospice Services Program reimbursed by medicare, medicaid, insurance Medications, supplies, durable medical equipment – provided at no cost to patient Family bereavement support for 1 year after death Palliative Care Services Physician consult is paid All other services are non-reimbursed Texas Palliative Care (TPC) The only palliative care service in east Texas Service began October, 2008 and is offered at Mother Frances Hospital and ETMC in Tyler Dr. Laura Ferguson, Dr. Thomas Beets, Dr. Keith Frazier, Dr. Craig Gunter – all board certified in Hospice and Palliative Medicine 80 new consults/month in hospital (roughly 3/day) HOET part-time RN, hospital social work and clergy ½ day clinic twice monthly (4 – 5 patients) primarily pain management Texas Palliative Care (TPC) Hospital consults 1. “having the talk” 2. concerns R/T life support (withholding or withdrawing) 3. medical futility, family insistence on care, family disagreement 4. pain and symptom management 5. medical evaluation regarding patient capacity TPC Hospital Consults 30-40% - 1 time consult resulting in agreement on withdrawal of life support (resulting in death or transfer to hospice) 30–40% - multiple MD or RN visits to discuss options, answer questions, provide emotional and psychosocial support -resulting in death or transfer to hospice 15-20% - multiple MD or RN visits resulting in transfer to skilled care (home health, nursing facility, rehab, or aggressive care) 2% - strictly pain and symptom management; followed in clinic TPC benefits Rate of hospital readmission has declined significantly on all patients consulted Decreased length of hospital stay, especially critical care + 50% of all consults enroll in a hospice program (reinforces the skill needed for end of life prognostication) Coping with Cancer Study NCI and Dana-Farber Cancer Institute October 2008 Patients who recalled having end of life talks with their physicians: were more likely to accept that their illness was terminal; preferred comfort care over life-extending therapies; received less aggressive medical treatment, such as resuscitation or admission to an intensive care unit; and enrolled earlier in hospice programs. Coping with Cancer Study More aggressive medical care was associated with worse patient quality of life and worse adjustment by patients' bereaved caregivers. Moreover, 6 months after the patients died, their family members were much less likely to experience persistent major depression. Excerpts from HOET family interviews “When the doctor told us it was time for hospice, I was surprised.” “I don’t know what I expected… that at the end, we would just disappear and arrive in heaven…. I never thought about it.” Our every impulse is to fight…. and we want choices, but, Hope is not a plan. Everyone Wants To Go To Heaven…. But Nobody Wants to Die