Thoracic wall and mediastinum pericardium and heart 27.09.2011
advertisement

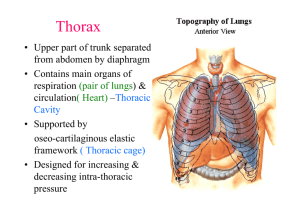
Salvador Dali - Anthropomorphic Chest of Drawers, 1936 Kaan Yücel M.D., Ph.D. 1 26. September 2011 Tuesday The thorax is the part of the body between the neck and abdomen. Posterior surface:: 12 thoracic vertebrae & posterior parts of the ribs Anterior surface: Sternum & costal cartilages Lateral surfaces: Ribs, separated from each other by the intercostal spaces 2 The floor of the thoracic cavity is deeply invaginated inferiorly by viscera of the abdominal cavity. 3 Regions Thoracic wall Thoracic cavity 4 The thorax includes the primary organs of the respiratory and cardiovascular systems. The thoracic cavity 3 major spaces Mediastinum – central compartment Right & left pulmonary cavities The majority of the thoracic cavity lungs Heart & structures involved in conducting the air and blood to and from the lungs +Esophagus 5 The true thoracic wall includes: • The thoracic cage and the muscles that extend between the ribs as well as the skin, subcutaneous tissue, muscles, and fascia covering its anterolateral aspect. • The mammary glands of the breasts lie within the subcutaneous tissue of the thoracic wall. 6 The domed shape of the thoracic cage provides its components enabling to: Protect vital thoracic and abdominal organs (most air or fluid filled) from external forces. Resist the negative (sub-atmospheric) internal pressures generated by the elastic recoil of the lungs and inspiratory movements. Provide attachment for and support the weight of the upper limbs. Provide the anchoring attachment (origin) of many of the muscles that move and maintain the position of the upper limbs relative to the trunk, as well as provide the attachments for muscles of the abdomen, neck, back, and respiration. The thorax is one of the most dynamic regions of the body. • 12 pairs of ribs and associated costal cartilages • 12 thoracic vertebrae and the intervertebral (IV) discs • Sternum Ribs & costal cartilages largest part of the thoracic cage Both are identified numerically, from the most superior (1st rib or costal cartilage) to the most inferior (12th). 8 Characteristic features of thoracic vertebrae • Bodies, vertebral arches, 7 processes for muscular & articular connections Costal facets (demifacets) on the vertebral bodies, inferior & superior pairs, articulation w/ the heads of the ribs Costal facets on the transverse processes articulation w/ the tubercles of the ribs, except inferior 2 or 3 Th vertebrae • Spinous processes 9 Ribs (L. costae) 12 pairs of curved, flat bones Form most of the thoracic cage 10 3 types of ribs True (vertebrocostal) ribs Carticalages’ direct connection w/ the sternum False (vertebrochondral) ribs Indirect connection with the sternum Cartilages’ connection w/ the superior rib Floating (vertebral, free ribs) No connection w/ the sternum VIIII- X XI-XIIII 11 Typical ribs (3rd to 9th) • Head Has two articular facets • articulate with numerically corresponding vertebra • articulate with one superior vertebra • Neck Connects the head with the body at the tubercle • Tubercle Between the shaft and the neck. Has an articular facet for articulating with the transverse process of the corresponding vertebra. • Body Concave internal surface has the costal groove for the intercostal nerve and vessels. Bears the angle. 12 13 Atypical ribs 1st, 2nd, and 10th-12th ribs are dissimilar. Costal cartilages prolong the ribs anteriorly and contribute to the elasticity of the thoracic wall, providing a flexible attachment for their anterior ends. 15 Intercostal spaces separate the ribs and their costal cartilages from one another. Named according to the rib forming the superior border of the space The 4th intercostal space lies between ribs 4 and 5. 11 intercostal spaces and 11 intercostal nerves 16 G. sternon, chest Has three parts: 1. Manubrium 2. Body 3. Xiphoid process Jugular notch @ sup. margin of the manubrium Level of T2 vertebra Clavicular notch 17 Sternal angle is formed by the junction of the manubrium with the body of the sternum. Lies at the level of 2nd costal cartilage anteriorly 18 While the thoracic cage provides a complete wall peripherally, it is open superiorly and inferiorly. The much smaller superior opening is a passageway that allows communication with the neck and upper limbs. The larger inferior opening provides the ring-like origin of the diaphragm, which completely occludes the opening. 19 Structures that pass between the thoracic cavity and the neck through the superior thoracic aperture: Trachea Esophagus Nerves, and vessels that supply and drain the head, neck, and upper limbs. 20 1. 2. 3. 4. 5. Costa transverse joints Sterno costal joint Costachondralis joint Intercondral Joints Sternal JointsManubrium, body, xiphoid process of the sternum. 21 22 Some muscles attached to and/or covering the thoracic cage are primarily involved in serving other regions. Several (axioappendicular) muscles extend from the thoracic cage (axial skeleton) to bones of the upper limb (appendicular skeleton). Muscles, such as sternocleidomasteoid muscle, abdominal muscles, pectoral muscles, function as accesory muscles of respiraton and work in forced respiration; when the person needs to breathe in and out more than usual; 100 meter sprinters, patients with respiratory problems. 23 Muscles of the thoracic wall Serratus posterior muscles Levator costarum muscles Intercostal muscles(External, internal and innermost) Subcostal muscle Transverse thoracic muscle These muscles either elevate or depress the ribs helping to increse the volume of the thoracic cavity. 24 The diaphragm is a shared wall (actually floor/ceiling) separating the thorax and abdomen. Although it has functions related to both compartments of the trunk, its most important (vital) function is serving as the primary muscle of inspiration. 25 26 27 In general, the pattern of vascular distribution in the thoracic wall reflects the structure of the thoracic cage—that is, it runs in the intercostal spaces, parallel to the ribs. 28 Arteries of Thoracic Wall Branches of the Thoracic aorta Subclavian artery Axillary artery 29 Arteries of Thoracic Wall The intercostal arteries course through the thoracic wall between the ribs. 30 Veins of Thoracic Wall Intercostal veins accompany the intercostal arteries & nerves Most superior in the costal grooves 11 posterior intercostal veins + 1 subcostal vein on each side. Posterior intercostal veins anastomose anterior intercostal veins Most posterior intercostal veins (4-11) end in the azygos/hemiazygos venous system SVC. 31 32 The 12 pairs of thoracic spinal nerves supply the thoracic wall. As soon as they leave the IV foramina in which they are formed, the mixed thoracic spinal nerves divide into anterior and posterior (primary) rami or branches. The anterior rami of nerves T1-T11 form the intercostal nerves that run along the extent of the intercostal spaces. 33 The intercostal nerves pass to and then continue to course in or just inferior to the costal grooves, running inferior to the intercostal arteries (which, in turn, run inferior to the intercostal veins). The neurovascular bundles (and especially the vessels) are thus sheltered by the inferior margins of the overlying rib. 34 35 The skin area supplied by a segment of the spinal cor.d 36 • The breasts (L. mammae) are the most prominent superficial structures in the anterior thoracic wall, especially in women. • Accessory to reproduction in women • Rudimentary and functionless in men, consisting of only a few small ducts or epithelial cords. • Mammary glands lie superficial to the pectoralis major muscle • The anterior part is called the nipple and it is surrounded by a circular pigmented area of skin, called the areola 37 Lymphatic drainage Axillary lymph nodes , Parasternal lymph nodes Abdominal lymph nodes 38 39 Arterial supply of the breast 1. Medial mammary branches 2.Lateral mammary branches, lateral thoracic & thoracoacromial arteries 3. Posterior intercostal arteries 2nd-4th 40 41 42 Venous drainage of the breast Mainly to the axillary vein, some to the internal thoracic vein 43 Nerves of the breast Anterior and lateral cutaneous branches of the 4th-6th intercostal nerves 44 45 The thoracic cavity is divided into three major spaces: The central compartment or mediastinum that houses the thoracic viscera except for the lungs and, on each side The right and left pulmonary cavities housing the lungs. 48 The mediastinum (Mod. L. middle septum, L, mediastinus, midway), occupied by the mass of tissue between the two pulmonary cavities, is the central compartment of the thoracic cavity. It is covered on each side by mediastinal pleura and contains all the thoracic viscera and structures except the lungs. •anterior mediastinum (1) •middle mediastinum (2) •posterior mediastinum (3) Mediastinum Superior to Inferior From superior thoracic aperture to the diaphragm Anterior to Posterior From sternum & costal cartilages to the bodies of the thoracic vertebrae The looseness of the connective tissue and the elasticity of the lungs and parietal pleura on each side of the mediastinum enable it to accommodate movement as well as volume and pressure changes in the thoracic cavity, for example, those resulting from movements of the diaphragm, thoracic wall, and tracheobronchial tree during respiration, contraction (beating) of the heart and pulsations of the great arteries, passage of ingested substances through the esophagus. Superior mediastinum Inferior mediastinum Superior mediastinum Superior to sternal angle Inferior mediastinum Inferior to sternal angle Further subdivided by the pericardium into anterior, middle, and posterior parts. Anterior mediastinum Between the anterior surface of pericardium and posterior surface of the sternum Middle mediastinum Pericardium, heart and beginings of the great vessels emerging from the heart lie here Posterior mediastinum Lies posterior to the pericardium and diaphragm 55 56 The pericardium and its contents (heart and roots of its great vessels) constitute the middle mediastinum. Some structures, such as the esophagus, pass vertically through the mediastinum and therefore lie in more than one mediastinal compartment. Contents of the superior mediastinum 1) Thymus 2) Great vessels related to the heart with the veins 3) Inferior continuation of the cervical viscera (trachea anteriorly and esophagus posteriorly) and related nerves (left recurrent laryngeal nerve) 4) Thoracic duct and lymphatic trunks 5) Prevertebral muscles 60 The posterior mediastinum The posterior mediastinum (the posterior part of the inferior mediastinum) is located inferior to the sternal angle, posterior to the pericardium and diaphragm, between the parietal pleura of the two lungs. Contents of the posterior mediastinum Thoracic aorta Thoracic duct Posterior mediastinal lymph nodes Azygos and hemiazygos veins Esophagus Esophageal nerve plexus Thoracic sympathetic trunks Thoracic splanchnic nerves HEART & PERICARDIUM HEART • Slightly larger than a clenched fist • A double, self-adjusting suction and pressure pump • Propel blood to all parts of the body The right side of the heart (right heart) receives poorly oxygenated (venous) blood from the body through the superior vena cava (SVC) and inferior vena cava (IVC) and pumps it through the pulmonary trunk and arteries to the lungs for oxygenation. The left side of the heart (left heart) receives well-oxygenated (arterial) blood from the lungs through the pulmonary veins and pumps it into the aorta for distribution to the body. The heart has four chambers: Right & Left atria Right & Left ventricles The atria are receiving chambers that pump blood into the ventricles (the discharging chambers). The synchronous pumping actions of the heart's two atrioventricular (AV) pumps (right and left chambers) constitute the cardiac cycle. The cycle begins with a period of ventricular elongation and filling (diastole) and ends with a period of ventricular shortening and emptying (systole). The wall of each heart chamber consists of three layers: • Endocardium, a thin internal layer or lining membrane of the heart that also covers its valves. • Myocardium, a thick, helical middle layer composed of cardiac muscle. The walls of the heart consist mostly of myocardium, especially in the ventricles. • Epicardium, a thin external layer (mesothelium) formed by the visceral layer of serous pericardium. Externally, the atria are demarcated from the ventricles by the coronary sulcus (atrioventricular groove), and the right and left ventricles are demarcated from each other by anterior and posterior interventricular (IV) sulci (grooves). The heart appears trapezoidal from an anterior or posterior view, but in three dimensions it is shaped like a tipped-over pyramid with its apex (directed anteriorly and to the left), a base (opposite the apex, facing mostly posteriorly), and four sides. The four surfaces of the heart Anterior (sternocostal) surface Diaphragmatic (inferior) surface Right pulmonary surface Left pulmonary surface Anterior (sternocostal) surface Diaphragmatic (inferior) surface 74 Right atrium • Forms the right border of the heart and receives venous blood from the SVC, IVC, and coronary sinus. • The ear-like right auricle is a conical muscular pouch that projects from this chamber like an add-on room, increasing the capacity of the atrium as it overlaps the ascending aorta. 76 • The interior of the right atrium has a smooth, thin-walled, posterior part (the sinus venarum) on which the venae cavae (SVC and IVC) and coronary sinus open, bringing poorly oxygenated blood into the heart. • Rough, muscular anterior wall composed of pectinate muscles (L. musculi pectinati). The interatrial septum separating the atria has an oval, thumbprintsize depression, the oval fossa (L. fossa ovalis), a remnant of the oval foramen (L. foramen ovale) and its valve in the fetus. 80 • Forms the largest part of the anterior surface of the heart, a small part of the diaphragmatic surface, and almost the entire inferior border of the heart. • The right ventricle receives blood from the right atrium through the right AV (tricuspid) orifice. Tendinous cords (L. chordae tendineae) attach to the free edges and ventricular surfaces of the anterior, posterior, and septal cusps, much like the cords attaching to a parachute. • The tendinous cords arise from the apices of papillary muscles, which are conical muscular projections with bases attached to the ventricular wall. • The papillary muscles begin to contract before contraction of the right ventricle, tightening the tendinous cords and drawing the cusps together. The interventricular septum (IVS), is obliquely placed partition between the right and left ventricles The left atrium forms most of the base of the heart. The valveless pairs of right and left pulmonary veins enter the atrium. The tubular, muscular left auricle, its wall trabeculated with pectinate muscles, forms the superior part of the left border of the heart. A semilunar depression in the interatrial septum indicates the floor of the oval fossa; the surrounding ridge is the valve of the oval fossa (L. valvulae foramen ovale). The interior of the left atrium has: Pectinate muscles Four pulmonary veins (two superior and two inferior) An interatrial septum A left AV orifice through which the left atrium discharges the oxygenated blood it receives from the pulmonary veins into the left ventricle. A semilunar depression in the interatrial septum indicates the floor of the oval fossa; the surrounding ridge is the valve of the oval fossa (L. valvulae foramen ovale). The left ventricle forms the apex of the heart, nearly all its left (pulmonary) surface and border, and most of the diaphragmatic surface. Because arterial pressure is much higher in the systemic than in the pulmonary circulation, the left ventricle performs more work than the right ventricle. The interior of the left ventricle has: A smooth-walled, non-muscular, superoanterior outflow part, the aortic vestibule, leading to the aortic orifice and aortic valve. A double-leaflet mitral valve that guards the left AV orifice. The mitral valve has two cusps. The semilunar aortic valve, between the left ventricle and the ascending aorta, is obliquely placed. 93 94 Vasculature of the Heart The blood vessels of the heart • Comprise the coronary arteries and cardiac veins, which carry blood to and from most of the myocardium. Coronary Arteries • • • The first branches of the aorta Supply the myocardium and epicardium. Supply both the atria and the ventricles. The right and left coronary arteries arise from aorta. Anastomoses between the branches of the coronary arteries exist, which enables the development of the collateral circulation. Veins of the heart The heart is drained mainly by veins that empty into the coronary sinus and partly by small veins that empty into the right atrium. Veins of the heart • All of the veins (except the smallest cardiac veins) open into the coronary sinus, which runs on the posterior part of the coronary groove . • Coronary sinus opens into the right atrium at the opening of the coronary sinus. Lymphatic Drainage of the Heart • A single lymphatic vessel, formed by the union of various lymphatic vessels from the heart ends in the inferior tracheobronchial lymph nodes, usually on the right side. Stimulating and Conducting System of the Heart The conducting system consists of nodal tissue that initiates the heartbeat and coordinates contractions of the four heart chambers, and highly specialized conducting fibers for conducting them rapidly to the different areas of the heart. The impulses are then propagated by the cardiac striated muscle cells so that the chamber walls contract simultaneously. . 103 Impulse generation and conduction can be summarized as follows: The SA node (pacemaker of the heart; in the right atrium) initiates an impulse that is rapidly conducted to cardiac muscle fibers in the atria, causing them to contract. The impulse spreads by myogenic conduction, which rapidly transmits the impulse from the SA node to the AV node (in the right atrium). The signal is distributed from the AV node through the AV bundle and its branches (the right and left bundles), which pass on each side of the IVS to supply subendocardial branches to the papillary muscles and the walls of the ventricles. Innervation of the Heart Innervation of the heart is through the autonomic nerves (both sympathetic and parasympathetics) from the cardiac plexus. PERICARDIUM The pericardium is a fibroserous membrane that covers the heart and the beginning of its great vessels. The pericardium is a closed sac composed of two layers: –Fibrous pericardium (external) continuous with the central tendon of the diaphragm – Serous pericardium (internal) • Parietal layer • Visceral layer (epicardium) Visceral and parietal layers are continuous with each other where the great vessels enter and leave the heart. 111 The fibrous pericardium is continuous superiorly with the tunica adventitia of the great vessels entering and leaving the heart and with the pretracheal layer of deep cervical fascia. • Attached anteriorly to the sternum by the sternopericardial ligaments • Continuous inferiorly with the central tendon of the diaphragm as the pericardiacophrenic ligament Inner surface is lined by the parietal layer of the serous pericardium and these layers are strictly attached to each other. The fibrous pericardium protects the heart against sudden overfilling because it is so unyielding and closely related to the great vessels that pierce it superiorly. Pericardial cavity Potential space between opposing layers of the parietal and visceral layers of serous pericardium. Contains a thin film of fluid that enables the heart to move and beat in a frictionless environment. Transverse pericardial sinus Oblique pericardial sinus The arterial supply of the pericardium is mainly from a slender branch of the internal thoracic artery, the pericardiacophrenic artery. The venous drainage of the pericardium is from the pericardiacophrenic veins, tributaries of the brachiocephalic (or internal thoracic) veins and variable tributaries of the azygos venous system. pericardiacophrenic artery