Prehospital Management of Hypothermia in the
advertisement

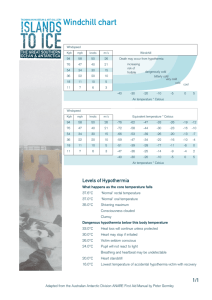
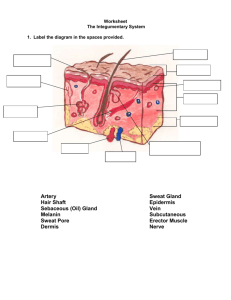
Disorders of Temperature Regulation Bryan E. Bledsoe, FACEP Midlothian, TX Temperature Regulation Hypothermia Hyperthermia Heat Cramps Heat Tetany Heat Exhaustion Heat Syncope Heat Stroke Fever Temperature Regulation Humans are warm-blooded mammals who maintain a constant body temperature (euthermia). Temperature Regulation Temperature regulation is controlled by the hypothalamus in the base of the brain. Temperature Regulation The hypothalamus functions as a thermostat for the body. Temperature receptors (thermoreceptors) are located in the skin, certain mucous membranes, and in the deeper tissues of the body. Temperature Regulation When an increase in body temperature is detected, the hypothalamus shuts off body mechanisms that generate heat (for example, shivering). When a decrease in body temperature is detected, the hypothalamus shuts off body mechanisms designed to cool the body (for example, sweating). Temperature Regulation Body Temperature = Thermogenesis–Heat Loss Temperature Regulation Basal The Metabolic Rate: metabolism that occurs when the body is completely at rest. Temperature Regulation Metabolic The Rate: body continuously adjusts the metabolic rate in order to maintain a constant CORE temperature. Temperature Regulation Normal body temperature is approximately 37º C (98.6º F). However, what is normal for an individual may vary somewhat. Hypothermia Definition of Hypothermia: CLASSIC DEFINITION: A state of low body temperature, specifically a low CORE temperature (< 35º C or < 95º F). ALTERNATIVE DEFINITION: It is best defined as the unintentional decrease of around 2º C (3.6º F) from the “normal” CORE temperature Hypothermia What is the CORE temperature? The deep internal temperature of normothermic humans. Hypothermia How is the CORE temperature measured? There is little variance in CORE temperature because of perfusion. Esophageal and tympanic temperatures are essentially the same as the temperature of the pulmonary artery. Hypothermia In steady-state conditions, the rectal temperature is a good index of CORE temperature. Hypothermia Oral temperature is an excellent index of CORE temperature, provided the mouth is kept closed. Hypothermia The type of temperature measurement utilized is less important than using the same device and measurement site to detect trends. Thermometer must be able to read low temperatures. Hypothermia Heat loss results from: Conduction Convection Radiation Evaporation Respiration Heat = Molecular Motion Hypothermia Conduction: Heat loss occurs due to direct contact of the body with a cooler object. Heat flows from higher temperature matter to lower temperature matter. Hypothermia Convection: Heat loss occurs due to air currents passing over the body. Heat must first be conducted to the air before convection can occur. Hypothermia Radiation: Heat loss results from infrared rays. All objects not at absolute zero will radiate heat to the atmosphere. Radiation Radiation Hypothermia Evaporation: Heat loss occurs as water evaporates from the skin. Heat loss occurs as water evaporates from the lungs during respiration. Hypothermia Respiration: Respiration combines the heat loss mechanisms of convection, radiation, and evaporation. Expired air is normally 98.6 degrees F. and 100% humidified. Heat-conserving Mechanisms Vasoconstriction of blood vessels in the skin. Stimulated through activation of the sympathetic nervous system. Causes pale, cool skin. Heat-conserving Mechanisms Piloerection is more commonly called “goose bumps” or “goose flesh.” Evolutionary remnant. Caused by sympathetic stimulation of arrector pili muscles. Heat-conserving Mechanisms Increased heat production: Shivering Activation of futile cycles (chemical thermogenesis) Increased thyroxine release Hypothermia When the core temperature of the body drops below 95º F, an individual is considered to be hypothermic. Hypothermia Clinically, hypothermia results from: Inadequate heat generation by the body (thermogenesis). Excessive cold stress. A combination of both. Hypothermia Normal Range: 96-100º F Mild Hypothermia: 90-95º F Severe Hypothermia < 90º F Hypothermia Predisposing Factors to Hypothermia: Patient Age Patient Health Medications Prolonged or Intense Exposure Co-existing Weather Conditions Hypothermia Patient Age: Pediatric and geriatric patients cannot tolerate cold environments and have less capacity for heat generation. Older patients often become hypothermic in environments that seem only mildly cool to others. Hypothermia Patient Health: Hypothyroidism (suppresses metabolic rate) Malnutrition, hypoglycemia, Parkinson’s disease, fatigue, and other medical conditions can interfere with the body’s ability to combat cold exposure. Hypothermia Medications: Some drugs interfere with the body’s heat-generating mechanisms. These include: narcotics, alcohol, antihistamines, antipsychotics, antidepressants, and many others. Hypothermia Prolonged The or Intense Exposure: length and severity of cold exposure have a direct effect on morbidity and mortality. The Wind Chill Index (WCI) must be taken into consideration. Hypothermia Coexisting Weather Conditions: High humidity, brisk winds, accompanying rain can all magnify the effect of cold exposure on the body by accelerating heat loss from the skin. Hypothermia Degrees Mild– of Hypothermia: Core temperature > 90 degrees F (32 degrees C) Severe– Core temperature < 90 degrees F (32 degrees C) Signs and Symptoms MILD Hypothermia: Lethargy Shivering Lack of Coordination Pale, cold, dry skin Early rise in blood pressure, heart, and respiratory rates. Signs and Symptoms SEVERE No Hypothermia: shivering Heart rhythm problems Cardiac arrest Loss of voluntary muscle control Low blood pressure Undetectable pulse and respirations Prevention Preventive Warm Measures: dress Plenty of rest Adequate diet Limit Exposure Treatment Treatment for Hypothermia: 1. Remove wet garments 2. Protect against further heat loss and wind chill. 3. Maintain patient in horizontal position. Treatment Treatment for Hypothermia: 4. Avoid rough handling. 5. Monitor the core temperature. 6. Monitor the cardiac rhythm. Treatment ECG changes seen in hypothermia: Prolongation of first the PR interval, then the QRS, then the QTc interval. J waves (also called Osborne waves) can occur at any temperature < 32.3º C (90º F). Most frequently seen in Leads II and V6. The size of the J waves increase with temperature depression. “J” or Osborne Waves “J” or Osborne Waves “J” or Osborne Waves Rewarming Methods Active of Rewarming: External Rewarming Active Internal Rewarming Rewarming Active Rewarming of MILD Hypothermia: Active external methods: Warm blankets Heat packs Warm water immersion (with caution) Active internal methods: Warmed IV fluids Rewarming Active Rewarming of SEVERE Hypothermia: Active external methods: Warm blankets Heat packs Warm water immersion (with caution) Active internal methods: Warmed IV fluids Warmed, humidified oxygen Rewarming Rewarming of the SEVERE hypothermia patient is best carried out in the Emergency Department using a pre-defined protocol, unless travel time exceeds 15 minutes. Most patients who die during active rewarming die from ventricular fibrillation. Rewarming Application of external heat in the prehospital setting is usually not effective and not recommended because: More heat transferrence is required than generally possible in the prehospital setting. Application of external heat may cause “rewarming shock.” Rewarming Rewarming Shock: Occurs due to peripheral reflex vasodilation. Causes the return of cooled blood and metabolic acids from the extremities. May cause a paradoxical afterdrop in the core temperature further worsening hypothermia. Rewarming Rewarming Can Shock: be prevented in the prehospital setting by using warmed IV fluids during active rewarming. Rewarming Portable IV fluid heaters are available in the United States and Canada. Devices fit in-line and are powered by DC power sources. Rewarming The device is single-use and remains with the patient in the hospital (both the ED and on the floor). Rewarming The HOT IV is powered from a Physio-Control battery or from a DC converter plugged in to an AC outlet. Issues in Hypothermia Benefits of IV Fluid Warming: Maintains euthermia Increases patient comfort Prevents shivering Issues in Hypothermia Benefits of IV Fluid Warming: Prevents cold-induced dysrhythmias Decreases hemorrhage in abdominal trauma patients Decreases the incidence of infectious complications in abdominal trauma patients Issues in Hypothermia Benefits Allows of IV Fluid Warming: active internal rewarming to begin in the prehospital setting. Less labor-intensive, freeing emergency personnel to manage other, more pressing care needs. Cardiac Arrest Other Clinical Concerns: Resuscitation of cardiac arrest due to hypothermia is only successful when the patient is being re-warmed. The hypothermic cardiac arrest patient is not DEAD until he is WARM and DEAD! Survival from Hypothermia 48.2º F (9º C) - Lowest reported survivor from therapeutic exposure. 59.2º F (15.2º C) – Lowest reported infant survival from accidental exposure. 60.8º F (16º C) – Lowest reported adult survival from accidental exposure. Survival from Hypothermia 64.4º F (18º C) – Asystole. 66.2º F (19º C) – Flat EEG. 71.6º F (22º C) – Maximum risk for ventricular fibrillation. 77º F (25º C) – Cerebral blood flow decreased by 66%. 78.8º F (26º C) – No reflexes or response to painful stimuli. Issues in Hypothermia Other Clinical Concerns: Hypothermia is common, even in persons with minor trauma. Hypothermia can worsen infectious complications of abdominal trauma. Hypothermic trauma patients suffer increased blood loss compared to their normothermic cohorts. Issues in Hypothermia Considerations in Emergency Care: “Most traditional methods of maintaining trauma patient temperature during prehospital transport appear to be inadequate.” From: Watts DD, Roche M, et al. The utility of traditional prehospital interventions in maintaining thermostasis. Prehosp Emerg Care 1999;3(2)115-122 Issues in Hypothermia Considerations in Emergency Care: “Based upon our findings, accidental hypothermia poses a relevant problem in the prehospital treatment of trauma patients. It is not limited to a special season of the year.” From: Helm M, Lampl L, Hauke J, Bock KH. Accidental hypothermia in trauma patients. Is it relevant to preclinical emergency treatment? Anaesthesist 1995;44(2):101-107 Issues in Hypothermia Considerations in Emergency Care: “Thus, hypothermia is common in patients undergoing a laparotomy for trauma. Hypothermic patients with similar injury severity have greater blood loss.” From: Bernabei AF, Levision MA, Bender JS. The effects of hypothermia and injury severity on blood loss during trauma laparotomy. J Trauma 1992;33(6):835-839 Hyperthermia Heat cramps Heat tetany Heat exhaustion Heat syncope Heat stroke Hyperthermia Abnormal elevation in body temperature. Not a normal physiological response (such as fever). Hyperthermia Caused by environmental temperature increase. Increased humidity. Still air. Hyperthermia Heat waves not uncommon. More devastating where heat waves are uncommon. 600 heat-related deaths in 1995 Chicago heat wave. Heat Cramps Brief, painful muscle contractions. Frequent complication of heat exhaustion. Salt depletion and other electrolyte problems commonly associated. Self-limited. Symptomatic treatment. Heat Tetany Carpopedal spasms that occur in hot environments. Secondary to hyperventilation from body’s attempt to cool. Resolves when hyperventilation slows. Heat Exhaustion Results from cardiovascular strain as body attempts to maintain normal temperature. Usually develops and continues over several days. Heat Exhaustion Most common between body temperature of 102.9° (39.4° C) and 104° (40° C). Finding is unreliable. Diagnosis should be made on physical assessment. Heat Exhaustion Firefighters at increased risk of developing heat exhaustion. Rehab sector essential for major fires in warm weather. Heat Exhaustion Symptoms: Dizziness Headache Fatigue Irritability Anxiety Chills Nausea/vomiting Heat cramps Heat Exhaustion Signs: Tachycardia Hyperventilation Hypotension Syncope Heat Exhaustion Treatment: Remove patient from warm environment. Remove bulky clothing. Fluids (IV or PO). Antiemetics Removal from duty. Heat Syncope Form of postural hypotension. Results from massive vasodilation. Dehydration usually a contributing factor. Most common in persons not acclimatized to the heat. Usually occurs during the early stages of heat exposure. Heat Syncope Treatment: Symptomatic Cool Fluids Rule out other causes of syncope. Heat Stroke Heat stroke is a life-threatening emergency! Heat stroke is a total failure of temperature regulation. Heat Stroke Core temperature >104.9° (40.5° C). Loss of sweating (anhidrosis). Altered mental status. Heat Stroke Anhidrosis may or may not be present. Just because a patient is sweating does not mean they are not suffering heat stroke. Heat Stroke Treatment must include: CPR if required. Fluid and electrolyte replacement. Immediate cooling. Heat Stroke Goal of cooling is to get body temperature down to 104° (40° C). Preferred method is immersion in cold water or ice-water bath. Evaporative cooling (moistened sheets) and ice packs) can be used but less effective. Essential to remove from bath as soon as target temperature reached to avoid overcooling and activation of reflex mechanisms. Fever Fever Fever is not an abnormal increase in body temperature. It is a resetting of the body’s set-point above normal. Causes: Abnormalities within the brain (tumors, hemorrhage compress hypothalamus) Dehydration Toxic substances within the body (pyrogens). Fever Definitions: Any oral temp ≥ 98.9° (37.2° C) in the early morning. Any oral temp ≥ 100° (37.8° C) at any time. Fever How hot is high? Human upper limit of fever is 105.8107.6°F (41–42°C). Almost never exceeds 42° C unless there’s a failure in thermoregulation. Fever How hot is high? 104° (40° C) may be the upper limit of fever in infants <12 weeks old. Remember that young infants can have infections with normal or lowered body temps. Fever Can high fever can cause damage in and of itself? Seizures and complications. Brain damage because of the infection causing the fever (meningitis or encephalitis). Fever No human studies published. Animal studies suggest that a body temp of ≥ 107.5° (42° C) in humans may trigger enough adverse effects on a cellular level to cause death. Fever Animal studies: Temperature >105° may cause respiratory alkalosis and occasional electrolyte imbalances Temperature >105.8° may cause cellular swelling and damage in the brain, kidneys and liver Fever When set-point in hypothalamus changes, it usually takes several hours to reach new set-point. Signs and symptoms common during this phase (blood temperature lower than hypothalamic set-point). Fever Fever is generally uncomfortable. Signs and Symptoms: Chills Flushing of the skin Teeth chattering Feels cold Shivering Skin cold to touch (phase-dependent) Fever It is important to remember that fever is a normal response to many diseases. Although uncomfortable, it is rarely harmful. Febrile Seizures Incidence of 2-5% in US. 6 months – 3 years (median 18-22 months). Boys more often than girls. Often occurs with the first fever of an illness. Febrile Seizures Characteristics: 85% of all febrile seizures last for <15 minutes and don’t recur within 24 hours. 50% have temp between 39°-40°C. 25% have temp > 40°C. Febrile Seizures: Characteristics: 1/3 will have recurrence of febrile seizures. The younger the age at 1st febrile seizure, the higher the incidence of recurrence. El-Radhi, 1998 Presenting temp <39° for 1st febrile seizure have 2.5x risk for recurrence within the same illness and 3x risk for recurrence with other illnesses Febrile Seizures Simple febrile seizures are generalized tonicclonic with brief post-ictal period. Complex or atypical febrile seizures can be focal, atonic, or prolonged Febrile Seizures Multiple studies have revealed several genetic loci that code for susceptibility to febrile seizures. Febrile Seizures Fever + Seizure ≠ “Febrile Seizure” Meningitis/Sepsis Seizure disorder Medication/Poison-induced Febrile Seizure is NOT an EMS diagnosis! Febrile Seizure Myths: Rate of temperature rise does not appear to be a cause of febrile seizures. No studies have demonstrated that febrile seizures without complicating hypoxia cause brain damage. Febrile Seizures Myths: Febrile Risk If seizures cause epilepsy. factors for afebrile seizure: Complex 1st Febrile Seizure. Abnormal neuro state before 1st Febrile Seizure. Afebrile seizure history in parents or siblings >2 risk factors, 10% chance of developing “epilepsy” Febrile Seizures Myths: Treating the fever will prevent the seizure. Antipyretics are not protective. Rectal/oral diazepam at time of fever is protective. Daily oral phenobarbital is protective but has undesirable side effects. Febrile Seizures There is no evidence that bringing the fever down by any means will stop or prevent a febrile seizure. Febrile Seizures Bottom line: They’re more scary than dangerous. Most resolve without anticonvulsant treatment. Antipyretic treatment does not prevent or treat febrile seizures. Not all seizures with fever are febrile seizures. Fever Fever treatment: Treatment of choice is antipyretics (acetaminophen, ibuproprofen). Fever There is no evidence to support one antipyretic over another when considering effectiveness No delivery route (po/pr) has been proven more effective than another, but there has been recent evidence to suggest that higher doses may be needed when given rectally. Fever Acetaminophen 10-15 mg/kg po/pr q4h. Ibuprofen 10mg/kg po q6-8h. No demonstrated benefit to alternating the two meds but there is a significant chance of dosing error and possible overdose. Fever Other cooling methods: Never use ice, cold water or alcohol. Use tepid water or cool compresses over head and pulse points. Avoid inducing chills. Fever Should we treat fever? Animal studies suggest that the fever mechanism is a positive adaptive response Triggers host immune responses May stabilize cell membranes Fever Should we treat fever? Increased metabolic stress and oxygen demand: Patients with poor cardiac reserve Patients with poor pulmonary reserve Lowers the “seizure threshold” Fever Reasons Patient to treat fever: comfort Parent comfort Fever Should EMS providers treat fever? Fever Should EMS providers treat fever? Pros: Providing an additional service to our customers. Comfort measure. Cons: Treat and release? Documentation of fever. Dosing of meds. Reinforcement of fears. Fever Cultural considerations. Relates to ancient beliefs of “hot” and “cold” illnesses. Fever Summary: Fever is not the clearly defined concept many believe it to be. Both the lay public and the medical community need more education about fever. “Fever Phobia” is unfounded. Fever treatment by EMS personnel is controversial. Temperature Regulation For more detailed information on temperature regulation and hypothermia, see the March 2003 issue of JEMS magazine.