MacmillanGISymptomsinpalliativecare211009
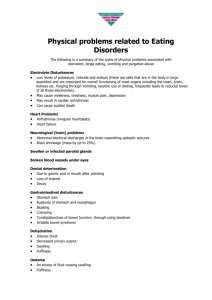
advertisement

Gastrointestinal Symptoms in Palliative Care Dr Peter Nightingale Macmillan GP Introduction Nausea and vomiting reported by 40-70% Constipation Dry reported by 50% of hospice inpatients mouth reported by over 75% Overview Nausea and vomiting Pathways and receptors Evaluation Causes Receptor-specific anti-emetics Malignant intestinal obstruction Causes Clinical features management Overview Constipation Causes Associated symptoms Management/laxative guidance Mouth Dry care mouth Oral candidiasis Nausea and Vomiting Which of the following is true? A Cyclizine and metoclopramide is a logical combination of drugs B Steroids are unhelpful in malignant bowel dysfunction C Cyclizine and Haloperidol is a powerful combination of antiemetics D Metoclopramide can help colicy pain in malignant bowel dysfunction Definitions Nausea A feeling of the need to vomit May be accompanied by autonomic symptoms Retching Rhythmic, laboured, spasmodic movements of the diaphragm and abdominal muscles Vomiting Forceful expulsion of gastric contents through the mouth Table 2 Mechanism of action of drugs used in the treatment of nausea and vomiting 1 2 Class Drug Dopamine 2 receptor antagonist Metoclopramide Domperidone Haloperidol 5-Hydroxytryptamine 3 antagonist Ondansetron Granisetron Antihistaminic antimuscarinic Cyclizine Dopamine 2 antagonist, antihistaminic, antimuscarinic, 5-hydroxytryptamine 2 antagonist Levomepromazine Antimuscarinic Hyoscine hydrobromide Benzodiazepine Lorazepam Cannabinoid Nabilone Corticosteroid Dexamethasone Prokinetic 5-hydroxytryptamine 4, D2 Metoclopramide Domperidone Antisecretory Antimuscarinic Hyoscine butylbromide Glycopyrronium Somatostatin analogue Octreotide Evaluation Establish a likely cause Examination Thorough review of medication-do they need a PPI?(most do) Check bloods where appropriate Treat anything reversible Non-drug measures Set realistic goals Identify the most likely pathway and receptors involved Evaluation Choose the most potent antagonist Choose the most appropriate route of administration Opt for regular rather than PRN dosing Titrate the drug dose accordingly Review regularly: Have you identified the cause correctly? Consider combined therapy Causes of Nausea and Vomiting Chemical Drugs e.g. opioids Metabolic disturbance Calcium and urea Gastrointestinal Gastric stasis Stretch/distortion of GI tract ?correctable bowel obstruction Cranial Elevated ICP Meningeal irritation Skull mets Other XRT Anticipatory and anxiety Movement Cough Is a prokinetic (e.g.metoclopramide 10-20mg tds) indicated? Promote gastric emptying Useful in gastric stasis (large volume vomits-late in day-undigested food-little nausea-hiccoughs) If not settling in 2 or 3 days or happening 2-3 times daily consider using a syringe driver Is vomiting due to opioids or chemical/metabolic factors? Haloperidol 1.5mg is drug of choice for opioid induced vomiting (can usually be stopped after 1014 days) Some patients develop secondary gastric stasis so metoclopramide helps. Alternative opioid indicated if nausea persists Haloperidol 1.5-3mg is indicated for uraemia or hypercalcaemia Is the patient still vomiting? With vomiting more than 2-3 times daily then consider a syringe driver. Cyclizine (25-50mg tds) is broad spectrum but can cause drowsiness and a dry mouth. Haloperidol and cyclizine is a potent combination Avoid cyclizine and metoclopramide (they oppose each others action) Levomepromazine 3-25mg acts at multiple sites and is sedating at higher doses. Dexamethasone 8mg daily has an anti emetic activity Summary Points Establish a cause Reverse anything reversible Choose the most appropriate receptor antagonist Choose the most appropriate route of administration Review regularly Malignant Intestinal Obstruction Incidence and Prognosis Rates of up to 42% reported in ovarian cancer Survival for several months without surgical intervention is possible Causes of Obstruction Organic (mechanical) Intraluminal Intramural Extramural May be multiple sites of obstruction Functional (pseudo-obstruction) Mesenteric or bowel muscle infiltration Coeliac plexus infiltration Clinical Features Depends on level of obstruction Usually insidious onset Complete or partial (sub-acute) Difficult to distinguish in practice Abdominal Constant Colic pain background Clinical Features Vomiting +/- nausea Abdominal distension Absolute constipation Diarrhoea Borborygmi, normal or absent bowel sounds Management Try to anticipate and plan treatment in advance Surgical intervention should be considered in all patients Radiological investigations To distinguish between severe constipation and obstruction In patients considered for surgery Medical Management Appropriate drug regimen can provide excellent symptom relief CSCI is route of choice for most drugs IV fluids, NG tubes rarely needed Allow to eat and drink little and often Good mouth care vital Realistic goals Pain Background pain Opioids Colic May be relieved by opioids Most need antispasmodic Hyoscine butylbromide 20mg stat and PRN Hyoscine butylbromide 60-120mg/24hr Also has an antisecretory action Nausea and Vomiting If no colic and passing flatus try prokinetic Metoclopramide 40-100mg/24hr Stop if develop colic If patient has colic prokinetics are contraindicated Cyclizine +/- haloperidol Somatostatin Analogues Octreotide inhibits secretion of numerous hormones Resultant reduction in volume of GI secretions More rapidly effective than hyoscine Duration of action 8 hours Administer via CSCI or SC bolus Side effects: dry mouth and flatulence Laxatives Stop stimulant, osmotic or bulk-forming laxatives If likely to be constipated try phosphate enema and a softener e.g. docusate sodium 100-200mg bd Corticosteroids Cochrane review 1999 (Feuer and Broadley) May relieve peri-tumour oedema Resultant improvement in symptom control Trial of dexamethasone 8mg daily SC Review after 5-7 days Stop or reduce dose according to response Gastroduodenal Obstruction Duodenum Often caused by pancreatic tumour Usually functional Try metoclopramide first Pylorus Antisecretory drugs mainstay of treatment Steroids Consider NGT or venting gastrostomy Constipation Definitions The passage of small, hard faeces infrequently and with difficulty The passage of hard stools less frequently than the patient’s own normal pattern Prevalence in Palliative Care A frequent cause of distress in terminally ill patients 50% of patients admitted to Palliative Care Units report constipation 80% require laxatives 90% of terminally ill patients on opioid analgesics are constipated Physiology Food residue usually in the small bowel for 1-2hr and in the colon for 2-3 days In constipated patients colonic transit can be greatly prolonged (4-12 days) Most of the colon’s action is mixing Forward movement 6x/day The frequency and strength of peristaltic contractions are influenced by meals and activity Causes of Constipation Cancer e.g. hypercalcaemia, intraabdominal disease Debility Weakness Immobility Poor nutrition Treatment Concurrent disease Drugs e.g. opioids, anticholinergics e.g. anal fissure Neurological disease Immobility Loss of rectal sensation and anal tone Effects of Opioids Increased sphincter tone Suppress forward peristalsis Increase water and electrolyte absorption in the small and large bowel Impaired defaecation reflex Associated Symptoms Flatulence Bloating Abdominal pain Feeling of incomplete evacuation Anorexia Overflow diarrhoea Confusion Nausea and vomiting Urinary dysfunction Restlessness Can mimic bowel obstruction by tumour Assessment and Examination Pattern of bowel movements Access to toilet, etc Halitosis Faecal leak Confusion Abdominal distension Visible peristalsis Palpable colon PR / stomal examination Management Prevention is better than waiting until intervention is needed The aim is to achieve comfortable defaecation rather than any particular frequency and without the need for enemas or suppositories General Measures Diet Increase fluid intake Privacy Commode rather than bed-pan Mobilise if possible Stop or reduce constipating drugs where possible Oral Laxatives Softeners Surfactants/wetting 1-3 days latency Osmotic 3 agents e.g. docusate, poloxamer laxatives e.g. lactulose, Movicol day latency Lactulose: bloating, colic and flatulence Need to increase fluid intake Movicol better tolerated and more effective Oral Laxatives Softeners Bulk-forming Stool agents e.g. Fybogel, Normacol normalisers Large fluid intake required Can exacerbate constipation in the terminally ill and those on opioids Oral Laxatives Stimulants e.g. senna, bisacodyl, danthron, sodium picosulphate Induce peristalsis 6-12 hr latency Can cause colic and severe purgation Especially useful in opioid induced constipation Oral Laxatives Combinations More effective and better tolerated than either alone for opioid induced constipation Codanthramer = poloxamer + danthron Codanthrusate = docusate + danthron Discolouration of urine with danthron and may cause a rash Equivalent Doses (Regnard, 1995) 3 codanthrusate capsules 15ml codanthrusate suspension 6 codanthramer capsules 4 codanthramer strong capsules 30ml codanthramer suspension 10ml codanthramer strong suspension 2 senna tabs + 200mg docusate 10ml senna liquid + 10ml lactulose Rectal Measures Ensure adequate oral laxatives Undignified and inconvenient Suppositories Glycerol softens and lubricates Bisacodyl stimulates Usually given in combination 30mins to work Rectal Measures Enemas Micro-enemas Phosphate enemas Evacuates Arachis oil enema Softens May stools from the lower bowel hard and impacted stools need high enema if stools higher than the rectum Faecal Impaction Empty rectum/loaded colon Oral stimulant and softener +/- high enema Movicol Soft faeces Bisacodyl suppositories Hard faeces Oral laxatives Suppositories and osmotic enemas first Arachis oil retention enema Manual evacuation may be necessary Laxative Guidance Prescribe daily stimulant AND softener, especially if on opioids Escalate dose until bowels opened If maximum dose ineffective reduce by half and add an osmotic agent If bowels not opened for three days use rectal measures Continue daily oral laxatives Summary Points Constipation should be considered in all palliative care patients Prophylactic laxatives for patients on opioids are essential Consider PR examination in all constipated patients Remember non-drug measures Titrate oral laxative dose according to response Mouth Care Dry Mouth Reported in over 75% of patients Causes: Reduction in amount of saliva produced Poor quality of saliva Drug therapy XRT Dehydration And lots of others Associated Problems Chewing and swallowing impaired Taste impaired Difficulty speaking Poor oral hygiene Dental caries Dentures problematic Embarrassment Oral candida Other oral infection General deterioration in health Management of Dry Mouth Review medication Frequent sips of water Mouth care Debride tongue Mouthwashes Pineapple chunks Sponge sticks Lip salve Management of Dry Mouth Stimulate salivary flow Chewing gum, boiled sweets, citric acid Pilocarpine (Davies et al 1998) Artificial saliva Glandosane, Use Saliva Orthana, Oralbalance PRN Usually better than water Oral Candidiasis 30% of terminally ill patients Causes Dry mouth Dentures Topical steroids (oral corticosteroids, antibiotics) Oral Candidiasis Features: May be asymptomatic Symptoms may relate to underlying cause e.g. dry mouth White plaques +/- smooth, red, painful tongue +/angular stomatitis Oral Candidiasis Treatment Good mouth care, including dentures Treat underlying problem Topical antifungal agents e.g. nystatin for 10 days (sometimes continuous) Systemic antifungals e.g. fluconazole, ketoconazole Significant resistance to systemic antifungals Summary Gastrointestinal symptoms are extremely common in all cancer patients A thorough evaluation of the underlying cause of any symptom is vital Treatment should be directed according to the underlying cause Set achievable goals Review the response to treatment regularly