receptor activates G
advertisement

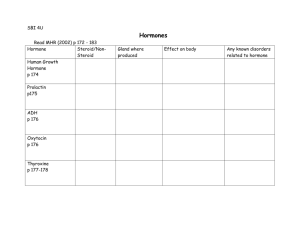
CLINICAL ENDOCRINOLOGY OBJECTIVES: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. Explain why the endocrine system is so closely related to the nervous system. Distinguish between an endocrine gland and an exocrine gland. Define the term hormone and explain its general characteristics. Distinguish between a steroidal and non-steroidal hormone, in terms of composition and action. For each of the glands, name the hormone(s) they secrete, identify the target organ of each hormone, and the effect of each hormone. Define the term gonadotropin, name of hormones secreted by the pituitary ,thyroid,adrenal glands,pancreatic gonadal gland …. Distinguish between dwarfism, giantism, and acromegaly Describe how calcium levels are maintained in the blood. The hormones that work together to regulate water and electrolyte levels in the blood and therefore regulate blood pressure. Describe how glucose levels are maintained in the blood. Compare and contrast cretinism, myxedema, Grave’s Disease, and goiter. Define the blood ,stimulatory tests, and other diagnostic procedures to define the disease. To describe secondary sexual characteristics ,differentiate between virilism and hirsutism, get information about PCOS and ovulatory cycle. Describe the adipose tissue -derived hormones ( leptin,adiponectin,resistin) and their role in adiposity Learning outcomes 1. List the cells and state the hormones secreted by anterior and posterior pituitary,thyroid gland,adrenal,pancreas, gonads 2. Explain the role of hypothalamus in controlling anterior & posterior pituitary 3. Describe the regulation of secretion & actions of different hormones 4. Explain the neural control of hormone release. 5. Describe specific hormonal disorders 6. Describe the role of adipose tissue in regulation of body metabolism Nervous and Endocrine Systems • Act together to coordinate functions of all body systems • Nervous system – Nerve impulses/ Neurotransmitters – Faster responses, briefer effects, acts on specific target • Endocrine system Composed of endocrine glands produce, store, and secrete hormones. that – HORMONE = a very powerful chemical substance secreted by an endocrine gland into the bloodstream, that affects the function of another cell or "target cell Types of Glands Exocrine Glands are those which release their cellular secretions through a duct which empties to the outside or into the lumen (empty internal space) of an organ. These include certain sweat glands, salivary and pancreatic glands, and mammary glands. They are not considered a part of the endocrine system. Endocrine Glands are those glands which have no duct and release their secretions directly into the intercellular fluid or into the blood. The collection of endocrine glands makes up the endocrine system.The main endocrine glands are : pituitary (anterior and posterior lobes) thyroid, parathyroid - ` Adrenal (cortex and medulla) pancreas and gonads • Hormone types – Circulating – circulate in blood throughout body – Local hormones – act locally • PARACRINE – act on neighboring cells • AUTOCRINE – act on the same cell that secreted them General characteristic of hormones 1. needed in very small amounts (potent); 2. produce long-lasting effects in the cells they target; 3. regulate metabolic processes (maintain homeostasis) 4. may be steroid (produced from cholesterol = fat-soluble) or non-steroid (water-soluble). 5. they have specific rates and patterns of secretion (diurnal, pulsatile, cyclic patterns, pattern that depends on the level of circulating substrates) 6. they operate within feedback systems, either positive(rare) or negative, to maintain an optimal internal environment 7. they affect only cells with appropriate receptors specific cell function(s) is initiated 8. they are excreted by the kidney, deactivated by the liver or by other mechanisms Some general effects of hormones Hormones regulate the transport of ions, substrates and metabolites across the cell membrane: 1. they stimulate transport of glucose and amino acids 2. they influence of ionic transport across the cell membrane 3. they influence of epithelial transporting mechanisms 4. they stimulate or inhibit of cellular enzymes 5. they influence the cells genetic information Control of Hormone Secretion Control of secretion is in the form of neural, hormonal, or humoral stimuli. 1. Neural: Signals from nervous system The adrenal medulla is directly stimulated by the sympathetic nervous system. Epinephrine and NE reinforce the actions of the sympathetic nervous system. 2. Hormonal Occurs when hormones from one endocrine gland stimulate the secretion of hormones from another endocrine gland. E.g. TRH,TSH, TH E.g. CRH, ACTH,Cortisol These routes of secretion are usually controlled in a negative feedback manner. 3. Humoral : Chemical changes in the blood Occurs when substances other than hormones control the secretion of endocrine glands. E.g. Insulin secretion by the pancreas is determined by several factors. Rise in glucose after a meal triggers insulin secretion. Rise in amino acids after a meal triggers insulin secretion. In addition hormonal and neural stimuli also play a role in insulin secretion. or change in osmolarity (ADH release) Chemical classes of hormones 1. Amino acid-derived: Hormones that are modified amino acids (catecholamines, thyroid hormones, prostaglandins, leucotrienes, dopamine, serotonine, GABA, melatonin) 2. Polypeptide and proteins: Hormones that are chains of amino acids of less than or more than about 100 amino acids, respectively. Some protein hormones are actually glycoproteins, containing glucose or other carbohydrate groups. (insulin, GH, Leptin...) 3. Steroids: Hormones that are lipids synthesized from cholesterol. Steroids are characterized by four interlocking carbohydrate rings.(a) Corticoids (cortisol, aldosterone,, b) sex hormones(androgen,estrogen, progesterone),c) Nitric oxide (NO) 4. Eicosanoids: Are lipids synthesized from the fatty acid chains of phospholipids found in plasma membrane. Hormones circulating in the blood diffuse into the interstitial fluids surrounding the cell. Cells with specific receptors for a hormone respond with an action that is appropriate for the cell. Because of the specificity of hormone and target cell, the effects produced by a single hormone may vary among different kinds of target cells. Another groups of hormones A. gastrointestinal hormones (more than 26 GI polypeptides) B. opioid peptides (endogenic opioids) C. tissue growth factors (epidermal growth factor, nerve growth factor, PDGF, insuline-like growth factor ...) D. atrial natriuretic hormone (ANF) E. transforming growth factors and hematopoietic and other growth factors (FGF....) F. endothelial factors (endothelins, EDRF...) G. cytokines (interleukiny, interferón, TNF....) Hormones activate target cells by one of two methods, depending upon the chemical nature of the hormone. • Lipid-soluble hormones (steroid hormones and hormones of the thyroid gland) diffuse through the cell membranes of target cells. The lipid-soluble hormone then binds to a receptor protein that, in turn, activates a DNA segment that turns on specific genes. The proteins produced as result of the transcription of the genes and subsequent translation of mRNA act as enzymes that regulate specific physiological cell activity. •Lipid-soluble hormones are bound to plasma proteins and are less easily metabolized and excreted from the body. E.g. TH has a half-life of several days. E.g. Cortisol has a half-life of about 90 minutes Blood capillary Free hormone 1 Lipid-soluble 1 Lipid-soluble Transport protein Transport protein hormone hormone diffuses diffuses into cell into cell Activated 2 Activated receptor-hormone receptor-hormone complex alterscomplex alters gene expression gene expression 2 Nucleus Nucleus Receptor Receptor DNA DNA Cytosol 3 Cytosol 3 Newly formed Newly formed mRNA directs mRNA directs synthesis of synthesis of specific proteins specific proteins on ribosomes on ribosomes mRNA mRNA Ribosome Ribosome New protein 4 New proteins alter cell's activity Target cell Lipidsoluble Water-soluble hormones (polypeptide, protein, and most amino acid hormones) bind to a receptor protein on the plasma membrane of the cell. The receptor protein, in turn, stimulates the production of one of chemical messengers. - Water-soluble hormones are easily degraded by enzymes in the blood stream and are also excreted very quickly from the kidneys. E.g. insulin has a half-life of about 10 minutes in the body. E.g. Epinephrine has a half-life of about 10 seconds in the body. Blood capillary Blood capillary Binding(first of hormone messenger) (first messenger) 1 Binding of1 hormone Watersoluble Hormones to its receptorto activates its receptor G protein, activates G protein, which activates which adenylate activates cyclase adenylate cyclase Water-soluble hormone Adenylate cyclase Adenylate cyclase Receptor Second messenger G protein G protein ATP ATP cAMP Second messenger 2 Activated cAMP adenylate 2 Activated adenylate cyclase converts ATP to cAMP cyclase converts ATP to cAMP 6 Protein Protein kinases kinases serves serves as a as a 3 cAMP 3 cAMP Activated second second messenger messenger protein to activate to activate protein protein kinases kinases kinases Protein Protein Activated protein kinases 4 Activated protein ATP kinases phosphorylate ATP cellular proteins ADP ADP Protein— Protein— P P Millions of phosphorylated 5 Millions5 of phosphorylated proteins cause proteins reactions cause that reactions that produce physiological produce physiological responses responses Target cell Phosphodiesterase inactivates cAMP 4 Activated protein kinases phosphorylate cellular proteins second messengers: The small molecule generated inside cells in response to binding of hormone or other mediator to cell surface receptors • Calcium (Ca2+) – Target: calmodulin – Calmodulin protein kinases • Cyclic nucleotides – cAMP & cGMP – Target: protein kinases • Diacylglycerol (DAG) & IP3 – Phosphoipase C act on the PIP2 From membrane lipids – DAG Protein Kinase C (membrane) – IP3 Ca2+ (triggers the release of Ca2+from the endoplasmic reticulum, which then activates enzymes that generate cellular changes.) RECEPTORS: General Characteristics of Receptors • Receptors bind hormones, resulting in a biological response • All receptors exhibit general characteristics: 1. Specific Binding (structural and steric specificity) 2. High Affinity (at physiological concentrations) 3. Saturation (limited, finite # of binding sites) 4. Signal Transduction (early chem event must occur) 5. Cell Specificity (in accordance with target organ specificity). All receptors have two functional domains: Recognition domain: it binds the hormone 2. Coupling domain: it generates a signal that couples the hormone recognition to some intracellular function. Coupling means signal transduction. Receptors are proteins. 1. They are present in cell membranes Intracellular receptors: cytoplasmic receptors nuclear receptors Cell Surface (membrane)Receptors There are three types of cell surface receptors: 1. Ion channel receptors :Ionotropic 1. Transmembrane receptors: G-proteincoupled receptors,Metabotropic Receptors that are kinases or bind kinases: Protein kinases phosphorylation Neurotrophins Cell surface receptors: G- protein receptors A. a. b. c. d. Basic G-protein Receptor ligand binds to receptor (outer surface of cell). receptor changes shape (inner surface of cell). shape change allows receptor to bind inactive G-protein inactive G-protein binds to receptor receptor activates G-protein a. G-alpha drops GDP, picks up GTP b. when G-alpha binds GTP --> G-beta and G-gamma are released c. G-alpha + GTP is released from receptor into cytoplasm d. G-alpha + GTP = active G-protein. e. activated G-protein binds to target protein target protein's activity is altered - might be stimulated or might be inhibited . f. G-alpha + GTP is released from receptor into cytoplasm g. G-alpha + GTP = active G-protein. h. The G protein activates adenylate cyclase, the enzyme that catalyzes the production of cAMP from ATP.Cyclic AMP then triggers an enzyme that generates specific cellular changes - might be stimulated or might be inhibited . Intracellular Receptors • Some receptor proteins are intracellular, found in the cytosol or nucleus of target cells • Small or hydrophobic chemical messengers (1st messenger,I,e hormone) can readily cross the membrane and activate receptors • Examples of hydrophobic messengers are the steroid and thyroid hormones of animals • An activated hormone-receptor complex can act as a transcription factor, turning on specific genes The action of nuclear receptors is slow, as it takes some hours for the whole process to occur. The effect is long-lasting (or even permanent) and changes the properties of the cell. This type of process is important in development, differentiation and maturation of cells, e.g. gametes (eggs and sperm cells). Transcriptional activator proteins DNA RNA Proteins Steroid Hormones Steroid hormones are lipid soluble. Steroids can diffuse through the membrane 1. Diffuse through the membrane 2. Binds & activates intracellular receptor. 3. Steroid-Receptor complex then enters the nucleus and binds to a particular sequence on the DNA which is called hormone response element (HRE). 4. Activates a gene. 5. Gene transcribed into messenger RNA. 6. mRNA goes to the ribosomes 7. Translate mRNA into protein Thyroid and Retinoids go directly into the nucleus. Their receptor is already bound to HRE, but along with a co –repressor protein which fails to activate transcription. The association of the ligand with the receptor results in the dissociation of the co repressor. Now this receptor- ligand complex can bind other co activator proteins and transcription begins. Negative Feedback in the Hypothalamus. • Most hormonal regulation by negative feedback – Few examples of positive feedback • hypothalamus maintains fairly constant levels of hormones because it operates The a negative feedback system. E.g: excitatory Hypothalamus Thyroid Stimulating Hormone-Releasing Hormone inhibitory Anterior pituitary Thyroid Stimulating Hormone Thyroid gland Thyroid hormones • positive feedback. In such a system, hormones cause a condition to intensify, rather than decrease. As the condition intensifies, hormone production increases. Such positive feedback is uncommon, but does occur during childbirth, where hormone levels build with increasingly intense labor contractions. Also in lactation, hormone levels increase in response to nursing, which causes an increase in milk production. The hormone produced by the hypothalamus causing the milk let down and uterine contraction is oxytocin. A classic example is the production of estrogen in response to gonadotropins. The consequences (or the outcome ) of increased estrogen production are the further production of gonadotropins, thus promoting more estrogen production. Mechanisms of hormonal alterations Endocrine diseases A. elevated hormones level B. depressed hormones level Hormone excess Hormone deficiency Hormone resistance may be caused by: 1. failure of feedback systems 2. dysfunction of endocrine gland or endocrine function of cells: a) secretory cells are unable to produce or do not obtain an adequate quantity of required hormone precursors b) secretory cells are unable to convert the precursors to the appropriate active form of hormon c) secretory cells may synthesize and release excessive amounts of hormone 3. degradation of hormones at an altered rate or they may be inactivated by antibodies before reaching the target cell 4. ectopic sources of hormones C. failure of the target cells to respond to hormone May be caused by: 1. receptor-associated disorders: a. decrease in the number of receptors hormone - receptor binding b. impaired receptor function sensitivity to the hormone c. antibodies against specific receptors d. unusual expression of receptor function 2. intracellular disorders:a) inadequate synthesis of the second messengers b) number of intracellular receptors may be decreased or they may have altered affinity for hormones c) alterations in generation of new messenger RNA or absence of substrates for new protein synthesis Primary & secondary endocrine diseases Based on site of hormone defect (either increase or decreased secretion), Endocrine disorders are classified as: • A) Primary Disease: If defect is in the target gland from which hormone has originated • B) Secondary Disease: If defect is in the Anterior Pituitary or Hypothalamus E.g., • Primary hypothyroidism means decreased secretion of thyroid hormone from the Thyroid gland • Secondary hypothyroidism means deficiency of Anterior pituitary/ Hypothalamic hormone which stimulates production of thyroid hormone from the thyroid gland (defect not in the thyroid gland) Investigations for Endocine Disorders I. Basal hormonal concentrations 1. Basal plasma levels (one-time examination) 2. Diurnal dynamics of hormone concentrations (e.g. cortisol,growth H) 3. Other hormonal cycles (e.g. menstrual phase dynamics: cyclic changes of LH, FSH, estrogens and progesteron) 4. Urinary output: 24 hr Is alternative method for hormones with diurnal dynamics (cortisol, aldosterone) or pulsate secretion (catecholamines), 5. Hormonal metabolites - plasma, urine (e.g. C-peptide), 5HIAA (hydroxyindole acetic acid),Serotonin metabolite Urinary excretion measurement in patients with suspicious carcinoid. 6. Indirect evaluation - measurement of a metabolic response (ADH ... diuresis, insulin ... glycaemia etc.) II. Functional tests Functional tests:1. Inhibitory tests 2. Stimulatory tests Basal hormonal concentration very often doesn´t allow to establish a diagnosis of hypo- or hyperfunction. Suspect hypofunction Stimulatory tests = quantification of functional reserve of endocrine gland, Insulin hypoglycemia test, Arginin infusion test,TRH test GnRH test,CRH test Suspect hyperfunction Inhibitory tests = quantification of responsibility of endocrine gland to inhibitory factors, e.g. Dexamethazone test, Dopaminergic drugs test Principles: • negative feedback inhibition / stimulation • direct stimulation / inhibition Tumor markers in endocrinology Thyroglobulin (Tg), anti-Tg antibodies Markers of non-medullar thyroid carcinoma. CEA (carcinoembryonic antigen) Marker of non-medullar thyroid carcinoma (and ather malignancy – e.g. colorectal ca) Diagnostic usage in combination with Tg and anti-Tg Ab Calcitonin, procalcitonin Hormonal product and diagnostic marker of medullar thyroid carcinoma (lower sensitivity that Tg for non-medullar thyroid ca) newborn screening : 1. Congenital hypothyroidism - incidence 1 : 5000 screening based on elevation of TSH 2. Congenital adrenal hyperplasia (CAH) - incidence 1 : 10-14000 screening based on elevation of 17-OH-progesterone 3. Phenylketonuria Imaging methods Indications: A. Localization of endocrine active tumors, hyperplasia, ectopic hormonal production B. Evaluation of systemic complications 1. Native X-ray exams 2. Ultrasonography 3. CT / MRI 4. Scintigraphy 5. Angiography Biopsy Thyroid gland - unclear solitary nodule, tumors 2. Adrenal glands - rarely Thyroid gland - Fine needle aspiration biopsy (FNAB)