ANKLE FRACTURE
advertisement

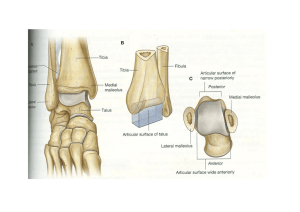
DR. Rahmatullah Highest incidence in elderly women Incidence – 187 per 1 lakh people per year Isolated malleolar fractures – 66 % Bi malleolar fractures – 25% Tri malleolar fractures – 5 to 10% Open fractures – 2% Incresed BMI is a risk factor. • • • Complex hinge joint with complex ligamentous system The plafond is concave in AP plane & convex in Lateral plane Plafond is wider anteriorly to allow for congruency with the wedge shaped talus Talar dome is trapezoidal, with anterior aspect 2.5 cm wider than posterior talus Chaput's tubercle: insertion site of anterior tibiofibular ligament on the anterolateral tibia Wagstaffe's tubercle: insertion site of anterior tibiofibular ligament on the anterior fibula Volkmann's tubercle: tibial insertion of posterior tibiofibular ligament at the posterolateral aspect of tibia Anterior colliculus: located at anterior, inner aspect of medial malleolus distally, Insertion site of deltoid ligament. Larger than posterior colliculus Posterior colliculs: located at posterior, inner aspect of medial malleolus distally, Insertion site of deltoid ligament. SYNDESMOTIC LIGAMENT COMPLEX : Exists between distal tibia & fibula Composed of 1) Anterior Inferior TibioFibular Ligament 2) Posterior Inferior TibioFibular Ligament – thicker & stonger 3) Transverse TibioFibular Ligament 4) Interosseous Ligament SUPERFICIAL PORTION : 3 ligaments originates from anterior colliculus 1) Tibionavicular Ligament 2) Tibiocalcaneal Ligament 3) Tibiotalar Ligament – most prominent DEEP PORTION : Originates on inter collicular groove and posterior colliculus 1. Deep ant talotibial Ligamen 2. Deep post talotibial Ligament Not as strong as medial complex 1)Ant Talofibular Ligament -weakest of lat ligaments 2) Post Talofibular Ligament -strongest of lat ligaments 3)Calcaneofibular Ligament Stabilises subtalar joint & limits inversion Rupture of this ligament causes POSITIVE TALAR TEST These rules are used to determine the need for radiographs in patients with an ankle injury. Ankle X-ray series are only required in case of: Bone tenderness along the distal 6 cm of the posterior edge of the fibula or tip of the lateral malleolus. Bone tenderness along the distal 6 cm of the posterior edge of the tibia or tip of the medial malleolus. Inability to bear weight for 4 steps both immediately and in the emergency department Tibiofibular overlap should be>10mm Tibiofibular clear space <5mm Talar tilt : difference in width of medial & lateral aspect of the superior joint space should be <2mm . The dome of talus should be centered under the tibia & congruous with tibial plafond Posterior tuberocity # & avulsion # of talus can be identified Taken with foot in 15-20 degrees of internal rotation that is perpendicular to intermalleolar axis Medial clear space should be equal to superior clear space, should be <4mm, >4mm is abnormal & indicates lateral talar shift Talocrural angle : angle subtended between the inter malleolar line and a line parallel to the distal tibial articular surface - 8 to 15 degrees. - should be within 2 to 3 degrees of un injured ankle. Tibiofibular overlap should be > 1mm, <1mm is syndesmotic injury Talar shift >1mm is abnormal Tibiofibular clear space should < 6mm Normal ROM – dorsiflexion : 30 & plantar flexion – 45 degrees Minimum of 10 degree of dorsiflexion & 20 degree of plantar flexion are required for normal gait Axis of ankle flexion runs between 2 malleoli, which is externally rotated 20 degrees Lateral talar shift of 1mm will decrease surface contact by 40%, & 3mm shift results in >60% decrease Disruption of syndesmotic ligaments results in decreased tibiofibular overlap & lateral talar shift Swelling, tenderness, variable deformity from a limp to non ambulatory. Check for Neurovascular status & extent of soft tissue injury Squeeze test – positive in high ankle sprains, syndesmotic injuries Dislocated ankle should be reduced & splinted immediately CT scan- specially for plafond #s MRI –for ligament, cartilage, tendon injuries BONE SCAN – for occult #, continued pain after injury Takes into account 1) the position of the foot at the time of injury 2) the direction of deforming force Based on cadaveric studies Patterns may not always reflect clinical reality 10-20% of malleolar # Only type asso with medial displacement of talus STAGE-I : Transverse avulsion # fibula (or) Rupture of talofibular ligament STAGE-II : - Vertical medial malleolus # -Transverse distal fibula # -Medial plafond impaction 40-70% of malleolar # occurs with this mech. STAGE-I : Disruption of ant tibiofibular lig +/avulsion # STAGE- II: Spiral # of distal fibula STAGE- III: Disruption of post tibiofibular lig (or) # of post malleolus STAGE- IV: Transverse avulsion # of medial malleolus (or) rupture of deltoid ligament 5-20% of malleolar # STAGE- I : Transverse medial malleolus # (or) rupture of deltoid ligament STAGE- II : Disruption of ant tibiofibular lig +/avulsion # STAGE- III : Spiral # distal fibula at/above the level of syndesmosis STAGE- IV : Disruption of post tibiofibular lig (or) avulsion # of posterolateral tibia 5-20% of malleolar # STAEGE- I : Transverse fracture of medial malleolus (or) rupture of deltoid lig STAGE- II : Rupture of syndesmotic lig (or) avulsion # with medial injury STAGE- III : Transverse/laterally comminuted # fibula with medial injury Based on the level of fibular # The more proximal, the greater risk of syndesmotic disruption & instability type A type B below level of the ankle joint Tibio fibular syndesmosis intact Deltoid ligament intact Medial malleolus often fractured usually stable : occasionally requires ORIF at the level of the ankle joint, extending superiorly and laterally up the fibula tibiofibular syndesmosis intact or only partially torn, but no widening of the distal tibiofibular articulation medial malleolus may be fractured or deltoid ligament may be torn variable stability type C above the level of the ankle joint tibiofibular syndesmosis disrupted with widening of the distal tibiofibular articulation medial malleolus fracture or deltoid ligament injury present unstable : requires ORIF 1 - Disruption of the medial ankle joint with small bone avulsion 2 - Disruption of the distal tibio-fibular syndesmosis No fibular fracture is visible at the ankle raising the suspicion of a proximal fibular fracture Spiral fracture of the proximal fibula It is a pronation & external rotation injury CURBSTONE # : Avusion fracture of posterior tibia is produced by a trippling mechanism LEFORTE – WAGSTAFFE # : -Anterior fibular tubercle avulsion fracture by anterior tibiofibular ligament -Associated with Lauge-Hansen SER type # THILLAUX – CHAPUT # : - Anterior tibial tubercle avulsion fracture by anterior tibiofibular ligament - Counter part of Leforte-Wagstaffe # VOLKMANNS TRIANGLE: -Bony avulsion of posterior tibiofibular ligament from the tibia HERSCOVICI CLASSIFICATION of medial malleolar fractures. A - tip avulsions (anterior colliculus) B - intermediate C - level of plafond D - above plafond (adduction fractures) Posterior colliculus fracture : - the fragment is nondisplaced because of stabilisation by posterior tibial & flexor digitorum longus tendons - supra malleolar spike clearly seen on external rotation views. Emergency room : -Dislocated ankles should be reduced immediately. If reduction fails , go for urgent surgical reduction - open wounds, abrasions cleansed & dressed - fracture reduction for displaced fractures - splint application STABLE FRACTURES Ankles with perfect position of the talus and with no medial swelling and tenderness are considered to be stable, follow-up x-ray 1 week after injury to ensure there is no displacement. if talus is perfectly centered but medial swelling and tenderness, take stress x-rays. - If there is no sign of talar shift, the ankle is considered to be stable. removable walking boot or short-leg cast for 6 wks with crutches but bear weight as tolerated Sport activity limitation for 3 months Nonoperative short-leg walking cast/boot indications isolated nondisplaced medial malleolus fx or tip avulsions isolated lateral malleolus fx with < 3mm displacement and no talar shift posterior malleolar fx with < 25% joint involvement or < 2mm step-off OPERATIVE : open reduction internal fixation indications any talar displacement displaced isolated medial malleolar fx displaced isolated lateral malleolar fx bimalleolar fx and functional bimalleolar fracture posterior malleolar fx with > 25% or > 2mm step-off Bosworth fracture-dislocations (distal fibula # with posterior dislocation of proximal fibular fragment behind posterior tibial tubercle ) open fractures TECHNIQUE : goal of treatment is stable anatomic reduction of talus in the ankle mortise 1 mm shift of talus leads to 42% decrease in tibiotalar contact area OUTCOMES : overall success rate of 90% prolonged recovery expected (2 yrs to obtain final functional result) worse outcomes with: smoking, decreased education, alcohol use, increased age, presence of medial malleolar fracture ORIF superior to closed treatment of bimalleolar fxs in Lauge-Hansen supination-adduction fractures restoration of marginal impaction of the anteromedial tibial plafond leads to optimal functional results after surgery Isolated Medial Malleolus Fx Nonoperative short leg cast indications nondisplaced fracture tip avulsion fractures Operative ORIF If they are displaced, thick periosteum usually folds into the fracture site leading to nonunion. indications any displacement or talar shift technique lag screw fixation lag screw fixation stronger if placed perpendicular to fracture line antiglide plate with lag screw best for vertical shear fractures tension band fixation utilizing stainless steel wire Used when fragment is small & in osteroporotic fragments Adverse effect - posterior tibial tendon irritation 4.0 mm partially threaded screws work well for most patterns Screws should be perpendicular to the fracture line and parallel for maximal compression Spread two screws for good stability Ignore or excise small anterior colliculus fractures Use fluoroscopy to be sure screws are clear of the joint Beware supination adduction patterns with vertical fracture lines and impacted medial dome fragments Oblique fractures of posterior colliculus involve posterior lip of the tibia. - On the AP x-ray- double profile of the medial malleolus. - better visualized on a slightly externally rotated AP x-ray Isolated Lateral Malleolus Fx Nonoperative short leg cast indications intact mortise, no talar shift, < 3mm displacement Operative ORIF indications if talar shift or > 3 mm of displacment can be treated operatively if also treating an ipsilateral syndesmosis injury Techniques : open reduction and plating intramedullary retrograde screw placement isolated lag screw fixation Most commonly fixed with one third tubular plate 3 types of plate orientations : lateral, posterolateral, posterior Avoid screw impingement on talofibular articular surface in lateral plating Posterior fibuar plating conditions : when # is more distal, dislocation is posterior, osteopenic bone - distal part of plate provides buttress & stabilise # even without distal screws - provides maximum stability - m/c disadvantage of posterior antiglide plating – peroneal irritation if the plate is too distal when # is long, oblique, non comminuted - isolated lag screw fixation Intra medullary screw or rod fixation : - more limited approach - particularly difficult in SER type #s Severly comminuted fibula #s : seen in Pronation-Abduction injuries - if asso with MM #, first fix MM that stabilises talus which reduces fibula - Bone grafting is not necessary - the position of the talus in the mortise should be used as the ultimate guide to accurate position of the distal fibula. Avoid injuring the superficial peroneal nerve with anterolateral incisions Make sure the distal fibula is fully out to length Laterally comminuted pronation abduction patterns are most difficult For maximal stability place a plate posterior Consider the location of syndesmosis fixation when placing a fibular plate Test the syndesmosis after lateral malleolar fixation Beware in short distal segments, elderly patients with osteopenic bone, diabetics For bimalleolar or trimalleolar fractures Fix the fibula fracture before reducing and fixing the medial malleolus. When the fibula is laterally comminuted and the medial malleolus fracture is large, we reduce and fix the medial malleolus fracture first. posterior malleolar evaluation and possible reduction and fixation as the last step in ankle fixation. The superficial peroneal nerve is at risk during the lateral approach to the fibula. The sural nerve lies posterior to the fibula, and during a posterolateral approach to the fibula, it should be identified and protected The deep peroneal nerve, the anterior tibial artery and branches of the superficial peroneal nerve are at risk when small incisions are made for front-to-back posterior malleolar fixation small increase in the medial clear space and valgus sag of the talus might be apparent - The talus is narrowest posteriorly leading to increased space in the mortise in plantar flexion. - absence of the deltoid allows the talus to rotate externally, - technique not necessary to repair medial deltoid ligament only need to explore it if you are unable to reduce the mortise Interposition of the deltoid ligament is one potential cause of residual talar shift , but very unusual. The clinical outcome of these ankle fractures is not improved by suturing the deltoid ligament External rotation lateral x ray view & CT scan are choice Increased rotation and posterior subluxation of the talus with positive posterior drawer test but have little effect on stability in inversion or eversion Trimalleolar fractures are known to have a worse prognosis than bimalleolar fractures (23). Large posterior malleolar fractures lead to poorer outcomes Approach : direct ( posterior to anterior) indirect (anterior to posterior) most important factor in reducing and stabilizing the posterior malleolus is accurate stable fixation of the associated fibular # In trimalleolar #, first fix MM, LM & then fix post malleolus When the fibula is reduced, the posterior malleolus is often nearly reduced, and the talus is centered After fibular fixation check posterior drawer test for posterior stability Non operative : short leg cast indications < 25% of articular surface involved evaluation of percentage should be done with CT, as plain radiology is unreliable < 2 mm articular stepoff OPERATIVE : ORIF indications > 25% of articular surface involved > 2 mm articular stepoff ipsilateral syndesmosis injury technique use posterolateral or posteromedial approach to the ankle joint to reduce and place fixation decision of approach will depend on fracture lines and need for fibular fixation can use anterior to posterior lag screws to capture fragment (if nondisplaced) syndesmosis injury stiffness of syndesmosis restored to 70% normal with isolated fixation of posterior malleolus (versus 40% with isolated syndesmosis fixation) stress examination of syndesmosis still required after posterior malleolar fixation posteroinferior tibiofibular ligament may remain attached to posterior malleolus and syndesmotic stability may be restored with isolated posterior malleolar fixation Bosworth Fracture-DislocationOverview rare fracture-dislocation of the ankle where the proximal fibula fragment becomes entrapped behind the posterior tibial tubercle and becomes irreducible posterolateral ridge of the distal tibia hinders reduction of the fibula Operative open reduction and fixation of the fibula indicated in most cases Open Ankle Fx Operative emergent operative debridement and ORIF external fixation Associated Syndesmotic Injury Overview suspect injury in all ankle fractures most common in Weber C fracture , L-H pronation type & AO type C pattern. fixation usually not required when fibula fracture within 4.5 cm of plafond Higher fibula fractures >4.5cm result in syndesmotic widening despite internal fixation of the fibula fracture and require syndesmotic fixation When there is a proximal fibula fracture and the talus is shifted or when the talus is shifted without a fibula fracture, there is always a syndesmosis injury with instability Radiographically, syndesmosis instability should always be suspected when fibula fractures are above the level of the ankle mortise Stress x-rays : ankle in the mortise position with external rotation force Pronation-abduction injuries completely tear the entire syndesmosis and lead to greater instability than external rotation injuries Evaluation : measure clear space 1 cm above joint it has also been reported that there is no actual correlation between syndesmotic injury and tibiofibular clear space or overlap measurements lateral stress radiograph has more reliability than an AP/mortise stress film best option is to assess stability intra operatively with abduction /external rotation stress of dorsiflexed foot the decision to fix or not to fix the syndesmosis must be individualized in each case and preferably should be based on direct stress testing of syndesmosis integrity after internal fixation of other structures. instability of the syndesmosis is most in the anteriorposterior direction in the absence of a deltoid injury, fixing the syndesmosis is unnecessary, and if a medial malleolar fracture is securely fixed restoring the deltoid ligament, despite complete disruption of the syndesmosis, tibial fibular fixation is not needed (Boden SD, Labropoulos PA, McCowin P, et al.) syndesmosis screw fixation indications widening of medial clear space tibiofibular clear space (AP) greater than 5 mm tibiofibular overlap (mortise) narrowed any postoperative malalignment or widening should be treated with open debridement, reduction, and fixation technique length and rotation of fibula must be accurately restored open reduction required if closed reduction unsuccessful or questionable one or two cortical screw(s) 2-4 cm above joint, angled posterior to anterior 20-30 degrees lag technique not desired maximum dorsiflexion of ankle not required during screw placement (can't overtighten a properly reduced syndesmosis) SER injury that shows mild syndesmosis diastasis, a single threecortex 3.5-mm screw is sufficient, In Maisonneuve's proximal fibula fracture with complete disruption of the syndesmosis without a medial malleolus fracture, fixing the syndesmosis will provide the entire stability of the ankle postoperative screws should be maintained in place for at least 8-12 weeks must remain non-weight bearing, as screws are not biomechanically strong enough to withstand forces of ambulation controversies 3 or 4 cortices (3 – motion between tibia, fibula & 4- stable fixation) 3.5 mm or 4.5 mm screws implant material (stainless steel screws, titanium screws, suture, bioabsorbable materials) need for hardware removal no differences seen in hardware breakage, loosening, or removal at 1 year Use syndesmosis fixation when the medial clear space widens on intraoperative stress views after the fibula is fixed The fibula must be accurately reduced to the tibia in all views including the lateral Use a 4.5-mm four cortex screw if the patient will weight bear postoperatively Do not remove syndesmosis screws before 3-4 months postinjury Achieve a perfectly symmetric tibiotalar clear space Use syndesmosis fixation only without fixing the fibula fracture when it is above the midfibula Overcompressing the syndesmosis by applying a screw with the ankle in plantar flexion or using a compression technique should be avoided Polyglycolide or polylactide implants have been used most commonly Advantages : eliminating the need for hardware removal, decreasing irritation over prominent screws and plates, and allowing for gradual stress transfer from the implant to bone. used as screws for the fibula, syndesmosis, and the medial malleolus Polylactide implants have excellent MRI compatibility wound infection rate has been reported to be similar to that seen with metallic implants Chance of redisplacement – 0.9% with simple ankle # - 8.2% with complex unstable ankle fractures A local inflammatory granulomatous reaction to polyglycolide has been reported in 4% to 50% of malleolar fractures, in the 3rd or 4th postoperative month, is culture negative, that contains polyglycolide debris Polylactide implants degrade at a much slower rate than polyglycolide implants longer time to degrade significantly decreases the rate of reaction to these implants NONUNION – m/c in medial malleolus MALUNION – due to lateral malleolus shortening & external rotation WOUND PROBLEMS INFECTIONS POST TRAUMATIC ARTHRITIS REFLEX SYMPATHETIC DYSTROPHY – rare, minimised by anatomical restoration of ankle & early return of function COMPARTMENT SYNDROME OF LEG, FOOT TIBIOFIBULAR SYNOSTOSIS – asso with use of syndesmotic screw, usually asymptomatic LOSS OF REDUCTION – in 25% of unstable # treated non operatively LOSS OF ANKLE ROM