Mild perioperative hypothermia
advertisement

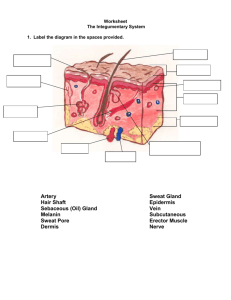
Perioperative Hypothermia Karim Rafaat, MD Introduction The human thermoregulatory system usually maintains core body temperature within 0.2℃ of 37℃ Perioperative hypothermia is common because of the inhibition of thermoregulation induced by anesthesia and the patient`s exposure to cool environment Hypothermia complications: Shivering prolonged drug effect, coagulopathy surgical wound infection morbid cardiac event Normal thermoregulation Processing of thermoregulatory information: afferent input central control efferent responses Normal thermoregulation Afferent input: cold signal-Aδ fiber warm signal-C fiber Each of the following contribute 20% of the total thermal input: Hypothalamus other parts of brain skin surface spinal cord deep abdominal and thoracic tissues Normal thermoregulation Primary thermoregulatory control center Hypothalamus Control of autonomic responses is 80% determined by thermal input from core structures In contrast, behavior response may depend more on skin temperature Normal thermoregulation The inter-threshold range (core temperatures that do not trigger autonomic thermoregulatory responses) is only 0.2℃ Each thermoregulatory response can be characterized by a threshold, gain, maximal response intensity Behavior is the most effective response Normal thermoregulation Major autonomic defenses against heat: 1. sweating 2.cutaneous vasodilation Major autonomic defenses against cold: 1.cutaneous vasoconstriction 2.nonshivering thermogenesis 3.shivering Normal Thermoregulation Sweating Active vasodilation 37 Vasoconstriction 36 Shivering Normal thermoregulation Vasoconstriction occurs in AV shunts located primarily in fingers and toes, mediated by α-adrenergic sympathetic nerves Non-shivering thermogenesis is important in infants, but not in adults (brown fat) Shivering is an involuntary muscle activity that increases metabolic rate 2-3 times Thermoregulation during general anesthesia General anesthesia removes a pt’s ability to regulate body temperature through behavior, so that autonomic defenses alone are available to respond to changes in temperature Anesthetics inhibit thermoregulation in a dosedependent manner and inhibit vasoconstriction and shivering about 2-3 times more than they restrict sweating Inter-threshold range is increased from 0.2 to 4℃ (20 times), so anesthetized pts are poikilothermic - with body temperatures determined by the environment Thermoregulation during general anesthesia The gain and maximal response intensity of sweating and vasodilation are well preserved when volatile anesthetics are given However volatile anesthetics reduces the gain of AV-shunt vasoconstriction, without altering the maximal response intensity Nonshivering thermogenesis dosen`t occur in anesthetized adults General anesthesia decreases the shivering threshold far more than the vasoconstriction threshold Anesthesia Impairs Regulation 38 Sweating Constriction 36 34 Shivering 32 30 Threshold (°C) 0.0 2.0 4.0 6.0 0.0 [Desflurane] (%) 0.1 0.2 0.3 [Alfentanil] (µg/ml) 38 36 34 32 30 0.3 0.6 0.9 [Dexmedetomidine] (ng/ ml) 0.0 2.0 4.0 6.0 8.0 [Propofol] (µg/ml) Inadvertent hypothermia during general anesthesia Inadvertent hypothermia during general anesthesia is by far the most common perioperative thermal disturbance (due to impaired thermoregulation and cold environment) Patterns of intraoperative hypothermia Phase I: Initial rapid decrease 0 -1 Phase II : Slow linear reduction ∆Core Temp (°C) -2 -3 Phase III: Thermal plateau 0 2 4 Elapsed Time (h) 6 Patterns of intraoperative hypothermia 1. Initial rapid decrease heat redistribution decreases 0.5-1.5℃ during 1st hr Tonic thermoregulatory vasoconstriction that maintains a temperature gradient between the core and periphery of 2-4℃ is broken The loss of heat from the body to environment is little Heat redistribution decreases core temperature, but mean body temperature and body heat content remain unchanged Patterns of intraoperative hypothermia 2. Slow linear reduction decreases in a slow linear fashion for 2-3hrs Simply because heat loss >metabolic heat production 90% heat loss through skin surface by radiation and convection Patterns of intraoperative hypothermia 3. Thermal plateau After 3-5 hrs, core temperature stops decreasing It may simply reflect a steady state of heat loss=heat production If a pt is sufficiently hypothermic, plateau phase means activation of vasoconstriction to reestablish the normal core-to-peripheral temperature gradient Temperature plateau due to vasoconstriction is not a thermal steady state and body heat content continues to decrease even though temperature remains constant Regional Anesthesia Regional anesthesia impairs both central and peripheral thermoregulation 38 Sweating 37 Hypothermia is common in patients given spinal or epidural anesthetics Threshold (°C) Vasoconstriction Shivering 36 35 Control Spinal Thermoregulation All thermoregulatory responses are neurally mediated 600 Control Spinal and epidural anesthetics disrupt nerve conduction to more than half the body 400 VO2 (ml/min) Epidural 200 The peripheral inhibition of thermoregulatory defense is a major cause of hypothermia during RA 0 35 36 37 Core Temperature (°C) RA also impairs the central control of thermoregulation The regulatory system incorrectly judges the skin temperature in blocked areas to be abnormally high It fools the regulatory system into tolerating core temperatures that are genuinely lower than normal without triggering a response Heat Balance and Shivering Initial hypothermia (Phase I) Redistribution of heat from core to periphery Primarily caused by peripheral inhibition of tonic thermoregulatory vasoconstriction Although the vasodilatation of AV shunts is restricted to the lower body, the mass of the legs is sufficient to produce substantial core hypothermia Subsequent hypothermia (Phase II) Loss of heat exceeds production Patients given SA or EA cannot reestablish coretemperature equilibrium because peripheral vasoconstriction remains impaired Hypothermia tends to progress throughout surgery Shivering Occurs during spinal and epidural anesthesia Disturbs patients and care givers but produces relatively little heat because it is restricted to the small-muscle mass cephalad to the block Treated by warming surface of skin or administration of clonidine / meperidine Temperature Monitoring Core Sites Pulmonary artery Distal esophagus Nasopharynx Tympanic membrane thermocouple Other generally-reliable sites Mouth Axilla Bladder Sub-optimal Forehead skin Infrared “tympanic” Infrared “temporal artery” Rectal Anesth Analg 2008 Potential Benefits of Mild Hypothermia Improves neurologic outcome after cardiac arrest Improves neurologic outcome in asphyxiated neonates Bernard, et al. Hypothermia after cardiac arrest study group Now recommended by European and American Heart Associations Number needed to treat: ≈6 Hypothermia recommended by International Liaison Committee Shankaren, et al. Gluckman, et al. Eicher, et al. Number needed to treat: ≈6 No benefit in major human trials Brain trauma in adults (Clifton, et al.) or children (Hutchison, et al.) Anurysm surgery: Todd, et al. Acute myocardial infarction: Dixon, et al Complications of Mild Hypothermia Many! Well documented Prospective randomized trials 1-2°C hypothermia Effects on many different systems Most patients at risk for at least one complication Complications of Mild Hypothermia Wound infection---the most common serious complication due to Impaired immune function decreased cutaneous blood flow protein wasting decreased synthesis of collagen Wound Infections: Melling, et al. Wound Infection (%) 16 P = 0.001 12 8 4 0 Hypothermic Normothermic Normothermia is more effective than antibiotics! Coagulopathy Hypothermia reduces platelet function and decreases the activation of the coagulation cascade From in vitro studies, it increased the loss of blood and the need for allogenic transfusion during elective primary hip arthroplasty Blood Loss 20% less blood loss per °C Transfusion Requirement 22% less blood Transfusion per °C Myocardial Outcomes: Frank, et al. Drug metabolism Mild hypothermia decreases the metabolism of most drugs Propofol ---during constant infusion, plasma conc. is 30 percent greater than normal Atracurium---a 3 ℃ reduction in core temp. increase the duration of muscle relaxation by 60 percent Significantly prolongs the postoperative recovery period Duration of Vecuronium 80 Duration of Action (min) 60 40 20 Normothermic (36.6 ± 0.1°C) Hypothermic (34.6 ± 0.3°C) Recovery Duration Time (min) Thermal comfort Patients feel cold in postoperative period, sometimes rating it worse than surgical pain Shivering occurs in ~40 percent of unwarmed patients who are recovery from GA Summary: Consequences of Hypothermia Benefits Improves neurologic outcomes after cardiac arrest Improves neurologic outcomes after neonatal asphyxia Major complications Increases morbid myocardial outcomes Promotes bleeding and increases transfusion requirement Increases risk of wound infections and prolonges hospitalization Other complications Decreased drug metabolism Prolonged recovery duration Thermal discomfort Treating and Preventing Intraoperative Hypothermia Preventing redistribution hypothermia The initial reduction in core temperature is difficult to treat because it result from redistribution of heat Prevent by skin-surface warming → → Peripheral heat content ↑ Temperature gradient ↓ Redistribution of heat ↓ Prewarming Prevents Hypothermia 38 37 TM 36 (°C) 35 No Warming Pre-Warming 34 -60 0 Time (min) 60 Airway heating and humidification Less than 10% of metabolic heat is lost through respiratory route Passive or active airway heating and humidification contribute little to thermal management • Fluid Warming Cooling by intravenous fluids 0.25°C per liter crystalloid at ambient temperature 0.25°C per unit of blood from refrigerator Fluid warming does not prevent hypothermia! Most core cooling from redistribution 80% of heat loss is from anterior skin surface Cooling prevented by warming solutions Type of warmer usually unimportant Cutaneous Warming The skin is the predominant source of heat loss during surgery, mostly by radiation and convection Evaporation from large surgical incisions may be important An ambient temp. above 25℃ is frequently required, but this is uncomfortable for gowned surgeons Heat loss can be reduced by covering the skin( with surgical draps, blankets, or plastic bags……) Insulator Forced-air warming Typically, forced-air warming alone or combined with fluid warming is required to maintain normal intraoperative core temp. Insulating Covers 120 100 Heat Loss (W) Plastic Cotton Cloth 80 Paper 60 -20 -0 20 40 Time (min) 60 ThermalDrape More Layers Do Not Help Much 100 80 1 Unwarmed 60 1 Warm 3 Unwarmed Heat Loss 40 (W) 3 Warm 20 0 -20 0 20 Time (min) 40 60 Forced-Air vs. Circulating-Water 38 Forced-Air 36 3.5°C Temp (°C) 34 Circulating-Water 0 4 8 Time (h) 12 Over-body Resistive Warming Negishi, A&A 2003 Röder, BJA 2011 The Relative Effects of Warming Methods on Mean Body Temperature. Conclusions Temperatures throughout the body are integrated by a thermoregulatory system General anesthesia produces marked, dose-dependent inhibition of thermoregulation to increase the interthreshold range by roughly 20-fold Regional anesthesia produces both peripheral and central inhibition The combination of anesthetic-induced thermoregulatory impairment and exposure to cold operating rooms makes most surgical patients hypothermic The hypothermia initially results from a redistribution of body heat and then from an excess of heat loss Perioperative hypothermia is associated with adverse outcomes, including cardiac events, coagulopathy, wound infections…… Unless hypothermia is specially indicated, the intraoperative core temperature should be above 36 ℃