HEADACHE
advertisement

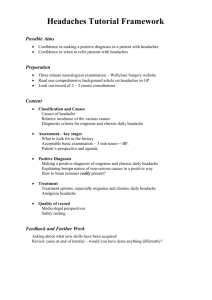
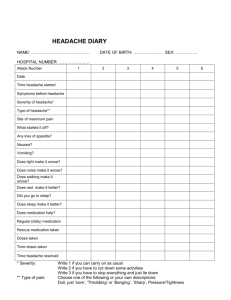
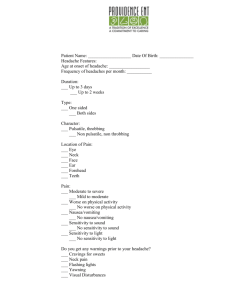
HEADACHE 4th year module Introduction • Headaches are very common – who hasn’t had one? • We see a lot of patients with headache in the ED and the trick is to work out those that have a benign cause for their headache vs those who have a potentially devastating diagnosis. • An excellent history and thorough examination will greatly help in differentiating these two group of patients Headache – a framework • Primary headache • Recurrent and (generally)benign • Secondary headache • Due to an underlying disease process • Potentially very serious/fatal Primary headache • • • • Migraine Tension headache Cluster headache Rebound or analgesia associated headache Secondary headache • Vascular • • • • • Subarachnoid haemorrhage AVM Stroke Cavernous sinus thrombosis Carotid or vertebral artery dissection • Temporal arteritis • Tumour • Trauma • Epidural/subdural/subarachnoid haemorrhage • Infection • Meningitis • Encephalitis • Brain abscess • Benign intracranial hypertension • Ophthalmological • Glaucoma • Optic neuritis • Iritis • Toxins • Carbon monoxide poisoning • Metabolic • • • • Hypoxia Hypercapnoea Hypoglycaemia Preeclampsia • Other • • • • • Sinusitis Dental TMJ dysfunction Trigeminal neuralgia Post LP headache History • A good history is essential in the diagnosis of the cause of the patient’s headache • Onset • Sudden vs gradual • What were they doing when they headache started? • Intensity/severity • ? Worst ever • Location • Uni or bilateral, frontal/occipital • Pattern • Recurrent/previous similar headaches vs new onset • Improving/worsening • Worse at particular time of the day? • Associated features • • • • • • • Fever Nausea/vomiting Visual changes Photophobia Neck pain Loss of consciousness/syncope Focal neurological deficit Examination • Vital signs • Temperature, BP • Full and thorough neurological examination • Cranial nerves including fundoscopy • Limb neurology • Gait • Skin • ? Rash • Look for signs of meningism • Neck suppleness/movement • Kernigs: with patient flat bend thigh/knee to 90 degrees, positive if painful to straighten knee • Brudenskis: involuntary lifting of the legs when lifting a patient's head off the examining couch, with the patient lying supine. • Also should include….. • • • • Eye examination ENT examination Dental/TMJ examination Temporal artery palpation if indicated Investigations • Most patients with a benign cause for their headache require no investigations • Further workup might include….. • Blood tests • Particularly looking at inflammatory markers (WCC, CRP, ESR) • Lumbar puncture • Neuroimaging • CT (with or without contrast) • MRI/MRA Notes on a few of the big players….. Migraine • May be preceded by an aura (10-20%) • Typically visual symptoms: eg - scintillating scotoma • More common in females, often have family hx • Typically • Recurrent in nature • Same or similar onset/severity/triggers/associated symptoms • • • • • Gradual onset Moderate to severe intensity Frontal, unilateral, pulsating in nature Accompanied by photo/phonophobia, nausea/vomiting Lasts up to 72 hours • Sometimes may be preceded or accompanied with focal neurological deficits • But this is a diagnosis of exclusion! Cluster headache • Typically affects young men • Intense unilateral periocular headaches that come in clusters with complete recovery between attacks • Eg: 30-90 mins 1-6x/day for 2 weeks • Often associated with unilateral autonomic symptoms • Ptosis/miosis • Lacrimation/rhinorrhoea/nasal congestion • Conjunctival injection • High flow oxygen therapy is a very effective treatment • Also sumitriptan Subarachnoid haemorrhage • Typically sudden onset, worst ever headache • “thunderclap” • Most commonly occiptonucal in location • Can just present with sudden onset neck pain • Can be associated with syncope, vomiting, decreased LOC, focal neurological deficit • ½ will present to ED with a completely normal neurological examination • A “sentinel bleed” (ie: leak) can completely resolve with no or very little analgesia • The next bleed is generally catastrophic • Standard of diagnostic care at present is a CT head followed by a LP at least 12h after onset of headache if this is normal (looking for blood in the CSF/xanthochromia) • *watch this space: there is some evidence that if the CT is performed within 6h of onset of headache, that a normal CT may be enough to rule out SAH Tumours • Around 50% of people with brain tumours will have no headache • May present with signs of increased ICP • Worse in the morning • Associated vomiting • Can present with seizure • May have associated neurological deficits • Focal deficits, visual symptoms, ataxia • Can be uni or bilateral, continuous or intermittant • Think of this if a patient has presented with a subacute onset of worsening headaches unlike those experienced before Temporal arteritis • Usually occurs in women >50 years • Typically unilateral piercing temporal pain with tenderness over the (often non-pulsitile) temporal artery • May have associated claudication symptoms • TMJ pain with chewing • • • • Strongly associated with polymyalgia rheumatica Inflammatory markers (ESR/CRP) typically raised Diagnosis is by temporal artery biopsy Failure to diagnose and treat (with high dose steroids) can lead to blindness (ischaemic optic neuritis)