RTA - European Society for Paediatric Nephrology
advertisement

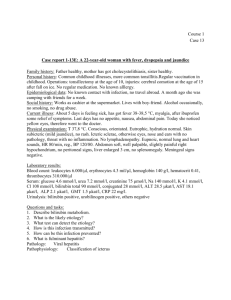
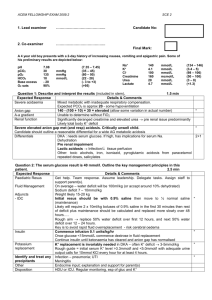
Electrolytes and pH disturbancies: clinical signs to make a correct diagnosis and an early treatment Alberto Bettinelli Departments of Pediatrics Leopoldo Mandic Hospital, Merate (LC) Italy Case 1 An Albanese child… Clinical presentation • Male. Age: 2 years and 3 months • Poor clinical condition with signs of dehydration and chronic malnutrition (hypotrophia of muscles with abdominal protrusion, hypotonia, psychomotor retardation) • Polypnea, 60/min • Weight Kg. 7.610, lenght cm. 75 (< 3° percentile) • Blood pressure 68/34 mmHg Emergency measures • - adequate periferal perfusion with administration of isotonic saline (20 ml/kg/h) • - delivery of 02 First biochemical examinations • venous pH 7.101 • plasma bicarbonates, 5.0 mmol/l • pC02 16.2 mmHg QUESTIONS ? 1) Is it a simple metabolic acidosis? 2) Is it a metabolic acidosis with normal plasmatic anion gap? Is it a simple metabolic acidosis? • Predicted metabolic and respiratory compensations to simple primary acid-base disturbances • (Bianchetti MG and Bettinelli A in Comprehensive Pediatric Nephrology, Geary DF and Schaefer F Ed; Mosby Elsevier 2008:395-432) • Metabolic Acidosis: Primary Change HCO3• Compensatory response: pCO2 by 1.3∆ mm Hg for 1.0 mmol/L* in HCO3• ∆ range approximately ± 3 mm Hg; * from 25 mmol/L; range approximately ± 2.0 mmol/L; from 40 mm Hg. First biochemical examinations • Venous ph 7.101; plasma bicarbonates 5.0 mmol/l; pC02 16.2 mmHg • • • • ∆bicarbonates: 25-5 = 20 ∆pC02: 20 x 1.3 = 26.0 40-26.0 = 14.0 = expected pC02 The respiratory compensation is appropriate = simple metabolic acidosis After some hours • Venous ph 7.150; plasma bicarbonate 8.7 mmol/l, pC02 26.9 mmHg • Plasma Na 135, K 4.3, Cl 116 mmol/l • Plasma anion gap: • (Nap + Kp) – (Clp + Bicarbonate) = 14.6 • (Ref values 8-18; If you do not include K = 4-14) • Plasma anion gap is normal: the major cause of metabolic acidosis with normal anion gap was excluded (gastrointestinal loss di bicarbonates) Metabolic acidosis with normal anion gap • - Losses of bicarbonate HCO3- • - intestinal: diarrhea, surgical drainage of the intestinal tract, gastrointestinal fistulas resulting in losses of fluid rich in HCO3-, patients whose ureters have been attached to the intestinal tract - urinary: carbonic anhydrase inhibitors (e.g.: acetazolamide), proximal renal tubular acidosis (= type 2) • • - Failure to replenish HCO3- stores depleted by the daily production of fixed acids • • - distal renal tubular acidosis (either classic, also called type 1 or type 4) - diminished mineralocorticoid (or glucocorticoid) activity (adrenal insufficiency, selective hypoaldosteronism, aldosterone resistance) - administration of potassium sparing diuretics (spironolactone , eplerenone, amiloride, triamterene) • • - Exogenous infusions • • - Amino acids like L-arginine and L-lysine (during parenteral nutrition) - HCl or NH4Cl - Rapid administration of normal saline (= NaCl 9 g/L) solution (= “dilutional” metabolic acidosis) • Other questions 3) How is the urinary ammonium (urinary anion gap)? 4) Can you perform some simple investigations? Response: question 3 3) How is the urinary ammonium (urinary anion gap) ? • Urinary anion gap: in non renal metabolic acidosis urinary Cl>Na+K; this is because urinary ammonium accompanies Cl • In this case: Cl 23; Na 20; K 11.4 mmol/l • Na + K – Cl = 31.4 -23 = + 8.4; a positive net charge indicates an impaired ammonium secretion and, therefore, impaired distal acidification of renal tubule Response to question 4) 4) Can you perform some simple investigations? Other investigations • Renal ecography demonstrated nephrocalcinosis • Urinary pH; not very simple to detect with the usual methodology • Our urinary pH (with a plasma venous pH between 7.101 and 7.150): 7.248-7.456 • Diagnosis of DISTAL RENAL TUBULAR ACIDOSIS (DRTA, type 2) Administration of bicarbonate? • - Possible benefits: metabolic advantage of faster glycolysis with better availability of adenosine triphosphate in vital organs, and improved cardiac action • - Risks: extracellular fluid volume expansion, tendency towards hypernatremia and devolepement of hypokalemia and hypocalcemia • - In this case a correction was started slowly: • Body weight x 0.5 (desired bicarbonate- current bicarbonate): 7.6 x 0.5 (9-5) = 15.2 mmol in some hours in normal saline Treatment • • • • Glucose 5% = 1.800 ml/mq/day NaCl = 60 mEq/mq/day KCl = 40 mEq/day NaHC03- = 20 mEq/day • - Than orally: NaHC03-, 1 gr/kg/day + potassium citrate 1 mEq/kg/die • After 7 days: venous pH 7.310; plasma bicarbonates 21.3 mmol/l; pC02 43.6 mmHg Audiometry evaluation • The first investigation (the test tones were warble tones) was in the normal range. • Further audiometry evaluations are required Molecular diagnosis • …the molecular diagnosis was of distal renal tubular acidosis due to an homozygous mutation in the ATP6V1B1 gene ( homozygous L81P mutation) • This mutation is known to be associated with neurosensorial deafness (Tasic V et al: Atypical presentation of DRTA in two siblings. Pediatr Nephrol 2008; 23:1177-81) - Laboratory investigations revealed proximal tubular dysfunction that disappeared some months after the beginning of the treatment Case 2 • The child was in apparent good health up to the age of 9 months when he was admitted to the Hospital for gastroenteritis • In the urgency plasma Potassium was 1.7 mmol/l • He presented a cardiac arrest followed by immediate reanimation. • After this episode he did not present any cardiac or neurologic complications • When he left the Hospital, the child was in good clinical conditions and his plasma K was between 2.9-3.0 mmol/l Interpretation • The severe hypokalemia was considered the cause of cardiac arrest (probably associated with cardiac arrhythmias) • Rotavirus was identified as the pathogenetic factor of the severe gastroenteritis At 10 years of age • He was admitted to the Hospital for a suspicious of appendicitis. His plasma potassium was 2.3 mmol/l • After surgery his plasma potassium levels persisted at low levels (2.5 e 3.0 mmol/l ) • In this case the origin of hypokalemia was investigated • New hypothesis?? • It appeared as a chronic condition of hypokalemia How is blood pressure? • His blood pressure was always normal: 90/60 mmHg = in the reference range • We can exclude hypokalemia associated with high blood • • pressure (often linked with metabolic alkalosis; total K+ body content normal) - renin: primary aldosteronism (either hyperplasia or adenoma), apparent mineralocorticoid excess (= defect in 11--hydroxysteroid-dehydrogenase), Liddle syndrome (congenitally increased function of the collecting tubule sodium channels), dexamethasone-responsive aldosteronism (synthesis of aldosterone promoted not only by renin but also by adrenocorticotropin), congenital adrenal hyperplasia (11--hydroxylase or 17--hydroxylase deficiency), Cushing disease, exogenous mineralocorticoids, licoriceingestion (= 11--hydroxysteroid-dehydrogenase blockade) - or renin: renal artery stenosis, malignant hypertension, renin producing tumor Hypokalemia associated with normal-low blood pressure • • • • • • • • • • • • • True potassium depletion (= total K+ body content reduced) Extrarenal “conditions” - Prolonged poor potassium intake, protein-energy malnutrition - Gastrointestinal conditions: gastric (associated with alkalosis), vomiting, nasogastric suction; small bowel ; associated with acidosis: biliary drainage, intestinal fistula, malabsorption, diarrhea, congenital chloride diarrhea - Acid-base balance unpredictable: bowel cleansing agents, laxatives, clay ingestion, potassium binding resin ingestion - Sweating, full thickness burns Renal “conditions” - Interstitial nephritis, post-obstructive diuresis, recovery from acute renal failure - With metabolic acidosis: renal tubular acidosis (type I or II), carbonic anhydrase inhibitors (e.g.: acetazolamide), amphotericin B, outdated tetracyclines - With metabolic alkalosis: - Inherited conditions: Bartter syndromes, Gitelman syndrome, and related syndromes - Acquired conditions: normotensive primary aldosteronism, loop and thiazide diuretics, high dose antibiotics (penicillin, naficillin, ampicillin, carbenicillin) Main investigations • The child was in good clinical conditions; his growth was between the 30-50° percentile • Main biochemical data: • - plasma K, 2.5-2.9 mmol/l ↓; FeK 39-45% ↑ • - plasma bicarbonates 28-35 mmol/l ↑ • - plasma Na, 140-141 mmol/l; FeNa 1.4-1.8% ↑ • - plasma Cl, 94-99 mmol/l; FeCl 2.5-2.7 ↑ • - plasma Mg 0.5-0.6 mmol/l ↓; FeMg 4.7-5.4% ↑ • - urinary calcium/creatinine 0.001 mg/mg ↓ ↓ • - plasma renin activity, 11-15 ng/ml /h (ref. < 5) ↑ • - plasma aldosterone, 75-143 pg/ml (ref. 50-300) Main probable diagnosis • GITELMAN SYNDROME: - hypokalemia with increased FeK and increased FeCl • - metabolic alkalosis • - hypomagnesemia • - hypocalciuria • - hyper-reninemia associated with normal blood pressure • - usually diagnosis during schoolife and young adults • - some patients with growth failure Differential diagnosis • BARTTER SYNDROME TYPE III: - hypokalemia with increased FeK and increased FeCl • - metabolic alkalosis • - NORMO-MAGNESIEMIA (sometimes hypomagnesemia, 39% of cases*) • - VARIABLE CALCIURIA (sometimes hypocalciuria 8% of cases*) • - hyper-reninemia associated with normal blood pressure • - usually diagnosis during early childhood • - half of the patients with growth failure *Konrad M et al; J Am Soc Nephrol 2000; 11:1449-59 Thiazide test (Colussi G, Bettinelli A, 2007) • A wash out period of at least 7 days was allowed between withdrawal of any therapy and thiazide test; however, oral KCl and Mg salts, if already in use, were maintained and stopped the day before the test • Thiazide test: after un overnight fast, the patients were invited to drink tap water (10 ml/kg b.w.) to facilitate spontaneous voiding Hydrochlorothiazide (HCT) 1 mg/kg b.w. - 60 - 30 Mean of the two urinary values 0 30 60 90 120 150 Maximum urinary value obtained after HCT Plasma Na, K, Cl and creatinine 180 DFECl • maximal excretion of FECl at any time after HTC administration • minus the mean of the two basal FECl DFECl: 0.60% ∆ Fractional Chloride Excretion, % 20 10 5 2 1 0.5 0.2 Bartter Control Gitelman Syndrome Subjects Adults Children Syndrome Molecular evaluation • The child presented two heterozigous mutations on the gene SLC12 A3 • Therapy consisted of oral KCl supplementation • QTc was 0.44” • No other cardiac complication was reported Mutations in the SLC12A3 gene found in the Italian population 1 2 R3 4 5 6 7 8 9 10 11 12 COOH NH2 Mutations demonstrated in patients subjected to HCT test • • • • Severe syncope and sudden death in children with inborn salt-losing hypokalaemic tuulopathies. Cortesi C, Bettinelli A, Bianchetti M.; Nephrol Dial Transplant 2005; 20: 1981-3 - 249 children were evaluated with inborn saltlosing hypokalaemic tubulopathies - 19 European paediatric kidney disease specialists - Four patients died suddendly and 3 had severe syncope - These episodes occurred in the context of severe chronic hypokalemia (< 2.5 mmol/l) or were precipitated by acute diseases, which exacerbated hypokalemia (< 2.0 mmol/l) Chronic treatment • - KCl supplementation • - Antialdosteronic drugs (Spironolactone, amiloride) Final message • In patients with inborn salt-losing tubulopathies, diarrhoea or vomiting may cause severe, hazardous hypokalemia (< 2.0 mmol/l) • A prompt electrolyte and fluid repair is of paramount importance