Proyecto Áncora y CESFAM Madre Teresa de Calcuta
advertisement

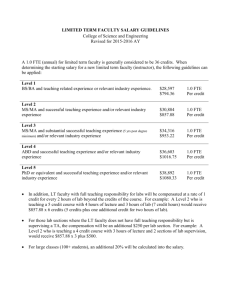
Proyecto Áncora & CESFAM San Alberto Hurtado Some reflections August 2008 Thomas Leisewitz Family Medicine Department Pontificia Universidad Católica de Chile tl@med.puc.cl Background Family & Community Medicine Programme: postgraduate training of family physicians from 1993 Collaborative work with Municipalities and Health Authority at SSMSO Health policy initiatives: Family Health Centres 1997/98 Political willingness: management of public funds by private not-for-profit institutions Health sector reform process based on primary care?: Family Health Centres Family Health Centres ‘Registered’ population ‘Family Health Plan’ Teamwork Responsiveness and accountability Information systems Local planning Outcome-orientation Coordination in the use of resources Proyecto Áncora. Aim “Contribute to a significative change in primary care, delivering health care services and training professionals with a wide, efficient and human perspective, in a replicable way” Proyecto Áncora. Objectives Operation of 3 Health Centres Continuing evaluation of the model Encourage professionals’ and students’ interest in primary care Diffussion of the experience Influence public policy decision-making Proyecto Áncora. Challenge …the implementation of a family health model in primary care through the management of public funding by a private not-for-profit organisation …within the scope of the aim and objectives of the Ancora Project Clinical model: some elements The person at the centre The family as a fundamental referent The community and its role as a social support network Keeping people healthy (Health Promotion) Continuity of care Personalised relationship with providers Responsiveness Teamwork Biopsychosocial approach What we have… until now! A team 22.703 people registered (22.076 validated) A building and equipment A budget An organisation of the main processes A proposal of implementation of the model Our team 15 FTE doctors 5 FTE nurses 4 FTE midwives 2 FTE social workers 4 FTE clinical psychologists 1 FTE dietician 4 FTE dentists 9 FTE administrative staff 8 FTE clinical assistants 4 FTE dental assistants The building Some health indicators used for allocating resources Coverage of preventive services Ultrasound for gall bladder disease Mammography for breast cancer Chronic disease management BP control in hypertensive patients Blood glucose control in diabetic patients Access to dental care Psychomotor development in children Our budget Per-capita value 2008: $ 2,826 Total per-capita funding 2008: M$ 536 University funding 2008: M$ 76 Total budget 2008: M$ 612 Expenditures Expenditures 55% salaries 22% outsourced services: laboratory, cleaning and security 15% pharmacy & others 4% electricity, water, heating, etc. How are we organised? 2 sectors: multidisciplinary teams delivering services for 10 000 people each (green & blue) 1 clinical support team: vaccination, pharmacy, laboratory, diagnostic procedures, special programmes (eg respiratory diseases) 1 administrative support team: call center, IT, secretarial support, etc. Work areas Family approach Patients lists for each physician Families assigned to an specific team Relationship with the community Diffusion and inscription Health promotion Implementation of services included in the ‘Health Plan’ Process design and re-design and the relationship with ECR The teaching model (especially for 2008) And what about evaluation? Evaluation. Methodology Primary Care global index -Continuity -Access -Resolutividad -Preventive care –Health Promot -Participation -bps & family approaches -Direct -Savings -Appointments - Referals -Out-of-pocket payments -Patients’ waiting times Effectiveness Costs Centre 1 Centre 2 Cost-Effectiveness analysis Δ Effectiveness Effectiveness Centre 1 Effectiveness Centre 2 Δ Costs Costs Centre 1 Costs Centre 2 Incremental Cost-Effectiveness Ratio Costs (Centre 1- Centre 2)/ Effectiveness (Centre1 – Centre2) = Δ C / Δ E Results. Effectiveness Total global ponderado Indicadores Objetivos Experiencia Aceptabilidad Total Dimension MTC Comp MTC Comp MTC MTC Comp MTC Continuidad 0,1702 0,1699 0,1238 0,0837 0,2339 0,1562 0,5279 0,4098 0,0598 0,0464 Enfoque Prev y prom. 0,4200 0,3780 0,0909 0,0710 0,1322 0,1022 0,6432 0,5512 0,0837 0,0717 Resolutividad 0,3758 0,4008 0,1084 0,0616 0,1361 0,0861 0,6202 0,5484 0,1073 0,0949 Enfoque BPS y familiar 0,0217 0,1261 0,1936 0,1340 0,2512 0,1550 0,4665 0,4151 0,0339 0,0301 Accesibilidad 0,3004 0,2429 0,1231 0,0097 0,4235 0,2526 0,1669 0,0995 Participacion 0,5160 0,3090 0,5160 0,3090 0,0604 0,0362 0,5119 0,3788 Comp Total ΔE = ΔE = 0, 1317 Comp 0,1331 Results. Direct costs Tipo de Costo Item Origen MTC Comp. Delta % Médicos gasto per cápita del centro 625 23,55% -176 -60,41% -12 -2,68% -39 -107,02% ΔE =398 13,44% 2652 2027 2594 1854 58 173 291 467 SAPU 115 148 Urgencia 170 307 6 12 448 460 81,9 173,1 Exámenes 191,1 151,5 Consultas 175,0 135,5 36 75 36 75 2960 2562 Gasto operacional del centro no docente Gasto administración central (gasto) per cápita del sistema Interconsultas no pertinentes gasto de bolsillo Medicamentos Tiempo destinado a buscar cuidado Pérdida de tiempo per cápita TOTAL ($2006) Todas las cantidades son percapita mensuales Evaluation. Some conclusions The evaluated Ancora health center (MTC) was more expensive and more effective than the comparator. The proposed effectiveness indicator seems comprehensive, though the difficulties in understanding its practical implications. Patient perspective stands as a key element for the proposed evaluation model, establishing significant differences between the analysed centres. The difference in the estimated per-capita cost is smaller if a social perspective (modified) is adopted rather than just considering the operational expenditures. Evaluation. Some conclusions The Ancora center saves money to the whole health system, although it does not fully compensate the increased operational cost. The effectiveness indicator is consistently higher for the Ancora health center, being unaffected by the different weights of the considered dimensions in a sensitivity analysis. The family health model is complex, so do its evaluation. However, the richness of this evaluation model could give great information to health teams and managers for the betterment of the model. Some reflections After four years, we have realised that our main strength is the way how each team (and each individual professional) establish a relationship with its patients and families The evaluation from the patients’ perspective has consistently been our best evaluated dimension Some reflections Financing Long-term feasibility (political willingness) Non-enveloped per-capita allocations versus specific allocations by each programme (change during 2007) Performance management Managing performance with a limited number of indicators Is it possible to define a common set of indicators for primary care organisations? Some reflections The Family Health Model What model do we want to implement? How should it be evaluated? Information management in primary care the challenges of the electronic clinical record (its full potential)