Sleep Pods for Strategic Naps - Stanford University School of Medicine
advertisement

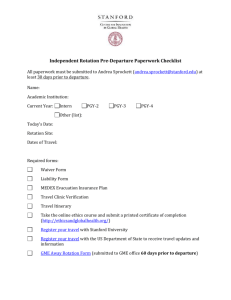
Thinking Outside the Box: The Use of Sleep Pods for Strategic Naps for Fatigue Management – Does it Work? Conference Session: SES022 2012 ACGME Annual Education Conference Nancy Piro, PhD Program Manager/Education Specialist and Ann Dohn, MA, DIO Department of Graduate Medical Education Stanford Hospital & Clinics Department of Graduate Medical Education (GME) Conflict of Interest • No conflicts of interest to report Department of Graduate Medical Education (GME) Session Objectives At the end of this session, participants will be able to have: – an increased awareness of the research on the effectiveness of naps in resident training programs – an increased understanding of the effectiveness of innovative solutions such as sleep pods to mitigate resident and fellow fatigue – A better understanding of how to (and how not to) operationalize a nap and fatigue management strategy in academic GME settings Department of Graduate Medical Education (GME) Setting the Stage - History • • • • Libby Zion case July 2003 ACGME Duty Hours Requirements IOM Report Education for faculty and residents on “The Effects of Fatigue & Fatigue Mitigation” • July 2011 New ACGME Duty Hour Requirements • Strategic Napping Department of Graduate Medical Education (GME) Libby Zion Case/Law • The Libby Zion law is a regulation that limits the amount of resident physicians work in New York State hospitals to roughly 80 hours per week. • The law was named after Libby Zion who died at the age of 18 under the care of what her father believed to be overworked resident physicians and intern physicians. • In July 2003 the Accreditation Council for Graduate Medical Education (ACGME) adopted similar regulations for all accredited medical training institutions in the United States. Department of Graduate Medical Education (GME) Libby Zion Case/Law (2) • After the grand jury's indictment of the two residents, the New York State Health Commissioner David Axelrod decided to address the systemic problems in residency by establishing a blue-ribbon panel of experts headed by Bertrand M. Bell, a primary care physician at the Albert Einstein College of Medicine in the Bronx. • Bell was well known for his critical stance regarding the lack of supervision of physicians-in-training. • The committee evaluated the training and supervision of doctors in the state, and developed a series of recommendations that addressed several patient care issues, including restraint usage, medication systems, and resident work hours. Department of Graduate Medical Education (GME) Libby Zion Case/Law (3) • In 1989, New York state adopted the Bell Commission's recommendations that residents could not work more than 80 hours a week or more than 24 consecutive hours and that attending physicians needed to be physically present in the hospital at all times. • Hospitals instituted “night floats” to spare their colleagues, allowing residents to adhere to the new rules. Periodic followup audits have prompted the New York State Department of Health to crack down on violating hospitals. – Similar limits have since been adopted in numerous other states. • In July 2003 the Accreditation Council for Graduate Medical Education (ACGME) adopted similar regulations for all accredited medical training institutions in the United States. Department of Graduate Medical Education (GME) New ACGME Requirements Effective July 1, 2011 Alertness Management VI.C.1. The program must: a) educate all faculty members and residents to recognize the signs of fatigue and sleep deprivation; b) educate all faculty members and residents in fatigue mitigation processes; and, c) adopt fatigue mitigation processes to manage the potential negative effects of fatigue on patient care and learning, including naps and back-up call schedules. VI.C.2. Each program must have a process to ensure continuity of patient care in the event that a resident may be unable to perform his/her patient care duties. VI.C.3. The sponsoring institution must provide adequate sleep facilities and/or safe transportation options for residents who may be too fatigued to safely return home. Department of Graduate Medical Education (GME) 2011 ACGME REQ’s 2003 ACGME LIMITS 2008-IOM RECOMMENDATION Supervision Programs ensure supervision by qualified faculty Supervision standards are set by the Resident Review Committee (RRC); in-house supervision is provided for 1st year residents. Residents and attendings inform patients of their roles, while PD’s & faculty assign documented progressive responsibilities accessible by the healthcare team. Supervisory requirements are defined for residents in program specific policies. Workload Assignments recognize that residents and faculty are both responsible for patient safety and welfare Residents have adequate time for patient care and reflection. Complexity of illness and resident competency is considered in setting appropriate caseloads. Workload is based on patient safety, severity and complexity of patient cases, available support, resident training and education. Maximum Duty Period Length 30 hrs (with 24 hrs to admit patients and 6 hours for transition and educational activities). 16 hrs; extended duty of 30 hrs (with 5 hrs sleep after 16 continuous hrs) only every third night. 16 hrs for first-year residents; 24 hours for other residents. Residents must be informed of alertness strategies, and a nap is strongly recommended after 16 hours of continuous duty. Minimum Time Off Between Scheduled Duty Periods 10 hrs 10 hrs after day duty period; 12 hrs after night duty; 14 hours after extended duty period and no return before 6a.m. the next day. 10 hrs (with minimum of 8 hrs duty-free between duty periods, or 14 hrs duty free after 24 hrs of in-hospital duty). Mandatory OffDuty Time 24 hrs off per week averaged over 4 weeks 24 hrs off per week, no averaging; one week 24 hrs per week averaged over four weeks; no home call on off duty days. Moonlighting Internal moonlighting is considered part of the 80hr weekly limit Internal and external moonlighting are included in the 80-hr weekly limit; approval is required by PD. Internal and ext. moonlighting are included in the 80-hr limit. No moonlighting (GME)weekly allowed for 1st yr. residents CATEGORY Department of Graduate Medical Education “Strategic napping, especially after 16 hours of continuous duty and between the hours of 10:00 p.m. and 8:00 a.m. is strongly suggested.” Department of Graduate Medical Education (GME) Traditional Hospital Fatigue Mitigation Strategies Gurneys Chairs Mattresses Call Rooms Coffee Patio Furniture Beds Floor Futons Department of Graduate Medical Education (GME) Thinking Outside the Box • • • • Looked to Silicon Valley Found “nap pods” being used at GOOGLE Sent resident “spy” to scope out DIO (born in Berkeley) said this is California---why not? • Did internet search – found lots of info Department of Graduate Medical Education (GME) What Does the Research Tell Us? • Emergency Medicine Residents • Sleep Pods – SUNY/VA Department of Graduate Medical Education (GME) Problems with Traditional Approaches • Limited Number of Call Rooms • Distance Between Clinical Areas and Call Rooms • Housekeeping constraints Department of Graduate Medical Education (GME) Looking Outside Medical Settings for Ideas “Napping Gets a Nod at the Workplace” J. Hoffman, 8/30/2010, Bloomberg Business Week • A growing number of companies are encouraging employees to nap at work—and boost their productivity • From Thomas Edison and Winston Churchill to Bill Clinton and George Costanza, the nap has had many famous champions. Department of Graduate Medical Education (GME) Looking outside Medical Settings for Ideas • Ever since sleep scientist David Dinges helped found the modern science of napping in the early '80s at the University of Pennsylvania School of Medicine, short periods of sleep have been shown to improve alertness, memory, motor skills, decision-making, and mood. – All while cutting down on stress, carelessness, and even heart disease. Department of Graduate Medical Education (GME) Looking outside Medical Settings for Ideas • With Americans averaging fewer than seven hours of sleep per night—and around 20 percent suffering from sleepiness during the day, according to a recent Stanford University study—many companies have turned to naps in an attempt to stave off billions in lost productivity each year. Department of Graduate Medical Education (GME) Looking outside Medical Settings for Ideas • Nike workers now have access to nap-friendly "quiet rooms" that can also be used for meditation. • Google, a forerunner in employee perks, has a number of nap pods scattered throughout its Mountain View CA campus. Department of Graduate Medical Education (GME) Department of Graduate Medical Education (GME) Naps Are Not Just for Kindergartners Anymore! Department of Graduate Medical Education (GME) Stanford Nap Research • Objective: Examine whether a 40-minute nap opportunity at 3 AM can improve cognitive and psychomotor performance in physicians and nurses working 12-hour night shifts. Rebecca Smith-Coggins, MD et al.” Improving Alertness and Performance in Emergency Department Physicians and Nurses: The Use of Planned Naps” (2006) Department of Graduate Medical Education (GME) Stanford Nap Research • Methods: A randomized controlled trial of 49 physicians and nurses working 3 consecutive night shifts in an academic emergency department. • Subjects were randomized to a control group (no nap condition - NONE) or nap intervention group (40-minute nap opportunity at 3 AM NAP). Rebecca Smith-Coggins, MD et al.” Improving Alertness and Performance in Emergency Department Physicians and Nurses: The Use of Planned Naps” (2006 Department of Graduate Medical Education (GME) Main Outcome Measures • Psychomotor Vigilance Task • Probe Recall Memory Task • CathSim intravenous insertion virtual reality simulation • Profile of Mood States – Administered before (6:30 PM), during (4 AM), and after (7:30 AM) night shifts. Rebecca Smith-Coggins, MD et al.” Improving Alertness and Performance in Emergency Department Physicians and Nurses: The Use of Planned Naps” (2006) Department of Graduate Medical Education (GME) Methodology • A 40-minute driving simulation was administered at 8 AM and videotaped for behavioral signs of sleepiness and driving accuracy. • During the nap period, standard polysomnographic data were recorded. Rebecca Smith-Coggins, MD et al.” Improving Alertness and Performance in Emergency Department Physicians and Nurses: The Use of Planned Naps” (2006) Department of Graduate Medical Education (GME) Results • Polysomnographic data revealed that 90% of nap subjects were able to sleep for an average of 24.8 minutes (SD 11.1). • At 7:30 AM, the nap group had fewer performance lapses – reported more vigor – less fatigue – less sleepiness Rebecca Smith-Coggins, MD et al.” Improving Alertness and Performance in Emergency Department Physicians and Nurses: The Use of Planned Naps” (2006) Department of Graduate Medical Education (GME) Results • At 7:30 AM, the nap group had fewer performance lapses – tended to more quickly complete the intravenous insertion – exhibited less dangerous driving and display fewer behavioral signs of sleepiness during the driving simulation. • Immediately after the nap (4 AM), the subjects scored more poorly on Probed Recall Memory Rebecca Smith-Coggins, MD et al.” Improving Alertness and Performance in Emergency Department Physicians and Nurses: The Use of Planned Naps” (2006) Department of Graduate Medical Education (GME) The effects of a mid-day nap on the neurocognitive performance of medical interns • Methods: Twenty-nine 1st year medical residents were divided into a nap group of 18 participants and a control group of 11 participants. • Participants were connected to a portable monitoring device prior to their tour of duty so that the occurrence of rolling eye movements, attention failures, could be monitored. Mohammad M. Amin, MD et al. (2011) Department of Graduate Medical Education (GME) The effects of a mid-day nap on the neurocognitive performance of medical interns • At mid-day, both groups underwent cognitive testing with Conner’s Continuous Performance Test (CPT II) and then were placed in a nap pod. • Participants in the intervention group were instructed to nap for up to 20 minutes while controls were prevented from napping. Mohammad M. Amin, MD et al. (2011) Department of Graduate Medical Education (GME) The effects of a mid-day nap on the neurocognitive performance of medical interns • The CPT II was repeated immediately following the 20-minute period and attention failures were recorded until the end of the tour of duty. • Mean outcome parameters were compared across both groups with ANOVA with effect of treatment and baseline covariate using SAS. Mohammad M. Amin, MD et al. (2011) Department of Graduate Medical Education (GME) The effects of a mid-day nap on the neurocognitive performance of medical interns • Conclusion: A mid-day nap can improve attention and cognitive function among first year medical residents. Mohammad M. Amin, MD et al. (2011) Department of Graduate Medical Education (GME) Conclusions from the Research • Naps DO mitigate fatigue and improve cognitive performance overall Department of Graduate Medical Education (GME) How Did We Proceed? • Brainstormed Possible Solutions with: – – – – Sleep Experts Program Directors GMEC Chief Residents Department of Graduate Medical Education (GME) What Did We Decide? • Pilot nap pods to see if they would be a means to enhance strategic napping and mitigate fatigue Department of Graduate Medical Education (GME) Department of Graduate Medical Education (GME) Why Did We Choose Nap Pods? • Could Be Located Almost Anywhere • Didn’t require linen changes – could be wiped down • Had Track Record in Industry and at the VA Department of Graduate Medical Education (GME) Pilot Implementation • Key Considerations: – Where do we locate them? • Call Quarters vs near the ICUs? – How Do We Market Them to the Residents and Fellows? – How Do We Encourage Attending/Faculty Support? – How Do We Evaluate Effectiveness? Department of Graduate Medical Education (GME) Implementation • Installed two trial nap pods – Collaborated with a source of nap pods • One in the Call Quarters • One outside the ICU • Informed GMEC, Program Directors and Residents • Started Gathering Data of Usage • Planned for Survey of Resident Perceptions about the nap pods Department of Graduate Medical Education (GME) Data Gathering • Quantitative Data • Qualitative Data for Analysis Department of Graduate Medical Education (GME) Quantitative Data Department of Graduate Medical Education (GME) Quantitative Data Department of Graduate Medical Education (GME) Quantitative Data Department of Graduate Medical Education (GME) Quantitative Data Department of Graduate Medical Education (GME) Department of Graduate Medical Education (GME) Department of Graduate Medical Education (GME) Department of Graduate Medical Education (GME) Department of Graduate Medical Education (GME) Preliminary Qualitative Survey Results • Pods don’t take the place of beds • Better awareness as to other factors e.g., noise, paging that impact sleep – noise in the hallway – quieter quarters for napping Department of Graduate Medical Education (GME) Takeaways from The Data • ICU Pod is getting more use than the one in the Call Rooms – Most Used 12-4 AM • Pods don’t take the place of beds • Better awareness as to other factors e.g., noise, paging that impact sleep Department of Graduate Medical Education (GME) What Could we Have Improved On? • Better Education • Better Marketing • More Champions Department of Graduate Medical Education (GME) So….Are Nap Pods A Successful Mitigation Strategy? • 10 months into the pilot . . . – Preliminary Findings • Pods do work • Pods do not take the place of beds • Pods do work better for mitigation during duty hours (especially between 4-6AM) than at the end of the duty period • Need to market to the residents and fellows • Need to empower Faculty Champions – Upcoming Meeting with Chief Residents Department of Graduate Medical Education (GME) Questions Department of Graduate Medical Education (GME)