Near Drowning - Calgary Emergency Medicine
advertisement

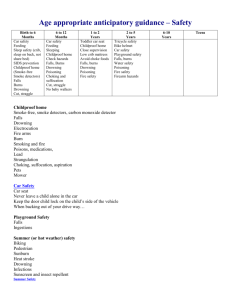
Near Drowning Resident Rounds June 26, 2003 Robbie N. Drummond Not Waving but Drowning Stevie Smith Nobody heard him, the dead man, But still he lay moaning: I was much further out than you thought And not waving but drowning. Poor chap, he always loved larking And now he's dead It must have been too cold for him his heart gave way, They said. Oh, no no no, it was too cold always (Still the dead one lay moaning) I was much too far out all my life And not waving but drowning. IV. DEATH BY WATER (from the Wasteland, T.S. Eliot) PHLEBAS the Phoenician, a fortnight dead, Forgot the cry of gulls, and the deep seas swell And the profit and loss. A current under sea Picked his bones in whispers.As he rose and fell He passed the stages of his age and youth Entering the whirlpool. Gentile or Jew O you who turn the wheel and look to windward, Consider Phlebas, who was once handsome and tall as you. The Tempest by Willy Boy the Spear Shaker Act I Scene ii ARIEL sings] Full fathom five thy father lies; Of his bones are coral made; Those are pearls that were his eyes: Nothing of him that doth fade But doth suffer a sea-change Into something rich and strange. Sea-nymphs hourly ring his knell Hark! now I hear them,--Ding-dong, bell. FERDINAND The ditty does remember my drown'd father. YODA’s 7 QUESTIONS ABOUT DROWNING There are a lot of terms to describe drowning how do I wade through them all? What is the real difference between fresh and salt water drowning? How common is drowning are there any preventative measures to be taken to avert death by water? There is a drowning victim in the ED what are the factors that suggest he will survive? What is the best approach to resuscitating a drowning victim? What about the prophylaxis measures previously taken, steroids, hyper therapy, antibiotics....etc.? Survivors of drownings usually are hypothermic what is the relation between hypothermia and drowning? There are many terms to describe drowning how do I wade through them all? gets complicated..... Drowning, near-drowning, drowning with/without aspiration, dry drowning, wet drowning, secondary drowning, submersion vs immersion, immersion syndrome, ORLOWSKI feels too complicated was supposed to imply prognosis but does not Drowning “ suffocation by immersion or submersion in any liquid medium, caused by the entrance of liquid in the airways that partially or fully compromises ventilation or oxygen exchange” basic definitions drowning death within 24 hours of submersion near drowning death after 24 hours of submersion secondary drowning death from a complication of submersion one author secondary drowning cause of death not related to water (eg MI) drowning with or without aspiration immersion vs submersion partially vs totally covered aspiration of other fluids bodily etc wet vs dry drowning 10% no fluid found in lungs severe laryngospasm, hypoxia, convulsion and death one author “dry drownings probably do not exist.... if there is no water in lungs victim probably not alive when entered water”..... A la Brian Jones of the Stones.... It was Mick and Keith, the glimmer twins, don’t you know it? 13 % of all drownings happens after precipitating event drugs 36% (usually alcohol) convulsion 18 % trauma 16 % cardiopulmonary 14% SCUBA 3 % others 11 % My mother told me to splash water on my face before..... Immersion Syndrome syncope provoked by arrhythmia sudden contact with water at least 5 degrees less than body temperature syncope loss of consciousness and secondary drowning massive release of adrenaline reduced by wetting face and head before entering water How common is drowning are there any preventative measures to be taken to avert death by water? 90 % of all drowning deaths occur within 10 meters of safety Some watery numbers 500,000 per year worldwide third most common cause of unintentional death 10 saves and five near drownings for every drowning 1996 62,747 rescues 55-60% less than 20 years of age African-Americans two time rate of Caucasians males five times as often as females costs 6.5 billion buckaroos in US alone bimodal distribution toddlers less than 2 and teenage boys 10 - 19 years teenager (boys) risk taking, alcohol factor 60% of time bathtubs usual site under one year of age many as a result of abuse bucket- related deaths older toddlers pools children and adolescents fresh water POOLS 50, 000 new pools built every year in USA 2.2 million residential pools 2.3 million nonresidential pools already in existence in temperate areas of USA 70 - 90 % of drowning occur in pools PUBLIC HEALTH proper pool fencing and supervision training in swimming and water safety essential not leaving child unattended near tub or pool personal flotation devices while boating proper training, SCUBA boating etc solar blankets support weight of toy not children hides drowning child citizens trained in CPR avoidance of alcohol PREVENTION the key to minimizing morbidity is successful prevention AAP 23 recommendations swimming lessons a good idea but sometimes children not aware of their skill level and parents not cautious enough RISK FACTORS FOR SUBMERSION ACCIDENTS , seizures, trauma, Etoh, hyperventilation, drugs of abuse, hot tubs, hypothermia, cvs disease, child abuse, diabetes, suicide inability to swim 53% of individuals with a submersion incident over age 26 blood etoh >100 9% of suicides due to drowning Time of day: toddler drowning : meal preparation times early evenings What is the real difference between fresh and salt water drowning? animal models (ie threw man’s best friend in water to see what happens) struggle small amounts fluid hypopharynx laryngospasm swallowing water laryngospasm abates aspiration large amounts water vomiting aspiration of gastric contents evolving hypoxemia , circulatory collapse myocardial damage, and multiorgan failure ischemic brain injury....death the Pacific vs Georgian Bay for many years suggested difference between fresh and salt water drowning give dogs 44 ml /kg fresh water causes potassium disturbance previous theory was fresh water more hypotonic hemodilution hyper volemia, red cell rupture dilution of pulmonary surfactant alveolar collapse sea water hypovolemia, and increased electrolyte hemoconcentration fluid movement from intravascular to alveoli In reality.... more than 11 ml per kg for change in blood volume only 15% who die in the water aspirate more than this quantity most less than 4ml/kg 22 ml/kg for changes in electrolytes in a study by spilzman 1994 187 drowning victims had no electrolyte abnormality seawater drowning does not cause hypovolemia freshwater drowning does not cause hypervolemia, hemolysis, or hyperkalemia no difference from clinical point of view no difference fresh vs salt water most immediate cause is hypoxia and metabolic acidosis both produce surfactant destruction alveolitis, noncardiogenic pulmonary edema disruption of gas exchange increased shunt leading to profound hypoxia as little as 1 ml /kg aspiration profound alterations in gas exchange decreased compliance cerebral hypoxia is the final common pathway resp disturbance more on amount than type of water 2 small points sometimes physiologic changes many hours after insult water may be contaminated with chemicals, bacteria, sand etc. DEAD SEA Dead Sea unless you drown in the dead sea (Yagil et al arch In Med 1985) one case hypercalcemia and hypermagnesemia What is the best approach to resuscitating a drowning victim? drowning victims present risk to rescuer approach with caution or intermediate object instinctive drowning response drowning victims unable to call for help upright position slapping or thrashing water children 10 - 20 seconds adult up to 60 seconds CPR ASAP SVP first description of CPR 1600’s : Paracelcus a Swiss physician inserting fireplace bellows in the victim’s mouth or nostrils always remember underlying causes for drowning caution re neck injuries citizens trained in CPR in water CPR usually ineffective and dangerous delay in CPR prolongs hypoxia because circumstance are never clear resuscitation should always be initiated in the field drowning victims swallow much more water than they inhale no attempt to remove water from lung great quantities of water in stomach likely to aspirate Heimlich himself suggested his maneuver to expel water from lungs,,,, counterproductive gastric acid aspiration from abdominal pressure lots of fluid in stomach up to 60 % of drowning victims vomit right lateral decubitus head down ? Sellick’s maneuver high risk for vomiting spontaneously or on resuscitation There is a drowning victim in the ED what are the factors that suggest he will survive? ORLOWSKI’s 5 unfavourable prognostic factors age of 3 or less submersion > 5 minutes no attempts at resuscitation for 10 minutes coma on admission to ED severe acidosis pH <7.1 lack of controlled studies which factors greatest impact <2.... 90 % recovery >3.... 5 % likelihood of recovery Check out the GCS GCS adds predictability 2-6 hours after if no improvement unlikely to improve if some increase GCS 50% if alertness normal sequelae limited other factors resuscitation > 25 minutes asystole on arrival at hospital GCS < 5 elevated ICP, coma or CPR needed in ED some survival in some individuals with some or all of these factors water temperature, duration and degree of hypothermia the diving reflex, the victim’s age, water contamination, duration of cardiac arrest the speed and effectiveness of initial treatment cerebral resuscitation success of resuscitation major determinant of outcome prognosis response to serial neurologic exams 3 point improvement on GCS on arrival to ICU portends 100 % full recovery in pediatric population conscious on arrival excellent chance of survival CONN scale alert 100%’ blunted mortality rate 10% comatose greater than 35% The Opposite of Drowning? What is the best approach to resuscitating a drowning victim in ED? continuous cardiac monitoring observation for 4-6 hours if asymptomatic serial ABG measurements (Arterial line) oxygen therapy NGT and FOLEY ETT degree of respiratory distress pa o2 below 50 paco2 greater than 50% Read my lips “it’s the anoxia, stupid!!!” grading system from 1 to 7 based on need for aggressive airway intervention grade 2 only by cannula, grade 4 mechanical pneumothoraces usually as result of baro trauma most significant implication is anoxic ischemic cerebral insult most common cause of late death every effort to maintain oxygenation and prevent cerebral edema r/o other cause of injury toxicological insult spinal injury evaluate and treat associated conditions, hypovolemia, hypothermia, hypoglycemia careful neurological assessment and reassessment both respiratory and metabolic acidosis may still need fluid resuscitation despite pulmonary edema shock is uncommon in drowning do not use furosemide to treat pulmonary edema may need volume in ICU many patients will need PEEP ARDS common in drowning same management as any ARDS patient delayed onset of pulmonary edema (up to 12 hrs) PATHOPHYSIOLOGY although some difference drowning is an asphyxia injury like like hanging, foreign body aspiration, apnea etc noncardiac pulmonary edema, noncardiogenic pulmonary injury, surfactant loss, inflammatory contaminants, and cerebral hypoxia global hypoxic ischemic event affecting brain, lungs, and heart cardiovascular function usually preserved aggressive pulmonary support is required to prevent long term sequelae of hypoxia optimal treatment for anoxic brain injury remains unclear no prognostic scale accurately predicts long term neurologic outcome Consequences global hypoxia cns dysfunction from initial hypoxic injury increased ICP edema aggressive control of cerebral perfusion pressure does not improve out come CNS damage progresses after circulation reestablished cardiac dysrhythmias : a result of hypoxemia/acidosis low cardiac index elevated right and left heart filling pressures increased SVR renal failure uncommon coagulopathies esp DIC and hemolysis What about the prophylaxis measures previously taken, steroids, hyper therapy, antibiotics....etc.? prophylactic antibiotics of limited use treat when infection antibiotics only if grossly contaminated water contributing to injury is aspiration of sand bacteria algae or particulate matter emesis and chemical irritant corticosteroids of limited use HYPER THERAPY early theory (BOHN Critical care medicine 1986) hyperhydration, hyperventilation, hyperpyrexia, hyperexcitability, hyperrigid suggested use of diuretic, hypothermia, barbituates glucocorticoids barbituate coma, muscle paralysis and monitoring and treating of ICP subsequent reviews failed to show improvement with these protocols most centers no longer use hyper therapy current approach supportive care disposition four groups 1) no evidence of sig. submersion d/c’d quickly cxray and abg unnecessary serial sats reassuring pts without any symptoms and completely normal respiratory status may be discharged with instruction to return immediately if respiratory distress developed 2) asymptomatic after sig. episode observed for four to six hours then d/c’d 3) poor oxygenation mod hypoxemia admitted followed once o2 resolved ....home ??? ICU final group... Intubated: depends on neurological status any respiratory complaints or symptoms, cxray abnormalities, demonstrated oxygen requirement monitored for 24 hours usually in ICU any patient with LOC, cyanosis, or apnea, CPR or resuscitative efforts need to be monitored closely GCS needs to be done sequentially CXRAY 20 % of severe drowning normal cxray typical findings perihilar infiltrates, pulmonary edema Pediatrics peds use fairly aggressive PEEP protocol increased risk of nosocomial infection children larger surface area less fat more prone to hypothermia hypothermia some degree of protection rapid cooling necessary in icy water <5 deg to offer benefit usually severe hypothermia increased mortality large costs realistic goal re prognosis families need time to adjust POOR PROGNOSIS IF: absence of cognitive function / recovery 48 -72 hours seizures beyond 12 hours despite early enthusiasm, ICP monitoring: no benefit CT only helpful if ass’d with other injury MRI day 1 and day 3 change helpful in predicting outcome EEG often obscured by drugs and resuscitation persistent flat tracing attenuated record without med or burst suppression poor prognosis brainstem evoked potential: controversial many confounding factors most useful for predicting outcome is repeated clinical neurological examination Survivors of drownings are often hypothermic what is the relation between hypothermia and drowning? continue resuscitation till core temperature 30 -35degreesC one child recovered successfully after 66 minute immersion in cold water hypothermic protection dependant on slowing cerebral metabolism before irreversible damage works with sudden immersion in very icy water or in victims above water cooling before immersion HYPOTHERMIA definition core temperature less than 35 degrees significant pathophysiology develops below 35 degrees primary direct exposure to cold secondary systemic disorders heat preservation shivering, autonomic and endocrinologic responses.... adaptive behavioral responses 35-32-27....mild, moderate, severe mild 32 -35 32 -35 shivering stops, hr and bp decline, oxygen consumption declines depressed CNS increase metabolic rate & pulse , dysarthria, amnesia, ataxia, apathy moderate 27 - 32 decreased loc and vitals, shivering extinguished, arrhythmias, qt prolonged, j wave (Osborne) cannot rewarm spontaneously cold diuresis Severe Hypothermia severe less than 27 degrees coma and areflexia with profoundly depressed vital signs co2 production decreases 50% for each 8 degrees fall in temperature increase heat loss impaired thermoregulation extreme bradycardia spont VF or asystole coagulopathy prolonged clotting times and platelet dysfunction physiologic changes protein binding increases temp drops drugs ineffective wait with monitoring 60 second before initiating CPR most recommend CPR with PEA even with profound hypothermia pulse oximetry accurate in hypothermic patients caution irritating heart in central line insertion most rhythms revert spontaneously with rewarming most VF refractory until rewarmed three shocks trial if unsuccessful rewarm CPR attempt at higher temperature changes in hypothermia tachycardia disproportionate to temperature suspect hypoglycemia hypovolemia or OD hyperventilation suggests A CNS system lesion systemic acidosis DKA or lactic acidosis cold induced rectus spasm and ileus may mask or mimic an acute abdomen need core temperature anemia is masked because hematocrit increase 2% per 1 degree drop in temperature leukocytes sequestered active rewarming passive vs active warming passive noninvasive involves simply covering the patient in a warm environment active rewarming if cvs instability temperature less than 32.2 active core rewarming heated humidified air inhalation, heated infusion lavage, extracorporeal rewarming Invasive techniques thorocostomy tube irrigation IV fluids 40- 42 degrees double catheter peritoneal lavage 2 liters of 40 -45 degrees NS suction after 20 minutes extracorporeal rewarming cardiopulmonary bypass arteriovenous and venovenous rewarming hemodialysis lifesaving in cardiac arrest situations caution: drop in core temp after initiation of rewarming temperature equilibration circulatory return of cold peripheral blood to the core overwhelms a depressed cvs system vasoconstricted skin prone to burning caution with warming extremities What is the Diving Reflex? mammalian response protective bradycardia shunting blood to brain and heart victims age ration of body mass to surface area development of hypothermia hypothermia more protective in children than the diving reflex water must be 10 degrees or colder sudden immersion in cold water can cause ventricular fibrillation controversy over diving reflex breath holding intense vaso constriction bradycarda decreased Cardiac output and increased MAP selective vasoconstriction and heart and CNS perfused breath holding reduced when children submerged in cold water Answers to Yoda’s seven questions drowning is a form of asphyxia main injury is anoxia and its consequences there is no clinical difference between fresh and salt water drowning 90% of drowning occurs within 10 meters of safety prevention is the key level of consciousness on presentation to the ED best prognostic indicator followed by sequential neurologic assessments main features of management is aggressive respiratory support prophylaxis is not indicated the usual dicturm applies the patient is not dead till he is warm and dead Yoda’s real feeling about water Nothing in the world is more flexible and yielding than water. Yet when it attacks the firm and strong none can withstand it, because they have no way to change it. So the flexible overcome the adamant, the yielding overcome the forceful. Everyone knows this, but no one can do it. This is why the sages say those who can take on the disgrace of nations are leaders of lands; those who can take on the misfortune of nations are rulers of the world. True sayings seem paradoxical. References DROWNING Pediatric clinics of North America June 2001Orlowski et al EMR June 1997Schwab et al Emergencies of Summer NEAR DROWNING Critical Care Clinics April199 Sachdeva SUBMERSION AND ASPHYXIAL INJURIES Ibsen and Kock Critical Care medicine Nov 2002 TINTINELLI’s 2002 Rosen’s 2002 EMERGENCY MEDICINE SECRETS THIRD EDITION Markovchick 2003+ the (deep) end