Postmastectomy Pain Syndrome
advertisement

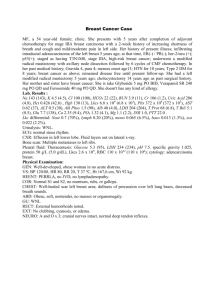
Postmastectomy Pain Syndrome May 21st, 2015 Leslie S. Cavazos, MD, PGY-4 KUMC Department of Rehabilitation Grand Rounds There are no financial disclosures or affiliations to report. Breast cancer The most common cancer in women worldwide. Greater than one million new cases diagnosed each year. The five year overall survival of patients with a diagnosis of primary breast cancer has increased to 85%. [9] Introduction to PMPS Postmastectomy pain syndrome (PMPS) is classified as a type of chronic neuropathic pain disorder. It can occur after breast cancer procedures; frequently with surgeries that remove the upper outer quadrant of the breast and/or axilla. PMPS can either regress or progress, it is not a static condition. Effects of PMPS The pain related to postmastectomy syndrome can be severe enough to: Affect one’s ability to complete ADLs Cause a sleep disturbance Lead to adhesive capsulitis Lead to complex regional pain syndrome Incidence The incidence of PMPS ranges from 20 to 72%, including nerve injury or impairment, and the chronic pain that results from injury. This range of values can be explained by the variation of definitions used to define PMPS. There is no standard definition of PMPS. Inclusion criteria are vague. Risk Factors Pain itself is multidimensional with the complexity of physiological, sensory, behavioral, socioeconomic, and cognitive components. Postoperative Pain Preoperative anxiety Age less than 49 Severe post-op pain was associated with developing chronic pain. Age at diagnosis Younger patients hypothetically noted to be more sensitive to nerve damage, because they are more sensitive to nerve damage, are less likely to tolerate pain, and have increased anxiety. Younger women are commonly offered more aggressive treatments. Axillary radiation and neuropathic Pain Neuropathic pain is a side effect of radiation therapy, which can occur months to years after treatment. In a series published in the Journal of Pain published in 2008, postoperative radiotherapy and neurotoxic chemotherapy, along with axillary lymph node dissection, were thought to contribute to chronic pain in 70% of patients who were pain free after the operation. [7] Skin changes with radiation Procedure Type An axillary node dissection can contribute to nerve injury in PMPS. The Intercostobrachial nerves enters the axilla and pass through the posteromedial border of the upper arm. There is a higher incidence of chronic pain in patients undergoing axillary lymph node dissection compared to sentinel lymph node dissection.[7] Anatomy of the chest wall and axilla Axillar dissection Thoracodorsal bundle Procedure Type The surgical treatment approach did not associate with PMPS. This includes a total mastectomy versus a partial mastectomy. Complications such as the incidence of seroma, hematoma, cellulitis, lymphedema, and reoperation did not correlate with PMPS. [8] Description of procedures Description of procedures A partial mastectomy is usually reserved for women with stage I or II breast cancer. It is a breast conserving therapy which is followed by radiation therapy to the remaining tissue. A lumpectomy (wide local excision) removes just the tumor and a small cancer-free area of tissue surrounding the tumor. If cancer cells are found later, the surgeon may remove more of the tissue. This procedure is called re-excision. Description of procedures A radical mastectomy is the complete removal of the breast, including the nipple. The surgeon also removes the overlying skin, the muscles beneath the breast, and the lymph nodes. A less traumatic and more widely used procedure is the modified radical mastectomy (MRM). With the modified radical mastectomy, the entire breast is removed as well as the underarm lymph node. But pectoral muscles are left intact. Psychosocial factors Psychosocial factors PMPS is associated with psychosocial factors; including depression, insomnia, anxiety, somatization, and catastrophizing. Lack of physical activity is also associated with decreased psychosocial well-being. Clinical Examination PMPS patients commonly present with burning, numbness, stabbing pain, electric shock, hyperesthesia, and/or paraesthesia. Numbness is the #1 symptom reported in women status post surgery for treatment of breast cancer. Chest wall pain, decreased ROM of the shoulder, and decreased shoulder and grip strength. Clinical Examination Sensory changes at the post-op site. Decreased ROM of the ipsilateral upper extremity. Decreased shoulder strength. Diagnosis The diagnosis is made based upon a thorough physical examination of the remaining breast, chest wall, axilla, and upper extremity. A complete sensory and motor neurological examination may reveal abnormalities in the affected peripheral nerve distribution. Differential Diagnosis Recurrent breast cancer Metastatic breast cancer (humerous) Breast infection/inflammation Chemo-induced neuropathy Lymphedema Musculoskeletal disorders Cervical radiculopathy Treatment Treatment Much of what is practiced currently in chronic pain management comes from treating cancer pain. Choosing the appropriate therapeutic strategy is dependent upon making the correct diagnosis of the type of pain-neuropathic versus nociceptive. Common sense ain’t common. Algorithm Lifestyle: Home safety checks, cane, walker, increase in daily activity level. Medications: Antidepressants, calcium channel alpha 2-delta ligands, topical therapy, opioids, nutritional supplements. Therapy: PT program to address stretching, increase activity, increase ROM, desensitization program, etc… Interventions: Injection of the rotator cuff tendons, Botox of the Pec major, Serratus Anterior. Diagnostics: Imaging to rule out a recurrence, injury. Medications Anticonvulsants: Used since the 1960s for neuropathic pain, Gabapentin, Lyrica, and Carbamazepine are FDA approved to treat neuropathic pain. Gabapentin and Lyrica bind to the voltage-gated calcium channel at the alpha-2 delta subunits. Lyrica was designed as a lipophilic GABA analog to facilitate diffusion across the BBB. Side effects include dose-dependent sedation and dizziness. Medications Antidepressants: SNRIs such as Cymbalta have been shown to be effective in the treatment of neuropathy, fibromyalgia, chronic low back pain, and osteoarthritis. Side effects include dry mouth, fatigue, constipation, dizziness, insomnia, drowsiness, and nausea. Many patients are concerned about weight gain. Medications TCAs (Nortriptyline, Elavil, and Desipramine: None carries a specific FDA indication for pain management; however, they have frequently been used for chronic pain management with success. Side effects include dry mouth, sedation, constipation, orthostatic hypotension (Elavil has the most effect), and anticholinergic symptoms. Topical agents Avoid drug interactions, with minimal systemic absorption. Lidocaine 5% topical ointment, Capsaicin cream, and compounding creams are commonly used. Capsaicin is believed to block Substance P from primary afferent neurons. Studies have not proven high efficacy, but can be trialed in patients refractory to other types of treatment. Botox injections Rotator cuff injections Home exercise program Slowly increasing daily activity level, by staring with a 12 minute walk per day. Perform daily stretching of the affected shoulder, in hopes of regaining prior ROM, and for prevention of adhesive capsulitis. Stretch the muscles of the anterior chest wall. Managing side effects of treatment Prescribe a bowel program, as constipation is a common theme in chronic pain management, due to drug side effects. Encourage adequate fluid intake, ideally 64 fluid ounces per day, with some intake in the form of a Power Aide Zero or Gatorade, to replace electrolytes. May help reduce fatigue. Thank you References 1. 2. 3. 4. 5. 6. Couceiro TC, Valenca MM, et al. Prevalence of Post-Mastectomy Pain Syndrome and Associated Risk Factors: A Cross-Sectional Cohort Study. Pain Management Nursing, Vol 15, No 4 (December), 2014: pp 731-737. Fabro EA, Bergmann A, Amaral e Silva B, et al. Post-mastectomy pain syndrome: Incidence and risks. The Breast. 29 January 2012. Meijuan Y, Zhiyou P, Yuwen T, et al. A retrospective study of postmastectomy pain sydnrome: incidence, characteristics, risk factors, and influence on quality of life. Scientific World Journal 2013; 2013: 159732 Belfer I, Schrieber KL, et al. Persistent Postmastectomy Pain in Breast Cancer Survivors: Analysis of Clinical, Demographic, and Psychosocial Factors. American Pain Society. 3 May 2013. Ilfeld BM, Madison SJ, et al. Persistent Postmastectomy Pain and Pain-Related Physical and Emotional Functioning With and Without a Continuous Paravertebral Nerve Block : A Prospective 1-Year Folllow-Up Assessment of a Randomized, Triple-Masked, PlaceboControlled Study. Annals of Surgical Oncology. 21 November 2014. Mejdahl MK, Andersen KG, et al. Persistent pain and sensory disturbances after treatment for breast cancer: six year nationwide follow-up study. BMJ. 11 April 2013. References 7. Steegers MA, Wolters B, et al. Effect of axillary lymph node dissection on prevalence and intensity of chronic and phantom pain after breast cancer surgery. J Pain 2008; 9:813. 8. Schreiber KL, Martel MO, et al. Persistent pain in postmastectomy patients: comparison of psychophysical, medical, surgical, and psychosocial characteristics between patients with and without pain. Pain 2013; 154: 660. 9. Cronin-Fenton DP, Norgaard M, et al. Comorbidity and survival of Danish breast cancer patients from 1995 to 2005. Br J Cancer 2007; 96: 1462-8.