Encephalitis CBP - UBC Critical Care Medicine, Vancouver BC
advertisement

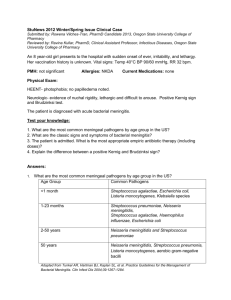
Encephalitis and Meningitis CBP Yoan Lamarche, 2009 46 yo male presenting to ED with progressive decreased LOC since 2 days. Able to mumble answers to questions. No history of recent travel or drug use. No allergies. On exam, patient protects A/W, Bp 110/52, HR 92, RR 29, Sat 92% RA T 38.4C. Neck N. Chest/Abdo N. Skin show no rash. WBC 14 000. CXR N. No focal signs on exam. ABG shows mild respiratory alkalosis. Approach to the unconscious Pt • • • • • • Naisan Scot Noemie Marios Neil Todd Initial workup, ↓LOC • • • • • • • • Glycemia ABCs Physical exam: seizure-localizing-toxidrome Labs: kidney, liver, sepsis, ABG, AG CT Head LP EEG Overlapping Tx 2. Describe the usual clinical presentation for meningitis, including the relative frequency of different signs and symptoms Clinical Presentation • Classical triad – Fever: 95% on presentation – Nuchal Rigidity: 88% on initial exam • Brudzinski sign • Kernig sign – Mental status change: 77% • Triad present in 44% pts on presentation • Sensitivity of 99% if pt has at least one finding of the triad N Engl J Med 1993 Jan 7;328(1):21-8 • How does the bug get to the brain? Organism Site of entry Predisposing conditions Neisseria meningitidis Nasopharynx Usually none, rarely complement deficiency Strep. Pneumoniae Nasopharynx or direct extension across skull fracture All conditions that predispose to pneumococcal bacteremia, fracture of cribriform plate Listeria monocytogenes GI tract, placenta Defects in cell mediated immunity Coagulase-negative staphylococcus Dermal or foreign body Surgery and foreign body, especially ventricular shunt Gram negative rods Various Advanced medical illness, neurosurgery Haemophilus influenzae Nasopharynx Diminished humoral immunity taphylococcus aureus Bacteremia, dermal, or foreign body Endocarditis, surgery and foreign body, especially ventricular shunt Major mechanism • Colonization of the nasopharynx with subsequent bloodstream invasion and subsequent central nervous system (CNS) invasion. • Invasion of the CNS following bacteremia due to a localized source, such as infective endocarditis or a urinary tract infection Major mechanism • Direct entry of organisms into the CNS from a contiguous infection (eg, sinuses, mastoid), trauma, neurosurgery, a cerebrospinal fluid (CSF) leak, or medical devices (eg, shunts or intracerebral pressure monitors or cochlear implants in children) 2. A)How does the bug get to the brain Emerg Clin N Am 2009 Clinical Presentation- Meningitis • 30% Seizure • 30% Focal Neuro signs 1. ↓ LOC 95% will have > 2 of 2. Fever 3. Neck Stiffness 4. Headache van de Beek D, de Gans J, Spanjaard L, et al. Clinical features and prognostic factors in adults with bacterial meningitis. N Engl J Med 2004;351(18):1849–59 Predictors: Bacterial 1. 2. 3. 4. Seizure ↓LOC Focal Shock 1 of those + •Neutro > 1000/mm3 Most likely Bacterial Brivet FG, Ducuing S, Jacobs F, et al. Accuracy of clinical presentation for differentiatingbacterial fromviralmeningitis in adults: amultivariate approach. IntensiveCareMed 2005;31(12):1654–60 • SiADH more frequent with Bacterial Meningitis • BC + in 50% Bacterial 30% other suppurative focus of Ix H influenza b Asplenia HIV Neisseria Meningitidis Young adults-children Deficiency in C5C6-C7-C8±C9 Pneumococcu s Adults Asplenia Myeloma Hypogammaglob R-OH Basilar skull Fx 50% infections Listeria Neonates ROH Elderly Cancer Immunosupp Cole slaw Milk Cheese Processed meat GNB Head trauma Neurosurgery Neonates S epi CSF shunts S aureus Post neurosurgery Db, R-OH, CRF, Cancer Group B Strep Db, R-OH, Parturient, cardiac disease, collagen, hepatic, renal, steroids 30% other suppurative focus of Ix E coli, Kleb, Pseudo Question 3: Describe the initial sequence of investigations and treatment plan in a patient with suspicion for meningitis Initial investigations in suspected bacterial meningitis Ensure adequate airway, breathing and circulation. Stat blood cultures + lumbar puncture Routine septic blood work (CBC, lytes, Creat, LFTs, lactate, coags) ABG Chest X-ray Contraindications to LP • Theoretical risk of brain herniation following lumbar puncture in pts with increased ICP. IDSA criteria for pre-LP CT head: Tunkel A, et al. Practice Guidelines for the Management of Bacterial Meningitis (IDSA Guidelines). CID 2004;39:1267-84 Other relative contraindications to LP • Thrombocytopenia (plts < 50 000) • Coagulopathy or systemic anticoagulation (INR > 1.4). • Epidural abscess or infection over LP site Initial management in suspected bacterial meningitis Tunkel A, et al. Practice Guidelines for the Management of Bacterial Meningitis (IDSA Guidelines). CID 2004;39:1267-84 Lancet ID 2007 LP: Complications: IDSA Guidelines 2004 An LP is done after a CT of the head showing 8000 WBC/μl 4. Describe the findings on LP, what if traumatic? LP: send for • Cell count, differential • Biochemistry (gluc-proteins) • Stains and cultures for bacteria, fungi and mycobacteria • Viral studies-HSV PCR (Sen 98%, Spe 94%,NPV suboptimal) Latex Agglutination • Sen 50-100% • Spe <100 • Does not change tx in Bacterial Meningitis (treat or not with ATBX) • May be useful if received ATBX and CSF clear Broad Range Real time PCR • Sensitivity of 86%-100% • Specificity of 98% when compared with culture -Deutch S, Pedersen LN, Podenphant L, et al. Broad-range real time PCR and DNA sequencing for the diagnosis of bacterial meningitis. Scand J Infect Dis 2006;38(1):27–35. -Saravolatz LD,Manzor O, VanderVelde N, et al. Broad-range bacterial polymerase chain reaction for early detection of bacterial meningitis. Clin Infect Dis 2003;36(1):40–5. Acute Phase reactants •Nathan BR, Scheld WM. The potential roles of C-reactive protein and procalcitonin concentrations in the serumand cerebrospinal fluid in the diagnosis of bacterialmeningitis. Curr Clin Top Infect Dis 2002;22:155–65. •Gendrel D, Raymond J, Assicot M, et al. Measurement of procalcitonin levels in children with bacterial or viral meningitis. Clin Infect Dis 1997;24(6):1240–2. •Viallon A, Zeni F, Lambert C, et al. High sensitivity and specificity of serum procalcitonin levels in adults with bacterial meningitis. Clin Infect Dis 1999;28(6):1313–6. •ViallonA,Guyomarc’h P,Guyomarc’h S, et al.Decrease in serumprocalcitonin levels over time during treatment of acute bacterial meningitis. Crit Care 2005;9(4):R344–50 Post Neurosurgery • Lactate > 4mmol/l: higher risk of meningitis • Sensitivity was 88% • Specificity was 98%. • The positive predictive value was 96% • Negative predictive value was 94% • RT-PCR may have high SEN, research Leib SL, Boscacci R, Gratzl O, et al. Predictive value of cerebrospinal fluid (CSF) lactate level versus CSF/blood glucose ratio for the diagnosis of bacterial meningitis following neurosurgery. Clin Infect Dis 1999;29(1):69–74. . Pfausler et al Lancet 2007 Neurol Clin 2008 Viral encephalitis Review Solomon 2007 • 5. What is the bacteriology of bacterial meningitis? (Scot) • Historical – – – – – – – H influenzae (45%) S pneumoniae (18%) Neisseria meningitidis (14%) Group B streptococcus (S agalactiae) (6%) Listeria monocytogenes (3%) Others (14%) Children < 5 years old >70% H influenzae • HIB vaccine introduced in 1990s. • Since HIB vaccination – – – – – – S pneumoniae (47%) N meningitidis (25%) group B streptococcus (12%) Listeria monocytogenes (8%) H influenzae (7%) Others (1%) • Remains to be seen whether proportions will change with the increasingly widespread use of S pneumoniae multivalent vaccines. • In infants where it has been used, invasive S pneumoniae disease has decreased by >90%. 6-What should you initiate as a treatment for your now intubated unconscious febrile patient with possible meningitis? Is there resistance to this treatment? Empiric Treatment for Bacterial Meningitis • ABCs, as above. • Critical care setting, given decreased LOC and sepsis requiring airway protection and ventilatory support. • Fluid resuscitation as required. • Immediate antibiotics. Empiric Treatment for Meningitis • 3rd-generation cephalosporin, i.e. ceftriaxone 2 g IV q 12 hrs (maximize CSF concentration with this dose). • Vancomycin 1.5 g IV X1, then 1 g IV q 12 hrs. – For pneicillin-resistent pneumococci • +/- ampicillin if risk factor for Listeria monocytogenes – Alcoholism, immunosuppression Resistance to Initial Antibiotics • Antimicrobial resistant organisms: – Strep pneumo: may be resistant to penicillin (hence empiric vancomycin); approx 10% across VCH. – Neisseria meningitidis: often resistant to penicillin (hence empiric 3rd-generation cephalosporin) – May add rifampin if resistant to ceftriaxone (MIC > 2mg/L) • Wrong organism – Viral – Fungal Van de Beek, NEJM 2006 Directed Pharmacotherapy of CNS Infections: What Intensivists SHOULD Know What are the in vitro susceptibility results (if culture positive)? Is the antibacterial bactericidal in the CNS? Subarachnoid space/brain tissue are regions of ineffective host defence Antibiotics must demonstrate bactericidal activity in vivo What is the antibacterial concentration attainable in CNS? Central Nervous System Compartments The Brain and CSF cannot be viewed as 1 pharmacokinetic (PK) compartment! Three distinct PK compartments within the CNS 1. CSF 2. Extracellular space of neuron tissue 3. Intracellular space (neurons, glial cells, granulocytes, lymphocytes, macrophages) Drugs penetrate into each of these compartments to varying degrees CSF is not homogeneous (drug concentration higher in lumbar versus ventricular CSF) Blood-Central Nervous System Interfaces Blood-Brain Barrier Located in endothelial cells of vessels of brain and spinal cord Linked by tight junctions Only 0.02% of brain capillaries possess fenestrated endothelium Blood-CSF Barrier Choroid plexus is characterized by fenestrated vascular endothelium Blood-Central Nervous System Interfaces Blood-CSF Barrier Blood-Brain Barrier Most Important Drug-Factors Associated with Antibacterial CNS Concentration Molecular Size (smaller molecules pass better) Lipophilicity (lipophilic molecules pass better) Drug-Plasma Protein Binding (low protein binding enhances CNS penetration) Less Important Drug-Factors Associated with Antibacterial CNS Concentration Active transport into CSF (low clinical significance) Low capacity, facilitated diffusion system at blood-brain barrier exists for some penicillins/cephalosporins Active efflux from CSF (pump located in 3rd/4th ventricles) Molecular charge (low clinical significance) Weak acids, such as penicillins/cephalosporins will be nonionised in acidic CSF (more readily pass from CSF back into blood compartment) Metabolism at the barriers This is why IV dopamine is not useful for PD Meningeal Inflammation and CNS Drug Concentrations: Why? • Alteration of barrier permeability – Antibiotic therapy inflammation and CNS penetration 's over course of treatment – Corticosteroid therapy inflammation and 's CNS penetration • Inhibitory effect on CSF drug-efflux pump • CSF production CSF bulk flow CSF drug clearance CNS drug concentration Neuro Clin 2008 Empiric antibiotics van de Beek D, et al. Community- acquired bacterial meningitis in adults. N Engl J Med 2006; 354: 44–53. Antibiotic doses Fitch MT, van de Beek D. Emergency diagnosis and treatment of adult meningitis. Lancet Infect Dis 2007; 7:191-200 Empiric regimens • Dexamethasone 10 mg IV q6h x 4 days (dose to be given with or before first antibiotic dose) • Ceftriaxone 2 g IV q12h (or Cefotaxime 2 g IV q6h) • Vancomycin 15 mg/kg IV q12h • Amoxicillin 2 g IV q4h Tx Meningitis Add Dexamethasone 10mg IV q 6 x 4d pre ATBx for all. STOP if not Pneumococcus Tx Meningitis • • • • • • Bacterial: 10-14d Meningococcus: 7d E coli and GNB: 21d S agalactiae: 14-21d L monocytogenes: 21d If Not Pneumococcus: D/C steroids (IDSA), If Resistant pneumococcus: Stop Steroids (decrease Vanco penetration in CNS) • If already on ATBX, do not initiate Steroids NEJM 2006, van de Beek review IDSA Guidelines 2004 • IDSA GUIDELINES 2004 IDSA 2004 7- Should this patient receive steroids? What is the evidence for steroids in bacterial meningitis? Neil Should this patient receive steroids? What is the evidence for steroids in bacterial meningitis? • • • • 18 studies 2750 pts Mortality RR 0.83 (0.71-0.99) Hearing loss RR 0.65 (0.41-0.91) Neuro sequelae RR 0.67 (0.45-1.00) After 3 days, the patient’s partner appears in the unit, claiming they both have HIV, are on triple therapy, but that they are not together for the past 3 months. 8-What is the differential diagnosis of decreased LOC in the HIV patient with a CNS infection? At what levels of CD4 will you find those infections? Describe the typical investigations and typical findings for each of those infections DDX of CNS infections in HIV CD4 count CSF TESTS TB Any, but usually <250 Inc. protein and WBC Dec glucose BUT can be N AFB Culture Toxoplasma Encephalitis < 200 Usually contraindicated CT Scan IgG/IgM Cryptococcal Meningitis < 100 ++opening pressure Inc protein and monos. N glucose Antigen (94.1% spec) Culture CMV Encephalitis < 50 Inc protein and monos PCR Antigen cytology Progressive Multifocal leukoencephalopathy < 250 Normal PCR of CST CT scan Primary CNS lymphoma < 100 Inc protein PCR of EBV CT Scan DDX of CNS infections in HIV • Not CD4 dependant – Abscess • Staph/strep/aspergillus/nocardia/listeria – Syphillis – Neurocysterocosis – All the regular other stuff (bacterial, viral) Three days after the initiation of antibiotics, the patient wakes up with progressive signs of R sided paralysis 9- What are the complications of bacterial meningitis? Noemie – When to initiate ICP monitoring – When to do EEG Neurological complications • Altered mental status – 3 % have severe disability at 8 wks • Increased ICP – headache, confusion, irritability, N/V • Seizures – Occur in 5% before admission and 15% after admission – More common with pneumococcal meningitis – associated with a higher risk of neurologic deficits at hospital discharge (24 versus 6 percent) Uptodate.com Major CNS complications N Engl J Med 2006;354:44-53 Mortality • Mortality from Strep Pneumonia:19-37% • Mortality from Meningococcus: 3-13% • Strongest RFs for an unfavorable outcome are: – – – – evidence of systemic compromise impaired consciousness low WBC in the CSF Infection with S. pneumonia Complications • • • • • • Shock (15%) Seizures (30%) SiADH Subdural empyema Epidural abcess Increased ICP EmClinNAm 2009 While you are treating your patient for this complication, the partner collapses, seizing. You intubated him and send him to emergency. After he stopped seizing, he remains unresponsive. Question 10: Describe the clinical presentation of typical viral encephalitis Classical presentation of viral encephalitis • An acute flu-like prodrome developing into an illness with high fever, severe headache, nausea, vomiting and altered consciousness • Often associated with seizures and focal neurological signs lethargy, drowsiness, confusion, disorientation. Solomon T, et al. Viral Encephalitis: a clinician’s guide. Pract Neurol 2007; 7: 285–302 MENINGITIS VERSUS ENCEPHALITIS • The presence or absence of normal brain function is the important distinguishing feature between encephalitis and meningitis. • In encephalitis, abnormalities in brain function are expected including: - Altered mental status Motor or sensory deficits Altered behavior and personality changes Speech or movement disorders. Hemiparesis Flaccid paralysis Paresthesias • Patients with meningitis may be uncomfortable, lethargic, or distracted by headache, but their cerebral function remains normal. • Seizures and postictal states can be seen with meningitis alone and should not be construed as definitive evidence of encephalitis. Johnson RP, Gluckman SJ. Viral encephalitis in adults. www.UpToDate.com Clinical presentation Type Clinical Picture 1-2weeks post immuniz- post viral Postinfectious Fulminant Eastern Equine Herpes Simplex Slowly progressive Creutzfeld Jacob/Variant Subacute sclerozing panencephalitis (SSPE) AIDS Chronic-fluctuating mycobacteria Fungal (Mucor may be rapid) Cause Clues Arbovirus Season, locale, degree of insect exposure Rocky Mountain spotted fever Tick Eastern Equine Local horses or pheasants, enzootic area West Nile Outbreaks in dead birds St-Louis Serologis changes in chickens Lyme Tick Rabies Racoons, Bats, Fox, dogs Ehrlichiosis Tick Leptospirosis Animals Herpes Simplex HSV Tests The patient partner is now 39.5C and shivers, a rash appears all over his body. He is still unconscious. He is not receiving antibiotics. You wonder if this could be a Meningococcal meningitis 11. Describe the post exposure prophylaxis in bacterial meningitis for the resident who intubated him. For you, as a supervisor. For the nurses. For his family. (Scot) Post-exposure prophylaxis • Incidence of transmission of Meningococcus among household contacts is about 5% (increased risk of developing meningitis by 500-800 times). • 1/3 of secondary cases develop in 2-5 days, so prompt appropriate prophylaxis necessary for high risk contacts. High-risk, non-healthcare: • Household (slept or ate in same household). • Intimate nonhousehold with mucosal contacts (sexual partner). • Direct exposure to secretions (shared utensils, toothbrushes, kissing, school/daycare) in previous seven days. High risk, healthcare: • direct mucosal contact with the patient’s secretions (mouth-to-mouth resuscitation, endotracheal intubation, or suctioning of the airway.) Prophylactic regimens: • rifampin 600 mg dose for adults, 10 mg/kg every dose for children older than 1 month, 5 mg/kg every dose for neonates (age less than or equal to 30 days) orally every 12 hours for a total of four doses. • alternative single dose regimens: ciprofloxacin 500 mg by mouth for adults or ceftriaxone 250 mg IM (age greater than or equal to 12 years) or 125 mg IM (age less than 12 years). Prophylaxis for other organisms: • H influenzae: Rifampin for nonpregnant household contacts if there are young children (age younger than 4 years) in the household. • Chemoprophylaxis is not given for pneumococcal meningitis. 12- Describe the long term outcomes of patients with bacterial meningitis Todd Long-Term Outcomes in Bacterial Meningitis • Death. – Mortality is approximately 25% in adults (NEJM 1993, of 493 episodes), up to 50% in geriatric population. – Driven by S. pneumoniae; around 5% for H influenzae or N meningitidis, or GBS. – Poor prognostic factors include: • Decreased LOC at admission, increased ICP, seizures within 24 hours of admission, need for mechanical ventilation, delayed treatment, age > 50 yrs, medical comorbidities. • Presence of osteitis or sunusitis, thrombocytopenia, tachycardia, low CSF cell count, elevated ESR, positive blood cuture and absence of rash. Long-Term Outcomes in Bacterial Meningitis. Up to 60% have one or more of: • Hearing loss (mainly in children) • Cognitive impairment • Personality changes • Gait disturbances, dizziness • Blindness • Seizures • Paralysis/paresis • • • • • • • Hydrocephalus Subdural abscess Subdural effusion Subdural empyema Epidural abscess Cerebral thrombosis Cerebral vasculitis De Beek, NEJM 2004 13- As you were ordering some cipro for the sister who just showed up in the unit, she tells you about an envelope containing white powder that her brother received a couple days ago. What is the clinical presentation of Anthrax? Treatment? Outcome? Todd Just say “NO” to white powder… • • • • Anthrax: Not just a thrash band from the 80s. One more reason to fear post offices. 3 clinical presentations: – Cutaneous – Inhalation – Gastrointestinal Cutaneous Anthrax • Usually through contact with infected animals or animal products. • Small, occasionall pruritic papules that quickly enlarge to develop central vesicles or bullae, followed by erosion to necrotic ulcer. • Regional lymphadenopathy and edema of surrounding tissue. • May develop systemic symptoms, including fever, malaise and microangiopathic hemolytic anemia/ coagulopathy and renal failure. Inhalation Anthrax • Incubation period usually 1 to 7 days (reported to be as long as 43 days). • Nonspecific symptoms at first, such as fever, malaise, mylagia. • Progresses to hypoxia and respiratory failure, with hypotension, cyanosis and stridor. • May progress to hematogenous spread, including hemorrhagic meningitis. • Untreated, it’s fatal. 45 % mortality with treatment in 2001 bioterror event in US. Gastrointestinal Anthrax • Oropharyngeal – Oropharyngeal edema, with necrotic pseudomembranous ulcers, pharyngitis and cervical lymphadenopathy. • Diarrheal – Intestinal and mesenteric edema, with associated lymphadenopathy. Necrotic ulcers may form. – Presents with N/V, abdominal pain, anorexia and possibly hematemesis or bloody diarrhea. May proceed to toxemia, shock and death. • Overall case fatality rate 25-60%. Diagnosis • History (cloud of white powder in the post office, or at work after a creepy guy got fired) • Clinical (as above) • Stool, sputum, pleural fluid and blood at 2-8 degrees C • Room temp swabs • Formalin-fixed tissue samples. • Frozen tissue samples – All for C&S and PCR (B. anthracis), with several immunochemical tests available (i.e. ELISA*, immunohistochemistry, Redline Altert S-layer protein*) – Most go to CDC/Lab response network. – * = commercially available Treatment • Bacillus anthracis is highly susceptible to many antibiotics, including: – Fluoroquinolones – Erythromycin – Tetracycline, Doxycycline – Chloraphenicol – Streptomycin – Vancomycin – Rifampin • NOT to cephalosporins or TMP/SMX • Treat for 60 days in event of bioterrorism-related exposure, due to risk of inhalational anthrax. Empiric Regimen • Adults and children; – Ciprofloxacin or Doxycycline IV plus clindamycin, vancomycin, rifampin or a carbapenem • Pregnant women – Same, with cipro preferred over doxy. Toxoplasma Gondii Encephalitis in HIV + Toxo encephalitis • • • • IDSA Guidelines HIV 2008 Rare if CD4+>200, more if < 50cells/ul Fever, confusion, motor weakness, headache Dx – CT: mass lesions – Syndrome – Tissue/Microbio Dx (if fails to respond to Tx, need Bx) Toxo encephalitis DDx: Lymphoma MycoB (Tb) Fungi (Crypto) PML (Progressive multifocal leukoencephalopathy) Chagas PML Toxo White matter Gray matter no mass effect enhancement no enhancement mass effect Toxo encephalitis, Tx 1. Pyrimethamine + sulfadiazine 2. Pyrimethamine + clinda + leucovorin 3. TMP+SMX (If IV, TMP-SMX IV vs PO Pyrimethamine + IV Clinda) Side effects Toxo drugs • • • • • Pyrimethamine – rash, nausea, – Bone marrow suppression (neutropenia, anemia, and thrombocytopenia) that can often be reversed by increasing the dose of leucovorin to 50–100 mg/day administered in divided doses (CIII). Sulfadiazine – rash, fever, leukopenia, hepatitis, nausea, vomiting, diarrhea, and crystalluria. Clindamycin – fever, rash, nausea, diarrhea (including pseudomembranous colitis or diarrhea related to Clostridium difficile toxin), and hepatotoxicity. TMP-SMX – rash, fever, leukopenia, thrombocytopenia, and hepatotoxicity. Drug interactions between anticonvulsants and antiretroviral agents Management of Treatment Failure Toxo A brain biopsy, if not previously performed, should be strongly considered for patients who fail to respond to initial therapy for TE (BII) as defined by clinical or radiologic deterioration during the first week despite adequate therapy or lack of clinical improvement within 2 weeks. For those who undergo brain biopsy and have confirmed histopathologic evidence of TE, a switch to an alternative regimen as previously described should be considered (BIII)