מצגת של PowerPoint
advertisement

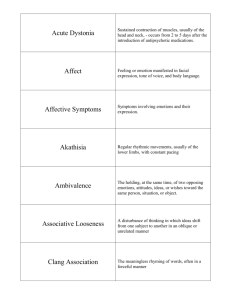
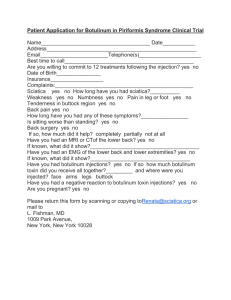
Botulinum toxin use in post traumatic cervical dystonia and head tremor Dr Marieta Anca-Herschkovitsch Movement Disorder Clinic Edith Wolfson Medical Center Israel Post-traumatic cervical dystonia :a subject of debate The development of abnormal posturing of the neck or shoulder after local injury has been termed posttraumatic cervical dystonia (PTCD). FIRST DESCRIPTION IN 1888 BY GOWERS Features to distinguish this disorder as a distinct clinical entity from those of typical idiopathic cervical dystonia are : onset and maximum disability occur very quickly after injury(hours to days), severe pain and a fixed abnormal posture(Lang ,2003),not influenced by sleep,poor response to BTX (Frei et al ,2004 ) In order to establish a consistent causal relationship between peripheral trauma and movement disorder, Jankovic (1994) proposed the following criteria : 1. The injury should be severe enough to cause local symptoms persisting or requiring medical attention for at least two weeks after the trauma; 2. The onset of involuntary movements must have occurred within one year after the trauma; 3. The abnormal movements should be anatomically related to the site of the injury. Moreover, the causal relationship should be supported by the absence of other causes capable of producing the same symptoms, presence of reflex sympathetic dystrophy and poor response to conventional treatment. The mechanism by which dystonia may be related to posttraumatic movement disorders and CRPS is poorly understood. *-mediated through the sympathetic nervous system- view recently called into question (Schott, 1995 ; Baron et al., 1999 ) * -Inflammation might be involved in the development of CRPS following injury, at least in the early stages (Birklein et al., 2001 ). * -Peripheral mechanisms ( sensitization of peripheral nociceptors, or ectopic or ephaptic transmission of nerve impulses) are suggested as a possible mechanism of CRPS and post-traumatic movement disorders (Jankovic, 1994 ; Schott, 1986b , 2001 ). However, spread to ipsilateral, axial, and contralateral muscles may occur in fixed dystonia, as in CRPS and post-traumatic dystonia, in these cases, such peripheral mechanisms are unlikely to explain the development of abnormal movements after injury. *-Impairment of interneuronal circuits at the spinal/ brainstem level and central synaptic reorganization analogous to that following amputation could be a possible mechanisms leading to such sequelae even after a minor peripheral injury (van Hilten et al., 2001 ). Controversy: 1-abnormal movements in CRPS indicate a somatoform or malingering origin? 2-evidence for organic origin : *- abnormalities of reciprocal inhibition of H-reflexes, seen in typical dystonia (Koelman et al., 1999 ; van de Beek et al., 2002a ,b ), *-abnormal stretch reflexes (van Hilten et al., 2001 ; van de Beek et al., 2002b) *- high prevalence of HLA-DR 13 in dystonia associated with CRPS (van Hilten et al., 2000b ) *-changes in contra lateral thalamic perfusion on 123iodine-labeled single photon emission computed tomography (SPECT) imaging in cases of CRPS (Fukumoto et al., 1999 ) . However, whether these central or peripheral changes are primary or secondary to the clinical abnormalities remains a matter of dispute, and the finding of a HLA-DR 13 association has yet to be replicated in other studies. Literature *- A series of 9 patients with PTCD in whom involuntary muscle spasms and abnormal head postures occurred within 7 days after cervical injury were treated with botulinum toxin as necessary, and were followed up to 5 years. Based on our observations of these cases, we propose that complex regional pain syndrome (CRPS) could represent a variant of posttraumatic cervical dystonia that may develop over time after the initiation of dystonia. (Frei et al,2004) *-A retrospective study of the clinical characteristics of the 16 patients with early post-traumatic CD (CD-PT) in comparison with the 52 patients reporting no antecedent trauma (CD-NT) was performed( O’Riordan,2004 ). In this comparison the CD-PT group had a significantly increased frequency of laterocollis, significantly more reported pain and more reported depression. Non-significant trends were noted for less responsiveness to botulinum toxin and less use of gestes antagonistes in the CD-PT group WHIPLASH ASSOCIATED DISORDER • The term "whiplash" has been used to describe a mechanism of injury, and the clinical manifestations as a consequence of the injury. • In 1995, the Quebec Task Force on Whiplash Associated Disorders (WAD) defined: "whiplash is an acceleration-deceleration mechanism of energy transfer to the neck. It may result from rear-end or side-impact motor vehicle collisions, but can also occur during diving or other mishaps. The impact may result in bony or soft-tissue injuries (whiplash-injury), which in turn may lead to a variety of clinical manifestations called Whiplash Associated Disorders • The incidence of whiplash injury :between 70–200 per 100,000 inhabitants no consensus about the natural course of the whiplash injuries . • It was concluded that 14 - 42 %of patients could develop chronic complaints (over six month duration), and that 10 percent of those patients had constant severe pain. • The common symptoms are: neck pain (88–100%), headache (54–66% ),neck stiffness, shoulder pain, arm pain/numbness, paraesthesia, weakness, dysphagia, visual and auditory symptoms and dizziness Mechanics of Whiplash Hyperextension HyperFlexion Majority of cases, no injury can be identified Symptoms attributed to musculo-ligamental sprain The exact pathophysiology of WAD is uncertain but probably involves some degree of aberrant muscle spasms and may produce a wide range of symptoms • Initial treatment of pain associated with whiplash usually includes oral medications, such as muscle relaxants and nonsteroidal anti-inflammatory drugs, agents limited by potential systemic adverse effects. Some patients with chronic WAD may benefit from radiofrequency neurotomy. • A new approach to treatment is the use of botulinum toxin, which acts to reduce muscle spasms. • Type A toxin (Botox) studied in small trials of patients with WAD has generally been found to relieve pain and improve range of motion(ROM). • Preliminary data from a small trial showed that type B toxin (Myobloc) produced almost immediate pain relief for most patients with postwhiplash headache., LITERATURE It was reported a significant reduction in pain and improvement in ROM in 77.4% of patients responding significantly to a BTX-A injection in an open label study with 31 patients, grade II WAD( Francisco Juan, 2003 ). Patients received 50–75 units of BTX-A, and the follow-up assessment was at week 8. BTX-A, specifically Botox®, has been studied for the treatment of WAD and chronic neck pain. BTX type-B has been studied in patients with postwhiplash headaches( Opida CL, 2002). The injection technique used for the neck is based on experience with cervical dystonia. The sites chosen are chiefly in the large superficial muscles, specifically, the splenius capitis, rectus capitis, semispinalis capitis, and trapezius (can develop hypertrophy). The muscles can easily be palpated in most individuals and can be injected without sophisticated techniques and without EMG . Personal experience Posttraumatic painful cervical dystonia SUBJECTS( 12 PATIENTS ) : 4 male and 8 female,age range 25-68y, 1 subject post cervical laminectomy , 1 post head trauma, 10 post whiplash injury ONSET of neck dystonia : few weeks to 6 months post trauma , on chronic cervicalgia and lack of other treatment strategies efficacy RESPONSE to Botox treatment –variable : --mild whiplash early treated resolved in 6 mo (2 inj) in 2 patients, --subjective/objective improvement (pain,ROM )in treatment period 2y-8y (each3-4 months), reduction of muscle tenderness and volume,head posture --Dynamic dystonia on treatment: 1 patient’s laterocollis shifted to anterocollis SIDE EFFECTS: transient dysphagia in 1 patient DOSES of Botulinum toxin/inj : 150-300 ui BTX /400-1000 ui Dysport SITES FOR INJECTION : trapezius,splenius capitis,sternomastoids ,paraspinal muscles HEAD TREMOR *In a clinical series of 487 individuals diagnosed with ET with a mean age of onset of 52, half of the sample had a family history of ET, half presented with symmetrical disease and tremor affected the arms (97%), voice (62%), head or neck (48%). ( Uitti RJ, 2007 ) * 43 patients with head tremor as the major complaint were treated with local botulinum toxin type A (Btx A) injections into neck muscles: 29 were classified as tremulous cervical dystonia (TCD), and 14 as head tremor without dystonia (HT). Patients with HT received mean total doses of 400 units (U) of Dysport (Btx A) (range, 160-560 U) distributed between the two splenius capitis muscles. Patients with TCD received a mean total dose of 500 U Dysport (range, 320-720 U) injected into a mean of 3 muscles (range, 2-4 muscles). The condition of all patients improved subjectively. The total on the Tsui scale as well as pain scores decreased significantly (p < 0.05) following treatment. Latency of onset, duration of improvement, and side effects showed no significant difference in HT and TCD. Amplitude of HT decreased significantly for both groups following treatment. The mean dominant peak frequency in TCD and HT was slightly less than 5 Hz and did not change significantly after treatment.(Poewe et al, 1997) Personal experience SUBJECTS(6 patients): 4 female, 2male, age 23-62 y, 2 with TCD as rotatory torticollis , 4 with HT changing direction /axis between anteroposterior (yes-yes) to lateral (no-no)movements Family history –negative Associated movement disorders- 2 patients(TS) Treatment duration :1y-5y Doses of botulinum toxin : 100-300 ui Botox/300-900ui Dysport Sites for injection: splenius capitis, sternomastoid muscles, bilateral Efficacy: improvement subjective / objective(amplitude,frequency) Side effects: negative Conclusion Botulinum toxin is a safe and effective therapy for most patients with cervical dystonia, including posttraumatic syndromes Botulinum toxin can safely be used to control tremor in patients in whom other forms of therapy have failed. “Regarding every disease now incurable we may entertain the hope that our powerlessness may not be permanent, and that we, or those who come after us , may be able to speak in very different terms “ W.R.Gowers , 1879