Legal Updates - New Jersey Psychological Association
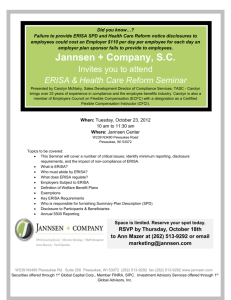
advertisement

NJPA Legal Update In Re Horizon UCR Litigation On July 9, 2014, Judge Chesler granted final approval of the settlement between the subscribers, providers, and NJPA and Horizon Blue Cross Blue Shield of New Jersey (“Horizon”). The settlement provides that Horizon will cease using the Ingenix Database and its homegrown Top of Range (“TOR”) database to determine reimbursement for out-of-network services. The settlement also provides that Horizon will revise is plan language, handbooks, website and other applicable marketing materials to clarify how reimbursement for out-ofnetwork services is calculated. A group of objectors appealed the district court’s order granting final approval of the settlement claiming that the settlement did not provide any meaningful relief since Horizon had already decided to cease using the Ingenix and TOR databases prior to entering into the settlement with Plaintiffs. The appeal has been fully briefed and has been calendared for submission on September 17, 2015. The Court of Appeals has not yet determined whether it will hear argument on the appeal. In Re Aetna UCR Litigation Following Aetna’s election to terminate the proposed settlement due to the number of requests for exclusions, the parties resumed active litigation of the action before Judge Katharine Hayden. In July 2014, Plaintiffs’ filed a motion for leave to file their third amended consolidated complaint. Similar to the prior complaints, the third amended complaint alleged ERISA and RICO violations on behalf of the Provider class and Provider Associations and alleged ERISA, RICO, antitrust, and certain state law violations on behalf of the subscriber class. In response, Defendants opposed the motion to leave and filed cross-motions to dismiss Plaintiffs’ second and third amended complaints. On June 30, 2015, Judge Hayden issued an order granting Plaintiffs’ motion for leave to file their third amended consolidated complaint and granting in part and denying in Defendants’ motions to dismiss. Unfortunately, the Court’s ruling was unfavorable for the Provider class and Associations. The Court found that the named Provider Plaintiff lacked standing to bring claims under ERISA because the assignment of benefit was in favor of limited liability company of which he was an owner and not the provider himself. Accordingly, the Court found that the provider had no ownership in the right to payment and no standing under ERISA. The Court did not rule on the issue of whether an assignment of the right to payment alone is sufficient to confer standing under ERISA. With respect to the Provider’s ERISA claims, the Court further ruled that the claims for failure to provide an accurate explanation of coverage and summary plan description, breach of fiduciary duties, and failure to conduct a full and fair review of denied claims were dismissed on the merits. The Court rejected the Plaintiffs’ contention that the disclosure requirements under ERISA relating to the evidence of coverage and summary plan description obligate the insurer to disclosure its methodology for calculating UCR payments. The Court also found that the duty to conduct a full and fair review of denied claims under ERISA does not include the requirement that insurers to explain their UCR claim reimbursement methodology. In addressing Plaintiffs’ claims for breach of fiduciary duty, the Court held that this claim was duplicative of the claim for benefits under ERISA and must be dismissed. The Court also dismissed the Association Plaintiffs’ ERISA claims, which were brought in a representative capacity. Because the Court found that the Provider Plaintiff lacked standing, the Association Plaintiffs could not show that their members would otherwise have standing to sue in their own right. In addition, because the Provider Plaintiffs’ right to sue under ERISA are based on valid assignments of benefits, the Court concluded that the Association Plaintiffs also lacked standing because the alleged claims would require participation of the Associations’ members in order to demonstrate each member had obtained a valid assignment of benefit. The Court dismissed the Provider and Association Plaintiffs’ RICO claims on the merits finding that the allegations surrounding the Defendants submission of flawed data to Ingenix did not sufficiently demonstrate that Defendants knowingly conducted and participated in the affairs of the alleged RICO. The Court further held that Plaintiffs failed to demonstrate that the alleged fraudulent scheme proximately caused their injuries. According to the Court, the fact that the Defendants used methods other than the Ingenix Database to reimburse out-of-network claims and that Plaintiffs failed to adequately allege that out-of-network providers balance billed patients for their services in all cases prevented a finding of proximate cause to support their RICO claims. In sum, the Court left open the possibility that the Provider Plaintiffs may be able to join another Provider who possesses a valid assignment of benefits. If this occurs, the only remaining claim under ERISA is a claim for benefits. Even if the Court were to find that a new Provider Plaintiff possessed standing to bring a claim for ERISA benefits, it is unlikely that this would resurrect the Association Plaintiffs’ ERISA claim brought in their representative capacity based on the Court’s finding that any claim by the Associations under ERISA would require proof by each member of the Associations that they possessed a valid assignment of benefits. Franco v. Cigna The case is on appeal to the United States Third Circuit Court of Appeals. The parties have fully briefed the appeal. On May 14, 2015, the Court informed the parties that the case would be submitted to the Court on the parties’ briefs on June 4, 2015, and that no oral argument would be heard. It is likely that an opinion will be issued within the next 90 days.


![[Click and Enter Attorney Name], State Bar No - E](http://s3.studylib.net/store/data/007177564_1-4d9407aff5e1ecb2a5922cd955484ee2-300x300.png)