Case
advertisement

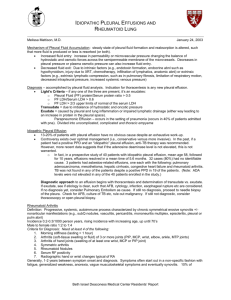
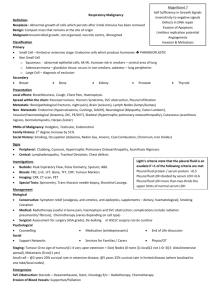
Pleural Effusion Larissa Bornikova, MD July 17, 2006 Objectives • To review the etiology and basic pathophysiology concepts related to pleural effusion. • To understand indications for thoracentesis. • To outline a systematic approach to diagnosing a cause of effusion. • To be able to differentiate exudative from transudative effusions. • To understand the basic principles of initial management of pleural effusions. Pleural Fluid: Normal Characteristics • Ultrafiltrate of plasma. • Enters pleural space primarily from the capillaries in the parietal pleura and removed via the lymphatics in the parietal pleura. • Produced at the rate of 0.01 cc/kg/hr. Normal volume of pleural fluid is about 16 cc for a 70-kg person. The rate of reabsorption is 20 times the rate of production. • Forms a thin layer (20 μ) in the pleural space. • • • • • pH 7.6 – 7.64 Protein content less than 2% (1-2 g/dL) Fewer than 1000 WBC per μL LDH less than 50% of plasma Glucose content similar to plasma Pleural Effusion It’s not a diagnosis! • Increased capillary hydrostatic pressure (CHF, superior vena cava syndrome) • Reduced intravascular oncotic pressure (hypoalbuminemia, liver cirrhosis) • Increased oncotic pressure in pleural space • Increased capillary permeability or vascular disruption (neoplastic disease, infection or inflammation, pancreatitis) • Decreased lymphatic drainage (obstruction or damage) • Reduction of pressure in pleural space (trapped lung) • Increased flow of fluid from the peritoneal cavity (liver cirrhosis) • Increased flow of fluid across the visceral pleura (pulmonary edema) • Disruption of intrathoracic vessels and thoracic duct • Iatrogenic Clinical Symptoms and Signs Symptoms Signs • Dyspnea is the most common symptoms at presentation and usually indicates large (>500 mL) effusion • Chest pain • Other symptoms occurring with pleural effusions are associated more closely with the underlying disease process. • Dullness or decreased resonance to percussion • Diminished or inaudible breath sounds • Decreased tactile fremitus • Egophony • Pleural friction rub • Asymmetric expansion of thoracic cage • Mediastinal shift • Other findings that provide clues to the cause of pleural effusion Indications for Thoracentesis 1. Pleural effusion >10 mm thick on lateral decubitus radiography of unclear cause. 2. If the patient presents with CHF and bilateral pleural effusions are of the same size, the patient is afebrile, and has no chest pain, a trial of diuresis can be undertaken. ** If effusion persists >3 days despite diuresis, or if the patient has fever, pleurisy, unilateral or markedly asymmetric pleural effusions in the absence of cardiomegaly, or if other atypical features are present (disproportionately widened A-a gradient) thoracentesis is indicated. 3. Therapeutic thoracentesis No absolute contraindications. Relative contraindications: anticoagulation or bleeding diathesis, very small pleural effusion, mechanical ventilation with high PEEP, active skin infection at the point of needle insertion, single lung, hepatosplenomegaly. Evaluation if pleural fluid Tests Indicated, According to the Appearance of the Pleural Fluid Light R. N Engl J Med 2002;346:1971-1977 Evaluation if pleural fluid: Light’s criteria. Pleural effusions that meet one or more of the three Light’s criteria are classified as exudates: • Ratio of pleural-fluid protein level to serum protein level > 0.5 • Ratio of pleural-fluid LDH level to serum LDH level > 0.6 • Pleural fluid LDH level > 2/3 the upper limit of normal for serum LDH level. Light’s criteria misclassify about 25 % of transudates as exudates. If criteria classify an effusion as exudative, but clinically suspect a transudative effusion, then serum albumin to pleural-fluid albumin difference should be measured. (Chest 2002; 122; 1524) Serum albumin – pleural-fluid albumin > 1.2 g/dL indicates transudative effusion. Sensitivity of Tests to Distinguish Exudative from Transudative Effusions Light R. N Engl J Med 2002;346:1971-1977 Leading Causes of Pleural Effusion in the United States, According to Analysis of Patients Subjected to Thoracentesis Light R. N Engl J Med 2002;346:1971-1977 Exudative pleural effusion require further laboratory investigation. • Cell count and differential - Neutrophil predominance indicates an acute inflammatory process - Lymphocytes indicate a chronic effusion (if >50% rheumatoid pleurisy, chronic fungal infections, chronic TB, sarcoidosis, chylothorax) - Eosinophils (pneumothorax, hemothorax, infarct, parasites, meds) - Mesothelial cells (>5% excludes tuberculous pleurisy) • Total protein level (>7 g/dL multiple myeloma and Waldenstrom’s should be considered) • Glucose level • LDH level (>1000 empyema, rheumatoid pleurisy, malignancy) • Amylase level • pH (low pH in empyema, malignancy, rheumatoid pleurisy, TB) • Cytologic analysis • Consider sending pleural fluid for Gram stain and culture, AFB stain, fungal cultures Parapneumonic effusions • Start out as sterile reactive effusions precipitated by pulmonary infections. • Progress from uncomplicated (free flowing, high WBC) to complicated (pleural pH <7.2, LDH >1000, glucose <60 mg/dL, loculations) to empyema (organisms on Gram stain/culture or frank pus on thoracentesis). • Pneumonia + pleural effusion = rapid diagnostic thoracentesis! Pleural effusion: Management • Transudative effusion treat underlying disease process. • Exudative pleural effusion management depends on etiology. • Symptomatic pleural effusion therapeutic thoracentesis. • Uncomplicated parapneumonic effusions generally resolve with antibiotics alone. - Aminoglycosides are inactivated at low pleural pH. • Complicated parapneumonic effusions or empyema require drainage in addition to antibiotic therapy. - Tube thoracostomy - Fibrinolytics - Thoracoscopy - Open thoracostomy - Decortication • Malignant pleural effusion: serial thoracentesis; tube thoracostomy; and/or pleurodesis. Algorithm for the Evaluation of Patients with Pleural Effusion Light R. N Engl J Med 2002;346:1971-1977 Case CC: fever, cough and shortness of breath HPI: 34-year-old man, an active IV heroin user, presents to the Emergency Department. He was in his usual state of health until about two weeks ago when he was evaluated in the emergency room for complaints of fever, chills, pleuritic chest pain, fatigue, and a cough productive of green sputum. A chest radiograph was taken during that visit and showed a right lower lobe infiltrate, but the patient left the emergency department without the discharge paperwork or prescriptions. Multiple attempts to contact him have been unsuccessful. In the two weeks since that visit, his symptoms have worsened. PMH: HIV test was negative 6 months ago per patient; no surgeries. Medications: Acetaminophen for fevers Allergies: NKDA Social History: IV heroin use; smokes half a pack of cigarettes per day for 15 years; social alcohol use; sexually active with women. Family History: non-contributory Case (cont’d) Physical Exam: VS: T 102.1; HR 110; BP 110/60; RR 20; O2 sat 92% on room air General: thin diaphoretic man, breathing uncomfortably, splinting. HEENT: no thrush; OP without lesions; normal TMs. Neck: supple, no LAD, JVP normal Lungs: egophony and dullness to percussion at the right base CV: tachycardic; regular; normal S1S2; no murmurs, rubs, or gallop. Extr: track marks on both forearms; no embolic stigmata; no c/c/e What do you think is going on? What would you like to do next? Case (cont’d) CXR: RLL and RML infiltrate and large right sided pleural effusion. Labs are drawn and pending. Case (cont’d) LABS: Blood: WBC 19; Platelets 390; Cr 0.6; INR 1.1; LDH 90 Thoracentesis: yellow-colored slightly hazy fluid, pH 7.0, LDH 70, WBC 80,000 with a predominance of PMNs, 1,200 RBCs, and grampositive cocci in chains. Post-thoracentesis CXR shows no pneumothorax. What is the next most appropriate management step for this patient’s condition? References • Light RW. Clinical practice: Pleural effusion. N Engl J Med 2002; 346; 1971. • Harrison’s Principles of Internal Medicine, 16th edition • UpToDate • Feller-Kopman. A Practical Approach to the Patient with a Pleural Effusion. CareWeb Portal slide presentation.