Weaving a Tapestry of Support: A View of Psychosocial
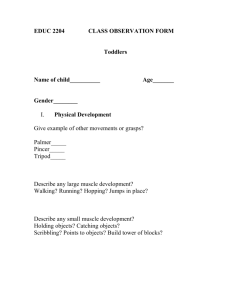
advertisement

Tracey Sutton, MSW, LCSW Family Support Services Of North Idaho A tapestry captures a moment in time. Using complex and rich designs and images, the artist tells a story of people, events, culture, beliefs and spiritual understanding. A tapestry is a metaphor for who we are as people. The threads of the past and present are woven together. The threads of decisions are how the present is connected to the past and future. “Mental health problems among children and adolescents constitute a public health crisis for our nation.” (Subcommittee on Children and Family, President’s New Freedom Commission, p. 1) Identify the unique qualities and challenges of psychosocial rehabilitation for children. Develop practical ways to integrate attachment theory and a strengths-focused approach to support caregivers in providing an emotionally responsive environment that will enhance the child's self-esteem and confidence on their trajectory toward greater resiliency. Discuss ethnic and cultural considerations, including history of oppression and trauma, when developing a family-centered treatment plan. Identify the skills necessary for youth to thrive in their living, learning and social environments, as well as the community resources available to help in the acquisition of those skills. “promote quality of life, community integration, and successful transition to adulthood for children and youth who have experienced serious emotional or behavioral difficulties that significantly impair the ability to function successfully in home, school, family or community life.” “services focus on empowering young people and their families to develop the skills and access the resources needed to increase their capability to thrive in the living, working, learning and social environments of their choice.” “undertaken in the spirit of partnership and collaboration between youth, caregivers, and providers. The services are individualized, driven by each young person and his or her family, and build on existing strengths. They promote each young person’s positive development, while supporting his/her movement along a developmental trajectory that will result in a successful transition to adulthood.” Successful transition to adulthood Increase capability to thrive Promote positive development Does the child/youth believe that something can be done to help them with their behaviors and improve their daily functioning? Does the family believe that something can be done to help the child/youth with their behaviors and improve their daily functioning? How is CPSR different than what has already been tried? Explanations about the problem behaviors and views about its etiology profoundly affect ideas about treatment. Often, different family members hold divergent beliefs about what should be done. Conflicts over the “appropriate” treatment may constrain effectiveness and polarize participants. Madson, 2007 To qualify for CPSR children must: • Be under 17-yrs old • Have serious emotional disturbance • Functional impairment as measured by the Child and Adolescent Functional Assessment Scale (CAFAS) or Preschool and Early Childhood Functional Assessment Scale (PECFAS) SAMSA definition of Severe Emotional Disturbance: “A diagnosable mental disorder found in persons from birth to 18-yrs of age that is so severe and long lasting that it seriously interferes with functioning in family, school, community or other major life activities.” The idea of recovery needs to be expanded to include resiliency when we speak of PSR for children. Systems of care must focus on facilitating recovery, and on building resilience, not just managing symptoms. Individual: intellectual functioning, easygoing temperament, self-efficacy, self-confidence, talents, close relationships to caring parent figures. Parenting: authoritative, warmth, structure, high expectations, socioeconomic advantages and connection to extended family networks. Community: bonds to pro-social adults, connections to pro-social organizations and attending effective schools. Masten & Coatsworth (1998) Social Learning Theory People learn from one another, via observation, imitation, and modeling. Experiential theory Concrete experience (or “DO”) Reflective observation (or “OBSERVE”) Abstract conceptualization (or “THINK”) Active experimentation (or “PLAN”) Behavior change and improved functioning occur as children learn and implement new ways of coping, behaving and thinking and as the child’s environment shifts to support desired behaviors. The child and family strengths, deficits and treatment needs should be clearly identified in the areas of psychiatric, medical, educational, social support/behavior toward others, family, basic living skills, housing, finances, cultural considerations and community. Successful transition to adulthood Increase capability to thrive Promote positive development What do these overall goals mean within the cultural context of the family? The individualized treatment plan will include specific goals and objectives with clearly stated tasks and outcomes to acknowledge success. Interventions are home and community based, child/family centered, culturally sensitive, individualized, integrated across providers and functional areas, and use evidence based practices. Specific services could include skill building, coordination of collateral agencies (school, day-care, probation, etc). The focus of intervention efforts are five-fold: Establish a working relationship with the child and his or her care givers. Increase motivation and hope for the child and family. Teach the child and caregivers a broad range of cognitive and behavioral skills designed to remediate symptoms and improve functioning. Allow the child and family to rehearse new behaviors or skills repeatedly in natural environments to the point of mastery. Alter environments so that desirable behaviors are reinforced and undesirable behaviors are ignored or consequence. Nathan J. Williams – CenterPoint Behavioral & Mental Healthcare, Inc. Nampa, Idaho (2009) Interventions take place in the home or natural community settings and are likely to include: Teaching children to be better observers of their own emotional states, level of emotional arousal and common triggers that generate unpleasant feelings. Provide effective education that develops an understanding of the link between thoughts, feelings and behaviors. Provide psychoeducation on social learning principles or on the child’s diagnosis. Teach specific cognitive and behavioral coping skills such as thought stopping, relaxation, self-talk, problem solving, social skills, perspective-taking, positive activity scheduling. Practice skills with coaching and feedback. Design reinforcement systems. Directly reinforce positive behaviors and consistently consequence inappropriate behaviors. Williams – (2009) Tools for presenting material: Didactic instruction, therapeutic games Role plays, puppets Modeling, coaching Workbooks, therapeutic stories Hope & Respect – all children have the capacity for learning and growth. Culturally Relevant – culture is central to recovery. Shared Decision-Making – facilitate partnerships with all people and community systems/agencies involved in supporting children, youth & families Strengths Based – build on the strengths & capabilities of each young person to promote resilience & recovery Family Centered – practices are designed to address the unique needs of each individual served, consistent with the values, hopes & aspirations of the individual and his/her family system. Community Integration – engage children in age- and developmental appropriate activities that promote positive growth. Empowerment – promote selfdetermination & empowerment, & honor family voice and choice. Natural Supports – identify and link children, youth and families to community resources. Quality of Life – improve all aspects of the lives of young people and their families including social, educational, financial, intellectual, physical and spiritual domains. Health & Wellness – promote a holistic view of wellness & encourage life-long habits for improving & maintaining physical & mental health. Evidence Based – best practices that produce outcomes congruent with empowerment, resilience & personal recovery. Accessible & Coordinated – services must be readily accessible to children & adolescents whenever, wherever and for as long as they are needed into adulthood. Services must be well coordinated with other treatments and practices. CPSR providers typically feel well prepared to work with children and youth, however there is also a need to understand the experience of caregivers. Considerable strain related to coping with the needs of their child/youth and coordinating services. Family members experience depression, fatigue and frustration with services systems that are uncoordinated. Safety is the core issue for children with disordered attachment and other attachment related problems. They are distant and distrustful because they feel unsafe in the world. They keep their guard up to protect themselves, but it also prevents them from accepting love and support. Set limits and boundaries. Consistent boundaries make the world seem more predictable and less scary. Take charge, yet remain calm when the child is upset or misbehaving. Remember that “bad” behavior means that the child doesn’t know how to handle what he or she is feeling and needs your help. Be immediately available to reconnect following a conflict. Conflict can be especially disturbing for children with insecure attachment or attachment disorders. After a conflict or tantrum where you’ve had to discipline the child, be ready to reconnect as soon as he or she is ready. Own up to mistakes and initiate repair. When you let frustration or anger get the best of you or you do something you realize is insensitive, quickly address the mistake. Try to maintain predictable routines and schedules. A child with an attachment disorder won’t instinctively rely on loved ones, and may feel threatened by transition and inconsistency. Respond to the child’s emotional age. Children with attachment disorders often act like younger children, both socially and emotionally. You may need to treat them as though they were much younger, using more non-verbal methods of soothing and comforting. Shock/Denial/Disbelief Emerging awareness of a difference in their child and a lack of clarity about what is happening. Recognition Initial awareness of a mental illness. Questions such as “what did I do wrong?” Coping Adjustment to the frequent crises & disruption in normal family life. Advocacy The family becomes more proactive in the community. Increased assertiveness, less self-blame, less blame of professionals. Time is spent to developing new roles and relationships with professionals. Friesen, B. J. (2007). Recovery and Resilience in Children’s Mental Health: Views from the Field. Psychiatric Rehabilitation Journal ,31(1), 38-48. Hopkins, G.L., McBride, D, Marshak, H.H., Preier, K., Stevens, J.V., Kannenberg, W ., et al. (2007). Medical Journal of Australia, 186(10). 71-73. Lefley, H.P. (2009). Family Psychoeducation for Serious Mental Illness. New York: Oxford University Press. Madson, W.C. (2007). Collaborative Therapy With Multi-Stressed Families (2nd ed.). New York: The Guilford Press. Masden, A., & Coatsworth, J.D. (1998). The development of competence in favorable and unfavorable environments: Lessons from research on successful children. American Psychologist, 53(2), 205-220. Williams, N.J. (2009). Preliminary Evaluation of Children’s Psychosocial Rehabilitation for Youth With Serious Emotional Disturbance. Research on Social Work Practice, 19(1), 5-18. Williams, N.J. (2009). Dose-Effect of Children’s Psychosocial Rehabilitation on the Daily Functioning of Youth with Serious Emotional Disturbance. Child Youth Care Forum, 38, 273-286.