systolic pressure
advertisement

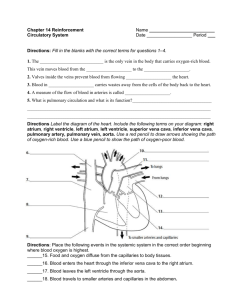
The Cardiovascular System Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Anatomy of the Heart o Heart functions: • • • • Keeps O2-poor blood separate from O2-rich blood Keeps the blood flowing in one direction Creates blood pressure Regulates the blood supply Anatomy of the Heart o • The Wall and Coverings of the Heart Pericardium • Two-layered serous membrane that encloses the heart Myocardium • Thickest part of heart wall Made of cardiac muscle Endocardium • Inner layer of heart Pericardial fluid • Reduces friction as the heart beats The coverings of the heart: Protect the heart Confine it to its location Prevent it from overfilling Fig 12.2 Anatomy of the Heart o • Chambers of the Heart Right atrium Receives O2-poor blood Vessels that empty into right atrium: • Superior vena cava Inferior vena cava Coronary sinus Venous blood leaves right atrium through the an atrioventricular (AV) valve (tricuspid) Directs the flow of blood Prevents backflow Has three cusps Right ventricle Chordae tendineae Fibrous cords connected to the tricuspid valve Blood passes through the pulmonary semilunar valve into the pulmonary trunk Anatomy of the Heart • Left atrium • Receives O2-rich blood Blood enters atrium through 4 pulmonary veins Blood leaves left atrium through an AV valve (bicuspid or mitral) Left ventricle Forms the apex of the heart Blood leaves the left ventricle through the aortic semilunar valve and enters the aorta Fig 12.3 Anatomy of the Heart o Operation of the Heart Valves • AV valves Normally open When ventricle contracts • AV valves shut Semilunar valves Normally closed Contraction of ventricles forces valves open Anatomy of the Heart o Heart Sounds • First sound, “lub” • Heard when ventricles begin to contract AV valves close Lasts longer and has a lower pitch Second sound, “dup” • When ventricles relax Semilunar valves close Heart murmurs Due to ineffective, leaky valves Valves do not close properly Allows blood to backflow into atria or ventricles after valves have closed Anatomy of the Heart o Coronary Circulation • Heart cells are not nourished by the blood in the chambers The left and right coronary arteries branch from the aorta • • • • Coronary arteries branch numerous times Heart is encircled by small blood vessels After blood passes through cardiac capillaries it enters the cardiac veins Cardiac veins enter the coronary sinus Coronary sinus enters the right atrium Fig 12.4 Physiology of the Heart o Conduction System of the Heart • • • Initiates and stimulates contraction of the atria and ventricles Is intrinsic – does not require nervous stimulation Coordinates contraction of atria and ventricles Physiology of the Heart • Nodal Tissue Has muscular and nervous characteristics SA (sinoatrial) node – upper posterior wall of the right atrium AV (atrioventricular) node – base of the right atrium Initiates the heartbeat Sends out an excitation impulse every 0.85 seconds Pacemaker of the heart Signals the ventricles to contract Atrioventricular bundle (AV bundle) Purkinje fibers Fig 12.5 Physiology of the Heart Artificial pacemaker may be implanted if the SA node fails to work properly Heart block – slow beating of the heart due to a damaged AV node Ectopic pacemaker An area other than the SA node that can become the pacemaker May cause an extra beat Caffeine and nicotine can stimulate an ectopic pacemaker Electrocardiogram Electrolyte changes within the myocardium can be detected by electrical recording devices Helps a physician detect and diagnose the cause of an irregular heartbeat (arrhythmias) Physiology of the Heart • Cardiac Cycle All events that occur during one heartbeat Systole – contraction of heart muscle Diastole – relaxation of heart muscle Three phases of the cardiac cycle: Phase 1: Atrial Systole Both atria are in systole Ventricles are in diastole Both AV valves are open The semilunar valves are closed Phase 2: Ventricular Systole Both ventricles are in systole The atria are in diastole Semilunar valves are forced open Both AV valves are closed Phase 3: Atrial and Ventricular Diastole Both atria and both ventricles are in diastole Both AV valves are open The semilunar valves are closed Fig 12.6 Physiology of the Heart • Cardiac Output (CO) Volume of blood pumped out of a ventricle in one minute Average CO is 5,250 ml/minute Dependent on two factors: Heart rate Beats per minute Can be altered by the autonomic nervous system Temperature affects the heart rate Proper electrolytes are needed to keep the heart rate regular Stroke volume Amount of blood pumped by a ventricle each time it contracts Depends on the strength of contraction Influenced by blood electrolyte concentration and the activity of the autonomic nervous system Venous return and difference in blood pressure also affect the strength of contraction Fig 12.7 Anatomy of Blood Vessels o Vessels function to: • • • • o Transport blood and its contents Carry out gas exchange Regulate blood pressure Direct blood flow Arteries and Arterioles Anatomy of Blood Vessels o Arteries and Arterioles • • Transport blood away from the heart Thick, strong walls composed of: • Tunica interna - endothelium Tunica media – smooth muscle and elastic fibers Tunica externa – outer connective tissue layer Elasticity allows an artery to expand and recoil Arterioles are small arteries • Constriction and dilation affect blood distribution and blood pressure Autonomic nervous system regulates the number of arterioles that are contracted Anatomy of Blood Vessels o Capillaries • • • • Microscopic blood vessels One layer of endothelial cells Site of nutrient and gas exchange Not all capillary beds are in use at the same time Most have a shunt Precapillary sphincters control the entrance of blood into capillaries Fig 12.9 Anatomy of Blood Vessels o • • Veins and Venules Return blood to the heart Venules Drain blood from the capillaries Join together to form veins • • Vein walls are thinner than arterial walls Valves in veins prevent backward flow of blood Varicose veins and phlebitis • Varicose veins Abnormal and irregular dilations in superficial veins Hemorrhoids are varicose veins in the rectum Develop when the valves of the veins become weak Phlebitis Inflammation of a vein Thromboembolism can occur Fig 12.8 Physiology of Circulation o Velocity of Blood Flow • Slowest in capillaries • • Cross-sectional area is at its maximum Allows time for gas and nutrient exchange Blood flow increases as venules combine to form veins Velocity of blood returning to the heart is low compared to that of blood leaving the heart Fig 12.10 Physiology of Circulation o • • • Blood Pressure The force of blood against blood vessel walls Highest in the aorta Decreases with distance from left ventricle and is lowest in the venae cavae Fluctuates between systolic blood pressure and diastolic blood pressure Mean arterial blood pressure • • Pressure in the arterial system averaged over time Equals cardiac output x peripheral resistance Increasing CO increases MABP Peripheral resistance is the resistance to flow between blood and the walls of a blood vessel The smaller the blood vessel or the longer the blood vessel the greater the resistance The greater the resistance the higher the blood pressure Fig 12.11 Physiology of Circulation • Blood pressure and cardiac output The faster the heart rate the greater the cardiac output As cardiac output increases, blood pressure increases The larger the stroke volume, the greater the blood pressure Stroke volume and heart rate increase blood pressure only if the venous return is adequate Physiology of Circulation Venous return depends on: A blood pressure difference The skeletal muscle pump and the respiratory pump Contraction of skeletal muscles compress the walls of veins causing blood to move past a valve During inhalation, thoracic pressure falls and abdominal pressure rises and blood will flow from an area of higher pressure to an area of lower pressure Total blood volume If blood volume decreases, blood pressure falls If blood volume increases, blood pressure rises Fig 12.12 Physiology of Circulation • Blood pressure and peripheral resistance Neural regulation of peripheral resistance Vasomotor center regulates vasoconstriction Also causes blood to be shunted from one area of the body to another Hormonal regulation of peripheral resistance Epinephrine and norepinephrine increase heart rate and constrict arterioles Renin-angiotensin-aldosterone system Angiotensin II constricts the arterioles Aldosterone causes the reabsorption of sodium and water in the kidneys Antidiuretic hormone causes the reabsorption of water and vasoconstriction Atrial natriuretic hormone inhibits renin and aldosterone secretion Fig 12.13 Physiology of Circulation • Evaluating circulation Pulse Alternating expansion and recoil of arterial walls Can be felt in superficial arteries (pulse points) - Radial artery - Common carotid Pulse rate normally indicates the rate of the heartbeat Fig 12.14 Physiology of Circulation Blood pressure Usually measured in brachial artery Sphygmomanometer is an instrument that records pressure changes The blood pressure cuff is inflated until no blood flows through the artery Korotkoff sounds - produced when the pressure in the cuff is released and blood begins to hit the arterial walls - Systolic pressure - When sounds end diastolic pressure is recorded Fig 12.15 Physiology of Circulation Normal blood pressure is 120/80 Higher number is systolic pressure – pressure recorded when the left ventricle contracts Lower number is diastolic pressure – pressure recorded when the left ventricle relaxes Hypertension is high blood pressure When the systolic pressure is 140 or greater When the diastolic pressure is 90 or greater Circulatory Routes o Pulmonary circuit • • • • • Blood from the body collects in the right atrium Blood moves into the right ventricle Right ventricle pumps blood into the pulmonary trunk Blood flows into the pulmonary capillaries in the lungs Blood flows from the lungs through the pulmonary veins and into the left atrium Circulatory Routes o Congestive Heart Failure • Damaged left side of the heart fails to pump adequate blood Blood backs up in the pulmonary circuit • • Pulmonary blood vessels have become congested Causes pulmonary edema Indicated by shortness of breath, fatigue, and a constant cough Treatment • Diuretics – increase urinary output Digoxin – increases the heart’s contractile force Dilators – relax blood vessels Circulatory Routes o Systemic circuit • Includes all other arteries and veins of the body Aorta and venae cavae are the major pathways for blood in the systemic circuit • • • • Aorta is the largest artery Superior and inferior venae cavae are the largest veins Begins in the left ventricle The left ventricle pumps blood into the aorta Branches from the aorta go to the major body regions and organs Circulatory Routes Table 12.1 Fig 12.16 Circulatory Routes Table 12.2 Fig 12.17 Circulatory Routes o Special Systemic Circulations • Hepatic Portal System Carries venous blood from the stomach, intestines, and other organs to the liver Capillaries of the digestive tract empty into the superior mesenteric and the splenic veins Superior mesenteric and splenic vein join to form the hepatic portal vein Gastric veins empty into the hepatic portal vein Nutrients and wastes diffuse into liver cells The hepatic veins drain the liver and enter the inferior vena cava Fig 12.18 Circulatory Routes • Hypothalamus-Hypophyseal Portal System Blood Supply to the Brain • Anterior and posterior cerebral arteries and the carotid arteries supply the brain with arterial blood Cerebral arterial circle (circle of Willis) The blood vessels form a circle Provides alternate routes for supplying arterial blood to the brain Equalizes blood pressure in the brain’s blood supply Fig 12.19 Circulatory Routes • Fetal Circulation Four circulatory features not present in adult circulation Foramen ovale Ductus arteriosus Umbilical arteries Ductus venosus Related to the fact that the fetus does not use its lungs Path of blood in the fetus From the right atrium Most blood enters the left atrium via the foramen ovale Blood that has entered the right ventricle and then the pulmonary trunk is shunted to the aorta through the ductus arteriosus Exchange between maternal and fetal blood occurs at the placenta Blood in the umbilical arteries is oxygen poor Blood in the umbilical veins is oxygen rich Enters the ductus venosus The ductus venosus then joins with the inferior vena cava Fig 12.20 Effects of Aging o Heart • • • • • • Grows larger with age In many middle-aged people, heart is covered by a layer of fat Number of collagenous fibers in the endocardium increases Valves become thicker and more rigid The myocardium loses contractile power and ability to relax Resting heart rate decrease Effects of Aging o Arteries • Atherosclerosis and arteriosclerosis are common Chances of coronary thrombosis and heart attack increase Occurrence of varicose veins increases • • Thromboembolism Pulmonary embolism Homeostasis o Maintaining blood composition, pH, and temperature • • • • • • Growth factors regulate the manufacture of formed elements in the red bone marrow The digestive system absorbs nutrients into the blood The lungs and kidneys remove metabolic wastes from the blood The kidneys help maintain the pH of blood The blood distributes heat Blood vessels in the skin dilate or constrict in response to changing temperatures Homeostasis o Maintaining blood pressure • • • • Sensory receptors within the aortic arch detect a decrease in blood pressure The lymphatic system collects excess tissue fluid, which helps regulate blood volume and pressure The endocrine and nervous systems work together to regulate blood pressure Venous return is aided by the muscular and respiratory systems