Lecture 4
advertisement

31:241 Behavioral and Cognitive Neuroscience
Professor A.K. Johnson
Fall 2012
Outline
Reward and Addiction
10/30; 11/1
I.
Introduction
II.
Neural and Neurochemical Bases of Reward and Action
A.
Discovery of rewarding electrical brain stimulation (self-stimulation)
B.
Rewarding brain stimulation and conventional motivation and reward
C.
A punishment system
D.
Theories of self-stimulation
E.
Neural and neurochemical substrates of self-stimulation
F.
Dopamine systems
G.
The relationship between self-stimulation and drug self-administration (i.e., drugs which act as reinforcers)
H.
Conditioned place preference: use for assessing reinforcing properties of drugs
I.
Neural substrates of drug addiction
J.
Neurochemistry and neuropharmacology of reward systems
K.
Relation of motivation and reward systems to motor pathways: from motivation to action
III. Overview of Drug Abuse, Addition and Dependence
A.
Definitions
B.
Toxicity of drugs of abuse
C.
Origins of abuse and dependence
D.
DSM-IV and ICD-10 criteria
E.
Variables associated with abuse and addiction
F.
Theories of addiction
IV. Treatments for Drug Dependence
A.
Detoxification
B.
Maintenance of abstinence
C.
Strategies and therapeutics
241-4.0
Key Terms and Concepts
Abstinence syndrome
Dependence
Depressant (neural depressant)
Dorsal mesostriatal (nigrostriatal)
Drug abuse
Drug sensitization
Drug tolerance
Mesocortical
Mesolimbic
Naloxone
Nigrostriatal
Sensitization
Stimulants
Tolerance
Ventral mesostriatal (mesolimbic)
Ventral pallidum
241-4 KTC
Operant Chamber (Skinner Box)
for Delivery of Rewarding Electrical
Brain Stimulation (Self-Stimulation)
241-4.1
A Cumulative Bar-Pressing Curve for a Self-Stimulating
Rat With an Electrode in a Positive Reward Site
241-4.2
The Relationship Between Self-Stimulation and
Conventional Motivated Behaviors and Reward
• Performance on instrumental tasks
- Reward magnitude
- Priming
- Rapid extinction
- Schedules of reinforcement
- Chaining of behaviors
- Secondary reinforcers
• Electrically elicited behaviors (drinking, eating,
chewing, hoarding, aggressive reproductive
responses)
• Aversion/punishment systems
241-4.3
Some Sites Which Support Intracranial SelfStimulation in Various Animal Species
Brain Area
Sites Which Support Self-Stimulation
Forebrain
Frontal cortex;
Olfactory nucleus;
Nucleus accumbens;
Septal area;
Amygdaloid nucleus;
Hypothalamus
Entorhinal cortex;
Caudate nucleus;
Entopeduncular nucleus;
Hippocampus;
Ventral and medial thalamus;
Median forebrain bundle;
Dorsal noradrenergic bundle
Midbrain and
brain stem
Ventral tegmental area; Substantia nigra;
Raphe nuclei;
Nucleus coeruleus;
Superior cerebellar
Periaqueductal gray matter
peduncle;
Mesencephalic nucleus
of trigeminal nerve
Cerebellum
Deep cerebellar nuclei
Medulla
Motor nucleus of
trigeminal nerve;
Nucleus of tractus solitarius
Other cerebellar areas
241-4.4
Neuroanatomy of Brain Reward
and Punishment Systems
241-4.5
Theories of Self-Stimulation
• Automatistic behavior
• Hedonic (Olds)
• Dual activation of drive and reward pathways
(Deutsch; Gallistel)
• Consummatory behavior (Glickman & Schiff)
• Incentive motivation (Trowill, Panksepp &
Gandelman)
241-4.6
Lines of Evidence Supporting the Idea that Catecholamines
(CAs) Mediate Rewarding Brain Stimulation
Larry Stein
(Circa 1966)
•
•
•
•
Drugs that facilitate self-stimulation release CAs (e.g., amphetamine).
Drugs that inhibit self-stimulation deplete CAs (reserpine, -methyl-ptyrosine).
Drugs that block adrenergic transmission (chlorpromazine) inhibit
self-stimulation.
Protection of CAs with monoamine oxidase inhibitors or block reuptake
(e.g., imipramine) enhances the facilitatory effect of amphetamine on
self-stimulation.
•
Depletion of brain CAs with reserpine or -methyl-p-tyrosine decreases
the facilitatory effects of amphetamine on self-stimulation.
•
A large component of the medial forebrain bundle (MFB), a “hot-spot” for
self-stimulation, is catecholaminergic.
•
Rewarding stimulation of the MFB causes release of norepinephrine into
the amygdala and hypothalamus.
241-4.7
Horizontal and Lateral Representations of Ascending
Noradrenaline and Dopamine Pathways
241-4.8
Dopaminergic Pathways in the Rat Brain
241-4.9
The Four Major DA Pathways in the Brain
241-4.10
Brain Dopamine Systems
Ultrashort
•
•
Retina – interplexiform amacrine-like neurons
Olfactory bulb – periglomerular dopamine cells
Intermediate Length
•
•
•
Tuberohypophyseal
Incertohypothalamus
Medullary periventricular
Long Length
•
•
•
Nigrostriatal
Mesolimbic
Mesocortical
241-4.11
The Dopamine Synapse
241-4.12
Six Types of Postsynaptic Dopamine Receptors
D1 and D5
D2a
D2b
D3 and D4
Molecular structure
Seven membranespanning regions
Seven membranespanning regions
Seven membranespanning regions
Seven membranespanning regions
Effect on cyclic AMP
Increases
Decreases
Increases phosphoinositide turnover
?
Agonists
Dopamine
Apomorphine
Full agonist (weak)
Partial agonist (weak)
Full agonist (potent)
Full agonist (potent)
Antagonists
Phenothiazines
Thioxanthenes
Butyrophenones
Clozapine
Potent
Potent
Weak
Inactive
Potent
Potent
Potent
Weak
Weak
Potent
241-4.13
The Rotometer
241-4.14
Investigation of the Actions of
Dopamine in the Nigrostriatal System:
Drug-Induced Rotational Behavior in Rats
with Unilateral Nigrostriatal Lesions
241-4.15
Some Prototypic Dopamine Agonists and Antagonists
Drug
Presumed Mechanism
of Action
Antagonists
Butyrophenones
Haloperidol
Phenothiazines
Receptor blockade
Chlorpromazine*
Agonists
Apomorphine
Receptor stimulation
Bromocriptine
Releasers
Amphetamine
Releaser
Vesicular Storage Inhibitors
Reserpine*
Depletion
Pump Inhibitors
Cocaine
Reuptake inhibition
Synthesis Inhibitors
Carbidopa
Dopa decarboxylase inhibition
-Methyl-p-tyrosine*
Tyrosine hydroxylase inhibition
Monoamine Oxidase Inhibitors
Iproniazid*
Broad-spectrum MAO inhibition
COMT Inhibitors
Tropolone, pyrogallol*,
COMT inhibition
rutin, quercetin
False Transmitters
-Methyldopamine*
Toxin
6-Hydroxydopamine*
Destruction of cells
Precursors
Dopa
Stimulates transmitter production
*Also has prominent norepinephrine or epinephrine action, or both
Most Prominent
Physiological Effects
Tranquilizer; antipsychotic; antinauseant
Antiparkinsonian, emetic
Stimulant, appetite suppressant
Antihypertensive; tranquilizer;
antipsychotic
Stimulant euphoriant
Adjuvant for central dopa
Depressant; akinesia
Antidepressant
Minimal effects
Antihypertensive
Experimental
Antiparkinsonism and mild stimulant
241-4.16
The Medial Forebrain Bundle is One of the
"Hottest" Brain Pathways for Self-Stimulation
241-4.17
Blockade of Medial Forebrain Bundle SelfStimulation by Dopamine Receptor Antagonist
Infused Into the Nucleus Accumbens
241-4.18
Effects of Electrical Self-Stimulation
of the Ventral Tegmental Area on Extracellular
Dopamine in the Nucleus Accumbens
241-4.19
Apparatus for Producing and
Measuring a Conditioned Place Preference
241-4.20
Place Conditioning With Dopamine Agonists
Infused Into the Nucleus Accumbens
241-4.21
Intravenous Self-Administration of Drugs of Abuse
241-4.22
Some Drugs Which Act as
Reinforcers* in Animal Species
Alcohol
Amphetamines
Apomorphine
Barbiturates
Benzodiazepines
Chlorphentermine
Chloroform
Clortermine
Cocaine
Codeine
Diethylpropion
Ether
Lacquer, thinners
Marijuana
Methadone
Methyl phenidate
Morphine
Nicotine
Nitrous oxide
Pentazocine
Phencyclidine
Phenmetrazine
Pipradrol
Procaine
Propiram
Propoxyphene
*Animals will voluntarily self-administer these drugs after suitable
priming, depending on dose, schedule, route of administration, and
species. Routes of administration include: intravenous,
intramuscular, inhalation, intracerebral, intragastric tube, and oral.
Animal species include: rat, monkey, ape, baboon, dog, and others.
241-4.23
Mediation of the Rewarding Effects of Drugs of Abuse
by Dopamine (DA) Action in the Nucleus Accumbens
241-4.24
Hypothesized Sites of Action of Drugs
on Brain-Reward Circuitry in the Rat
241-4.25
Changes in Dopamine Detected in the Extracellular
Fluid of the Nucleus Accumbens of Rats After Daily
Intraperitoneal Cocaine Injections (10 mg/kg)
241-4.26
Tetrahydrocannabinol (THC)-Induced Enhancement
of Dopamine Efflux in the Nucleus Accumbens
241-4.27
Two Systems Responsible for the
Initiation of Movements (Actions):
Limbic Structures
Cerebral Cortex
Caudate N.
(Neostriatum)
N. Accumbens
(Ventral Striatum)
Globus Pallidus
One Involves Cognitive Processes and the Other Involves Those
in Response to Basic Motivations (Drives) and Emotions
DA
A10
VTA
Motor
System
241-4.28
Locomotion Occurs When Inhibitory
GABA-Secreting Synapses on Neurons
in the Globus Pallidus Decrease Their Activity
241-4.29
The Motive Circuit "Translates" the
Perception of a Reward Into Locomotion
241-4.30
Simplified Diagram of Central
Pathways Controlling Locomotion
Thalamus
Mesencephalic Locomotor Region
(Pedunculo Pontine Nucleus)
N. Accumbens
(Ventral Striatum)
Globus Pallidus
Limbic Structures
Cerebral Cortex
Caudate N.
(Neostriatum)
NRP
NRP
Spinal
Pattern
Generator
Ventromedial
Medulla
Motor
System
VTA
VTA, ventral tegmental area; NRG, nucleus reticularis gigantocellularis; NRP, nucleus reticularis pontis oralis
241-4.31
Drug Dependence and Abuse
Drug Abuse = a maladaptive pattern of substance use
manifested by recurrent and significant adverse
consequences to repeated use of substances.
Dependence
•
•
•
•
•
Drug dependence is a state whereby an individual either
psychologically or physically requires a drug in order to
feel well in the absence of medical indications.
Discontinuation of the drug will produce a characteristic
group of withdrawal symptoms.
Physiological dependence = adverse physiological
reactions (e.g., stomach cramps) in the absence of drugs.
Primary psychological dependence = produces pleasure
and/or reduces "psychic" discomfort (drug craving).
Secondary psychological dependence = fear or anxiety as
a result of a lack of drug.
241-4.32
Drug Addiction = Substance Dependence
1. Compulsion to seek and take a drug.
2. Loss of control in limiting intake.
3. Emergence of negative emotional state (e.g.,
dysphoria, anxiety, irritability) when access to
drug is prevented.
4. Chronic relapsing disorder.
241-4.33
Categories of Drugs of Abuse
Opiates and Opioids
• Morphine, codeine, heroin, meperidine, hydromorphone,
and other opioid agonists
Stimulants
•
Cocaine, amphetamines, methylphenidate, nicotine,
caffeine
Depressants
• Barbiturates, non-barbiturate sedatives, benzodiazepines,
and ethanol
Hallucinogens
•
D-lysergic
acid diethylamide (LSD), mescaline,
methylenedioxymethamphetamine (MDMA),
phencyclidine, marijuana
Inhalants
241-4.34
Classification of Drug Use
1. Occasional, controlled, social use
2. Abuse or harmful use
3. Addiction
241-4.35
Drug Use, Abuse and Dependence
in U.S. Adults
At Some Point in Their Lifespan
• 15.6% engage in illicit drug use
• 3.1% engage in abuse
• 2.9% develop dependence
241-4.36
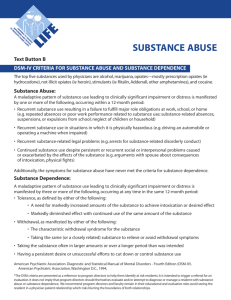
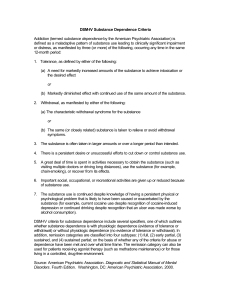
DSM-IV and ICS-10 Diagnostic Criteria for
Alcohol and Drug Abuse/Harmful Use
DSM-IV Alcohol and Drug Abuse
A. A maladaptive pattern of substance use leading to clinically significant impairment or
distress, as manifested by one (or more) of the following, occurring within a 12 month
period:
1.
Recurrent substance use resulting in a failure to fulfill major role obligations at
work, school, or home.
2.
Recurrent substance use in situations in which it is physically hazardous.
3.
Recurrent substance-related legal problems.
4.
Continued substance use despite having persistent or recurrent social or
interpersonal problems caused or exacerbated by the effects of the drug.
B. The symptoms have never met the criteria for substance dependence for this class of
substances.
ICD-10 Harmful Use of Alcohol and Drugs
A. A pattern of substance use that is causing damage to health. The damage may be
physical or mental. The diagnosis requires that actual damage should have been
caused to the mental or physical health of the user.
B. No concurrent diagnosis of the substance dependence syndrome for same class of
substance.
241-4.37
DSM-IV and ICD-10 Diagnostic Criteria for
Alcohol and Drug Dependence
241-4.38
Stages of Drug Addiction/Dependence
241-4.39
Diagnostic Criteria of Addiction
• Shift in emphasis in diagnostic criteria from focus on
tolerance and withdrawal to criteria related to
compulsive use.
• Diagnostic and Statistical Manual of Mental Disorders =
DSM-IV (American Psychiatric Association)
• International Statistical Classification of Diseases and
Related Health Problems = ICD-I0 (World Health
Organization)
241-4.40
Origins of Abuse and Dependence
• Drugs that affect behavior are likely to be taken in excess
when the effects are considered pleasurable.
• Legal prescription drugs (e.g., barbiturates, morphine,
amphetamine), illegal drugs (e.g., heroin and cocaine) and
non-prescription drugs (e.g., ethanol and nicotine) are
abused and can produce dependence.
• Very few individuals begin addiction problems by misuse of
prescription drugs.
• However, prescribed medications for pain, anxiety and even
hypertension commonly produce tolerance and physical
dependence.
• Tolerance and physical dependence do not imply abuse or
addiction.
241-4.41
Vulnerability to Addiction
Individual Differences:
• Temperament
--Disinhibition
--Negative affect
--Novelty/sensation seeking
• Social Development
--Early drug/alcohol exposure
• Co-morbidity
--Mood disorders
--Anxiety disorders
--Antisocial personality disorder
--Conduct disorders
• Genetics
--Contributes to ~40% of total variability associated with drug dependence
• Protective Factors
--Also receives contributions from genetics, personality, and environment
241-4.42
Abstinence Syndrome
• Physiological and psychological dependencerelated symptoms and signs that arise during
withdrawal of a drug.
- Relationship with ½ life of drug.
241-4.43
Relationship Between the Intensity of a Drug's Effects
and the Intensity of the Abstinence Syndrome
241-4.44
Differences in Responses
to Heroin and Methadone
241-4.45
Medical/Psychological Views of Addiction
1. Dependence ('40's)
--Physical dependence the sine qua non of the abstinence syndrome
--Evolved to include "psychic" (psychological) dependence
--Drug craving
2. Psychiatric
--Addiction has aspect of impulse control disorders and compulsive disorders
--Impulsive acts preceded by tension or arousal followed by pleasure gratification or relief
--Compulsive acts preceded by anxiety and stress followed by relief from stress
--Addiction considered to shift from an impulsive disorder to a compulsive disorder
--A circle of addiction with 3 stages: preoccupation/anticipation → binge/intoxication →
withdrawal/negative affect
3. Psychodynamic
--Focuses on developmental difficulties, emotional disturbances, structural (ego) factors,
personality organization and building of the self
--Associated with a self-medication hypothesis where users are considered to take drugs to cope
with painful/threatening emotions
--Opiates for anger and rage
--Psychostimulants for anhedonia, anergia, and lack of feelings
--Neurodepressants for those flooded by or cut off from feelings
--Each drug class serves as an antidote for a dysphoric condition or state
4. Social Psychological/Self-Regulation
--Failure in self-regulation leads to addiction
--Initial lapse in self-regulation leads to large-scale breeder claims in self-regulation due to
emotional distress
--Each successive lapse brings greater distress and a downward spiral ensues
--View can be related to neural processing concepts involving frontal lobe dysfunction
241-4.46
Diagram Representing a Psychiatric View of the
Transition of a Problem of Impulse Control to a Problem
of Compulsion in the Course of Becoming Addicted and
the Nature of Reinforcement (Positive to Negative)
241-4.47
Primary Goal of Neurobiological
Addiction Research:
To Understand the Neuropharmacological and
Neuroadaptive/Neuroplastic Mechanisms Within the
neurocircuitry mediating the transition between
occasional drug use and the loss of control over drug
seeking and taking (i.e., addiction).
241-4.48
Major Issues for a Comprehensive
Understanding of Drug Addiction
• Reward mechanisms
• Changes in response to the drug
(sensitization or tolerance)
• Drug craving
• Causes for relapse
241-4.49
Neuroadaptation Views of Addiction
1. Behavioral Sensitization
Berridge & Robinson
Conceptually tied to psychomotor sensitization
Incentive sensitization
Liking and wanting
Incentive-salience
--Cues associated with drug cues and drug taking become associated through Pavlovian stimulus
associative conditioning to enhance motivation
2. Opponent-Process or Counteradaptation Theory
Contributors used such theories to account for tolerance and withdrawal:
Himmelsbach ('40's)
Martin ('60's)
Solomon & Corbit ('70's)
Koob & Bloom ('80's)
--Theorized that the brain uses negative feedback mechanisms to keep affective responses in check
--An unconditioned "a" process (positive/pleasurable) is counteracted by a "b" process
--The "b" process has a larger latency of onset and duration of action
--"b" process grows disproportionally compared to the decreasing "a" process and is associated with an
aversive craving state
--Solomon argues that the 'b" process "grows" with repeated drug taking
3. Motivational
--Drug addicts frequently report that there is minimal pleasure derived from the drug although the
craving is great
--The threshold for reward becomes elevated when drug is administered
--Can be demonstrated by showing that ICSS thresholds are elevated by cocaine administration
4. Plasticity in Second Messenger and Immediate Early Gene Response Systems
5. Allostasis
Allostasis = maintaining apparent reward function stability through changes in brain reward mechanisms
Koob & Le Moal Propose: that not only does the opponent-process "b" change with repeated drug
consumption but that the drug-reward "set point" also changes
241-4.50
Robinson and Berridge's Theory
of Incentive Salience and Drug Addiction
• Administration of some classes of abused
drugs (e.g., psychostimulants) produce
sensitization (i.e., reverse tolerance).
• For example, psychomotor stimulants
increase locomotor behavior with spaced,
repeated administration in a normal
environment.
• Robinson and Berridge propose that
increased drug craving is the produce of a
similar sensitization process where "wanting"
the drug is enhanced.
241-4.51
Berridge and Robinson's Model Focusing on the
Role of Incentive Salience as a Factor Related to
Drug Craving and In Turn Relapse
241-4.52
The Opponent-Process Theory
of Motivation and Emotion
241-4.53
Koob and Le Moal's Application of
Opponent-Process Theory to Phenomenology
Associated with Drug Addiction
241-4.54
Koob and Le Moal's Diagram of the
Hypothetical Spiraling Distress-Addiction
From a Neurobiological Perspective
241-4.55
Nestler's Theory of Sensitization as a
Result of Drugs that Release Dopamine
Causing Increased Fos-Related Antigens (Fra)
241-4.56
Behavioral and Cellular/Molecular Changes
Associated with Drug Use, Addiction,
Withdrawal and Long-Term Abstinence
241-4.57
Treatment for Drug Dependence
• Will vary with the drug being used and social and
cultural factors determining the use.
• The management of withdrawal syndromes can be
achieved with minimal risk and high probability of
success using pharmacological agents.
241-4.58
Detoxification: Withdrawal of Opioids
•
Most patients will perceive withdrawal symptoms.
•
May be possible to reduce the drug.
•
Methadone is suitable for suppressing withdrawal symptoms.
•
•
•
•
With methadone substitution in an in-patient setting, symptoms
usually aren't worse than "flu-like" syndrome.
Under these "drug weaning" conditions, most patients can be
withdrawn in less than 10 days.
Clonidine (2-adrenergic receptor agonist) can suppress some
components of opioid withdrawal.
Clonidine suppresses autonomic signs and symptoms (e.g.,
nausea, vomiting, diarrhea) then drug craving.
241-4.59
Withdrawal of Neurodepressants
• Abrupt neurodepressant withdrawal can be fatal.
• Pentobarbital can be substituted for any
neurodepressant.
• Pentobarbital is administered to induce mild
intoxication and maintained 24 to 36 hrs and
stabilized, then withdrawal can be started.
241-4.60
Role of Pharmacological
Agents Following Withdrawal
• Therapeutics may be used to treat underlying
psychological problem (e.g., anxiety or
depression).
• Therapeutic agents intended to be a less toxic
substitute (e.g., methadone) may be used.
• Drugs to interfere with reinforcing actions of the
abused drug (e.g., naltrexone).
241-4.61
Pharmacological Approach to
Cocaine and Amphetamine Dependence
• Most consistent pharmacotherapy has been
obtained with tricyclic antidepressants (e.g.,
desipramine).
• After 1 to 2 weeks, desipramine appears to reduce
craving for cocaine.
• It is postulated that the antidepressants increase
functional activity in reward systems by altering
cocaine-induced supersensitivity at dopamine
autoreceptors.
241-4.62
Drugs of Abuse and How Their Effects
Might Theoretically Be Treated
Mechanism
Involved
Main Neurotransmitter
Affected
Potential Treatment
Action on endogenous receptors for endogenous ligands
Opioids
Endorphins, enkephalins
Alcohol
GABA, endorphins
Benzodiazepines &
barbiturates
Nicotine
Cannabinoids
LSD and related
hallucinogens
GABA
Acetylcholine
? Anandamide
5-HT
Partial agonist (e.g., buprenorphine)
Antagonists (e.g., naltrexone)
Partial agonists (e.g., bretazenil)
Opiate antagonists (e.g., naltrexone)
Partial agonists (e.g., bretazenil
Antagonists (e.g., flumazenil)
Antagonists (? mecamylamine)
Antagonists (e.g., SR 141716A)
5-HT2 receptor antagonists
(e.g., ritanserin)
Increasing the release of endogenous neurotransmitters
Cocaine
Dopamine
Solvents
? Noradrenaline
D2 receptor antagonist*
Antagonist of the uptake site
(e.g., SSRI)
? Receptor antagonists
Antagonizing the action of natural transmitters
Alcohol
Glutamate
NMDA antagonists (e.g., dizocilpine)
*Most typical (e.g., haloperidol) and atypical (e.g., sulpiride, tiapride, risperidone)
neuroleptics have a high affinity for D2 receptors.
241-4.63
Pharmacotherapy for Drug
Abuse Relapse Prevention
Drug
• Natrexone (Trexan) – opioid and alcohol
dependency
• Disulfiram (Antabuse) – alcohol dependency
• Clonidine (Catapres) – opioid withdrawal
• Methadone (Dolophine) – opioid dependency
• Buprenorphine (Buprenex) – opioid dependency
• Nicotine – patches and gum
• Ibogaine (Endabuse) - anticraving
• Acamprosate – anti-alcohol craving
• Immunization (experimental animals)
- Morphine
- Cocaine
241-4.64
Modification of Behavior After Withdrawal
Psychotherapy
• Little evidence that traditional individual
psychotherapy is of value for compulsive drug user.
• Cognitive or expressive psychotherapy has improved
poor prognosis patients in methadone programs.
• Special forms of group therapy and self-help groups
have been demonstrated to reduce relapse.
Voluntary Groups and Self-Regulatory Communities
• Alcoholic anonymous, narcotics anonymous, Phoenix
House, etc.
Supervised-Deterrent Approaches
• Abstinence during a period in a hospital, prison, or
special facility followed by supervision in the
community.
241-4.65